
Am Fam Physician. 2014;89(3):193-198
A more recent article on adolescent idiopathic scoliosis is available.
Patient information: A handout on this topic is available at https://familydoctor.org/familydoctor/en/diseases-conditions/scoliosis.html.
Adolescent idiopathic scoliosis is the most common form of scoliosis, affecting approximately 2% to 4% of adolescents. The incidence of scoliosis is about the same in males and females; however, females have up to a 10-fold greater risk of curve progression. Although most youths with scoliosis will not develop clinical symptoms, scoliosis can progress to rib deformity and respiratory compromise, and can cause significant cosmetic problems and emotional distress for some patients. For decades, scoliosis screenings were a routine part of school physical examinations in adolescents. The U.S. Preventive Services Task Force and American Academy of Family Physicians recommend against routine scoliosis screening in asymptomatic adolescents, concluding that harm from screening outweighs the benefit because screenings expose many low-risk adolescents to unnecessary radiographs and referrals. In contrast, the Scoliosis Research Society, American Academy of Orthopaedic Surgeons, American Academy of Pediatrics, and Pediatric Orthopaedic Society of North America suggest that the potential benefit of detecting scoliosis early justifies screening programs, but greater care should be used in deciding which patients with positive screening results need further evaluation. The goal for primary care physicians is to identify patients who are at risk of developing problems from scoliosis, without overtesting or overreferring patients who are unlikely to have further problems. Physical examination with the Adam's forward bend test and a scoliometer measurement can guide judicious use of radiologic testing for Cobb angle measurement and orthopedic referrals. Treatment options include observation, braces, and surgery.
Scoliosis is a condition commonly encountered in the primary care setting, affecting roughly 2% to 4% of adolescents.1–4 Scoliosis is defined as a lateral curve to the spine that is greater than 10 degrees with vertebral rotation.1–5 It can be classified as congenital, neuromuscular, or idiopathic; approximately 85% of cases are idiopathic.1–3,6 Idiopathic scoliosis can be further classified by age of onset: infantile (birth to two years), juvenile (three to nine years), and adolescent (10 years and older).1–3,6 Adolescent idiopathic scoliosis is the most common form.1–3,6,7 Scoliosis usually does not cause problems, but sometimes leads to visible deformity, emotional distress, and respiratory impairment from rib deformity.1,3–5,7–9
Males and females are about equally likely to have minor scoliosis of approximately 10 degrees, but females are five to 10 times more likely to progress to more severe disease, possibly needing treatment.1,3–5,10,11 The goal for primary care physicians is to first determine which patients have significant spinal curvature, then decide which of these patients may need imaging or referral for treatment.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The U.S. Preventive Services Task Force and the American Academy of Family Physicians recommend against routine scoliosis screening in asymptomatic adolescents. | B | 14, 15 |
| A scoliometer measurement of less than 5 degrees likely does not require follow-up. | C | 5, 8, 20 |
| A scoliometer measurement of 10 degrees or greater requires radiologic evaluation for Cobb angle measurement. | C | 5, 8, 20 |
Etiology
The exact pathophysiologic mechanism for scoliosis is unknown. A genetic factor has been implicated in the development and progression of scoliosis.3,12 If both parents have idiopathic scoliosis, their children are 50 times more likely to require scoliosis treatment compared with the general population.2 Scoliosis is believed to be a polygenic disorder with multiple inheritance patterns.12 Saliva-based genetic markers could be a useful adjunct in predicting which patients are at risk of scoliosis progression.12 However, further studies are needed, and genetic testing is not recommended at this time.
