
Am Fam Physician. 2014;89(4):256-258
Related letter: Glycemic Control Is an Important Consideration in Diabetes Care
Author disclosure: No relevant financial affiliations.
Because sugar was historically the defining feature of diabetes mellitus (meaning “excess urination of honey”), treatment focused primarily on lowering blood glucose levels until recently. However, based on high-quality evidence from meta-analyses, glucose control should no longer be the main focus of treatment. A new approach to the care of adults with type 2 diabetes emphasizes proven interventions that improve duration and quality of life.
Bolstering data from the University Group Diabetes Program published in 1970,1 four more recent studies have shown that intensive treatment aimed at lowering blood glucose levels neither affects mortality nor decreases complications of type 2 diabetes.2–5 In contrast, interventions that are especially effective at extending life in these patients include smoking cessation,6 blood pressure control, and reduction of lipid levels.5 The United Kingdom Prospective Diabetes Study also showed that treatment with metformin (Glucophage) decreases mortality, regardless of its effect on blood glucose or A1C levels.7 These findings are reflected in new guidelines from the American Diabetes Association and the European Association for the Study of Diabetes.8
An easy way to illustrate this new approach to patients is by “lending a hand” (Figure 1).4,5,7,9–14 From thumb to little finger, each digit on an open hand portrays one intervention in decreasing order of benefit: smoking cessation (thumb), blood pressure control (index finger), metformin therapy (middle finger), lipid reduction (ring finger), and glycemic control (little finger).5,7,14–16
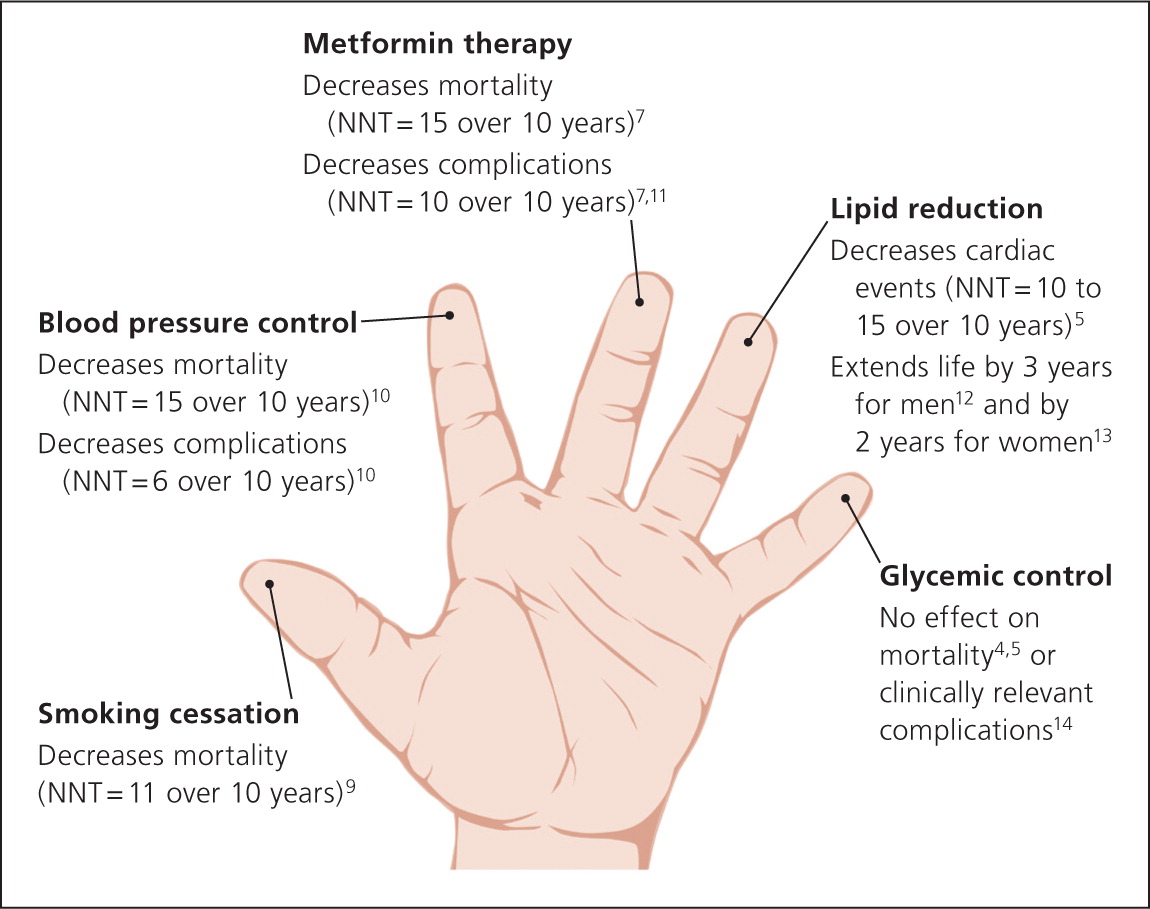
Step 1 (Thumb): Smoking Cessation
Smoking poses a greater risk of morbidity and mortality than any other physiologic abnormality in patients with diabetes.15 Addressing other issues without addressing smoking is like rearranging deck chairs on the Titanic. Smoking cessation is the primary goal except in patients with other risk factors that are so poorly controlled they will cause short-term effects (e.g., hypertensive crisis).
Step 2 (Index Finger): Blood Pressure Control
Blood pressure should be decreased to less than 140/80 mm Hg, based on evidence of fewer cardiovascular events and lower mortality in patients with type 2 diabetes.2,10,16–18 Further reducing the systolic blood pressure to 120 mm Hg confers no additional benefit and may increase the risk of adverse effects, such as syncope, arrhythmia, and renal failure.18 A thiazide diuretic or angiotensin-converting enzyme inhibitor should be the initial choice for pharmacotherapy.16,19
Step 3 (Middle Finger): Metformin Therapy
Metformin therapy delays premature mortality independent of its effect on glucose levels, and should be prescribed for overweight patients with type 2 diabetes unless contraindicated.7,20 Lactic acidosis, once associated with phenformin use, is not a risk with metformin, and it is even safe in patients with moderate renal dysfunction (i.e., glomerular filtration rate of 30 to 59 mL per minute per 1.73 m2).21
Step 4 (Ring Finger): Lipid Reduction
Step 5 (Little Finger): Glycemic Control
Despite the current focus on A1C as an indicator of quality of care, lowering glucose levels to the nondiabetic normal range does not significantly affect mortality compared with conventional glycemic control,4 and it does not reduce the risk of macrovascular complications from myocardial infarction or stroke.3,14 Glycemic reduction increases the risk of hypoglycemia and its complications,2 and can actually increase mortality if A1C is lowered consistently below 7.5%.23
Recently revised guidelines from the American Diabetes Association and the European Association for the Study of Diabetes propose less stringent goals (e.g., A1C less than 8%) for most patients with diabetes who have comorbidities.8,20 A fasting blood glucose level of less than 200 mg per dL (11.1 mmol per L) is reasonable in these patients.8,20 A management plan should center on controlling hyperglycemic symptoms in concert with individual patient preferences.
Physicians should not let well-intentioned but misguided concern for glucose levels distract them from attending to other interventions that more profoundly affect mortality: smoking cessation, blood pressure control, metformin therapy, and lipid reduction. This approach requires a shift in the thinking of patients and physicians. Patients with type 2 diabetes who currently focus first on glycemic control will need to “reverse the hand” to improve the duration and quality of life.