Screening
For decades, scoliosis screenings were a routine part of school physical examinations in adolescents.13 The screening itself carries little cost and negligible risk to the patient, but radiographs and referrals in youths who may be at low risk of disease progression can lead to significant expense and risk of harm to patients.14,15
The U.S. Preventive Services Task Force (USPSTF) did not find good evidence that screening in asymptomatic adolescents detects idiopathic scoliosis at an earlier stage than no screening. It also found fair evidence that treating adolescent idiopathic scoliosis decreases pain and disability in only a small proportion of patients, and that treatment of adolescent idiopathic scoliosis detected through screening leads to moderate harms (e.g., unnecessary use of braces and referral). The accuracy of the most common screening test, the Adam's forward bend test, with or without a scoliometer, is variable. The USPSTF found that most cases detected through screening do not progress to clinically significant scoliosis, and scoliosis requiring surgery is likely to be detected without screening.15
In a prospective study in the Netherlands that followed more than 30,000 students 10 to 14 years of age for up to three years, annual scoliosis screening in addition to the usual biennial health checkup detected no cases of idiopathic scoliosis requiring surgery, and the authors concluded that additional annual scoliosis screening was not needed.15 Based on these findings, in 2004 the USPSTF concluded that the harms of screening asymptomatic adolescents for idiopathic scoliosis exceeded the potential benefits.14,15 The American Academy of Family Physicians concurs in recommending against routine screening.16–18
The Scoliosis Research Society, American Academy of Orthopaedic Surgeons, American Academy of Pediatrics, and Pediatric Orthopaedic Society of North America convened a task force in 2007 supporting scoliosis screening, while also recognizing the need for greater care in deciding which patients with positive screening results need further evaluation.19 These groups argue that the cost of scoliosis screening is relatively low, and that the radiation exposure with current radiographic techniques is significantly less than in the past. They list prevention of deformity progression with brace treatment and earlier recognition of severe deformities requiring surgery as potential benefits of screening.
The challenge for the primary care physician is differentiating adolescents with higher-risk scoliosis requiring referral or intervention from those with lower-risk scoliosis requiring observation and no intervention. The USPSTF suggests that most patients who need treatment will be detected without screening,14 when presenting with visible curvature or possibly incidentally during another type of examination.
Physical Examination
Physical examination for scoliosis mainly consists of the Adam's forward bend test (Figure 1).3 The patient stands and bends forward at the waist, with the examiner assessing for symmetry of the back from behind and beside the patient.1,3,4,20 Patients with possible scoliosis will have a lateral bending of the spine, but the curve will cause spinal rotation and eventually a rib hump, which is visible on examination.3,4
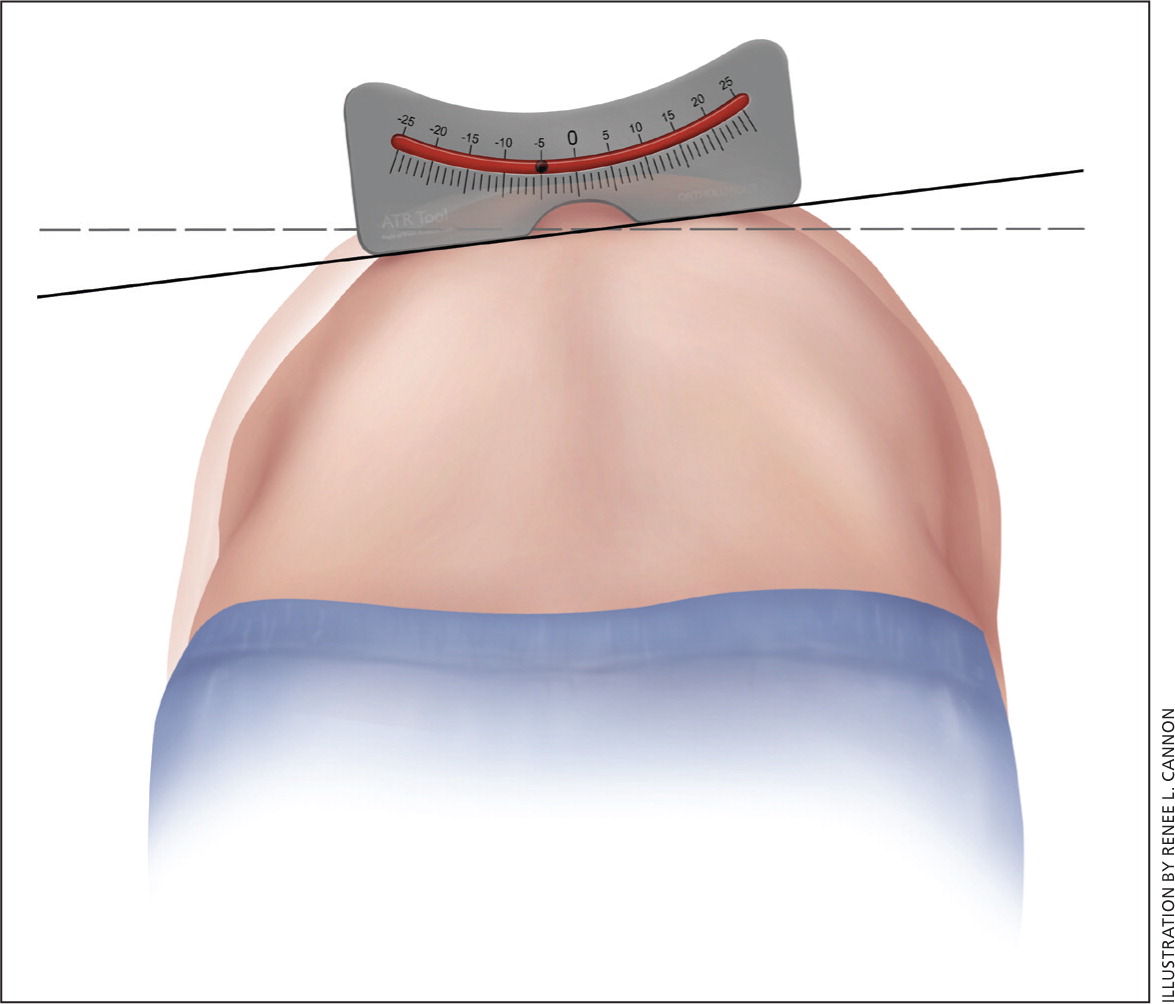
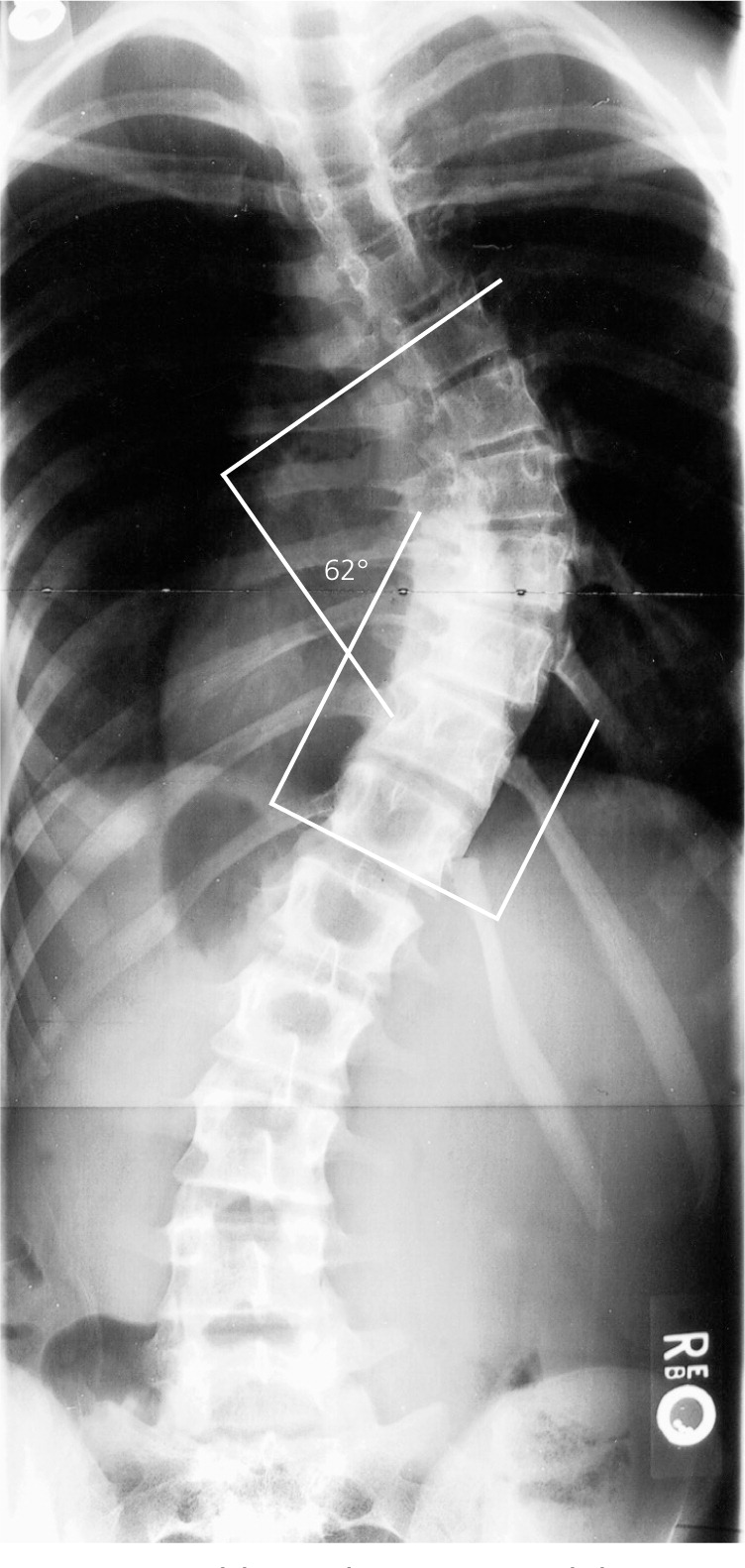
The examiner may then attempt to quantify the spinal curve and rotation with a scoliometer, or inclinometer4,5 (Figure 2). The inclination angle measured by a scoliometer will help determine which patients may need radiography. The estimated magnitude of the spinal curve can be used to determine the angle of trunk rotation.4,5 This can help avoid imaging in patients with clearly insignificant curves; however, a Cobb angle measurement using radiography is needed for the official diagnosis of scoliosis.1–6,10 Generally, an angle of trunk rotation that is less than 5 degrees is insignificant and may not require follow-up.4,5 A measurement of 5 to 9 degrees at least warrants reexamination in six months.5,20 A measurement of 10 degrees or greater requires radiologic evaluation for Cobb angle measurement,5,8,20 shown in Figure 3.3
Red Flags
Although scoliosis is usually benign and rarely requires treatment, there are several characteristics that suggest more serious problems and a diagnosis of nonidiopathic scoliosis. Approximately 85% to 90% of adolescent idiopathic scoliosis cases involve a right thoracic curve (the spinal curve is convex to the right).3,6,7 A left thoracic curve (convex to the left) is more likely to be associated with additional pathology, including spinal cord tumors, neuromuscular disorders, Arnold-Chiari malformations, or occult syrinx.3,6
Risk Factors for Disease Progression
Three major factors that determine whether scoliosis will progress are patient sex, magnitude of curve on presentation, and growth potential.3,5,10,11 One study followed 186 skeletally immature patients with idiopathic scoliosis, diagnosed through school screening, until skeletal maturity. The initial Cobb angle magnitude was the most important predictor of long-term curve progression and behavior past skeletal maturity, whereas initial age, sex, age of menarche, and pubertal status were less important prognostic factors. The authors suggested an initial Cobb angle of 25 degrees as an important threshold magnitude for long-term curve progression.10
The examiner may estimate growth potential based on age and Tanner stage; however, for more precise determination of growth potential, radiographs may be needed to measure the Risser grade. The Risser grade measures bony fusion of the iliac apophysis (Figure 421 ), with higher Risser grades indicating greater skeletal ossification, hence less potential for growth and curve progression.1,3–7,11 The time of greatest curve change is in early adolescence (curve acceleration phase). Progression of scoliosis curve averages 0.2 degrees per month before the curve acceleration phase, although curves could change 1 to 2 degrees per month at the start of this phase.22
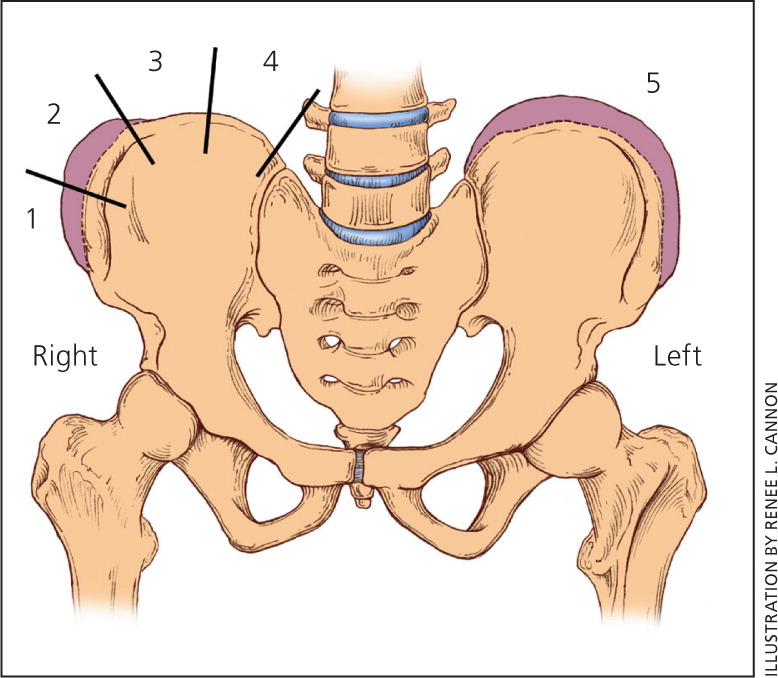
The Tanner-Whitehouse 3 assessments, which assess skeletal maturity based on radiographic evaluation of the epiphyses of the distal radius, distal ulna, and small hand bones, were simplified and used to create a skeletal scoring system to estimate scoliosis behavior.21 The researchers eliminated the radial and ulnar radiographic scores to produce a digital skeletal age score, which correlates with the curve acceleration phase. Table 1 shows predictions of scoliosis progressing to a 50-degree curve, with its potential for surgical treatment, based on digital skeletal age staging and curvature at the time of the measurement.11 The simplified Tanner-Whitehouse 3 skeletal maturity assessment goes up to stage 8, which corresponds to Risser grade 5. Many patients could be stage 5 on the simplified Tanner-Whitehouse 3 scale, but be a Risser grade 0. Therefore, the prediction of scoliosis activity may be stronger with the simplified Tanner-Whitehouse 3 scale than with the Risser grade.21
| Risser sign | Percentage of curves that progressed | |
|---|---|---|
| 5- to 19-degree curves | 20- to 29-degree curves | |
| Grade 0 or 1 | 22 | 68 |
| 2, 3, or 4 | 1.6 | 23 |
| Cobb angle (degrees) | Risser grade | Radiography/referral | Treatment |
|---|---|---|---|
| 10 to 19 | 0 to 1 | Radiography every six months, no referral | Observe |
| 10 to 19 | 2 to 4 | Radiography every six months, no referral | Observe |
| 20 to 29 | 0 to 1 | Radiography every six months, referral | Brace after 25 degrees |
| 20 to 29 | 2 to 4 | Radiography every six months, referral | Observe or brace* |
| 29 to 40 | 0 to 1 | Referral | Brace |
| 29 to 40 | 2 to 4 | Referral | Brace |
| > 40 | 0 to 4 | Referral | Surgery† |
Treatment
Determining which patients need referral to an orthopedist can be complicated, and clear indications are not always available.5,8,20 The risk of spinal curve progression increases with higher Cobb angle and lower Risser grade. However, the trend in recent years is that fewer patients need radiography, and fewer patients who undergo radiography need treatment.5,8 Treatment modalities such as physical therapy, chiropractic care, and electrical stimulation have questionable benefit in preventing scoliosis progression.3 Bracing and surgery are options, but the evidence for them is limited.9,23–25
A 50-year follow-up study of late-onset idiopathic scoliosis including 117 untreated patients and 62 age- and sex-matched volunteers found that patients with untreated scoliosis are productive, are high-functioning, and usually have little physical impairment other than back pain and cosmetic concerns.26 Table 3 includes general referral and treatment guidelines for scoliosis.3
Data Sources: A PubMed search was performed using the key terms scoliosis, adolescent scoliosis, and scoliosis screening. The search included randomized controlled trials, reviews, clinical trials, and meta-analyses. Also searched were the Cochrane Database of Systematic Reviews, Agency for Healthcare Research and Quality evidence reports, and National Guideline Clearinghouse. Search dates: October 16 and 18, 2010; September 1, 2013.
