
Am Fam Physician. 2014;90(11):791-792
Author disclosure: No relevant financial affiliations.
A 42-year-old woman presented with gradually decreasing vision in her right eye that began five days earlier. She did not have chest pain, palpitations, headache, or other neurologic symptoms. She was taking lisinopril (Zestril), furosemide (Lasix), and carvedilol (Coreg) and had allergies to atenolol (Tenormin), hydrochlorothiazide, and codeine. She had a history of hypertension and tobacco use.
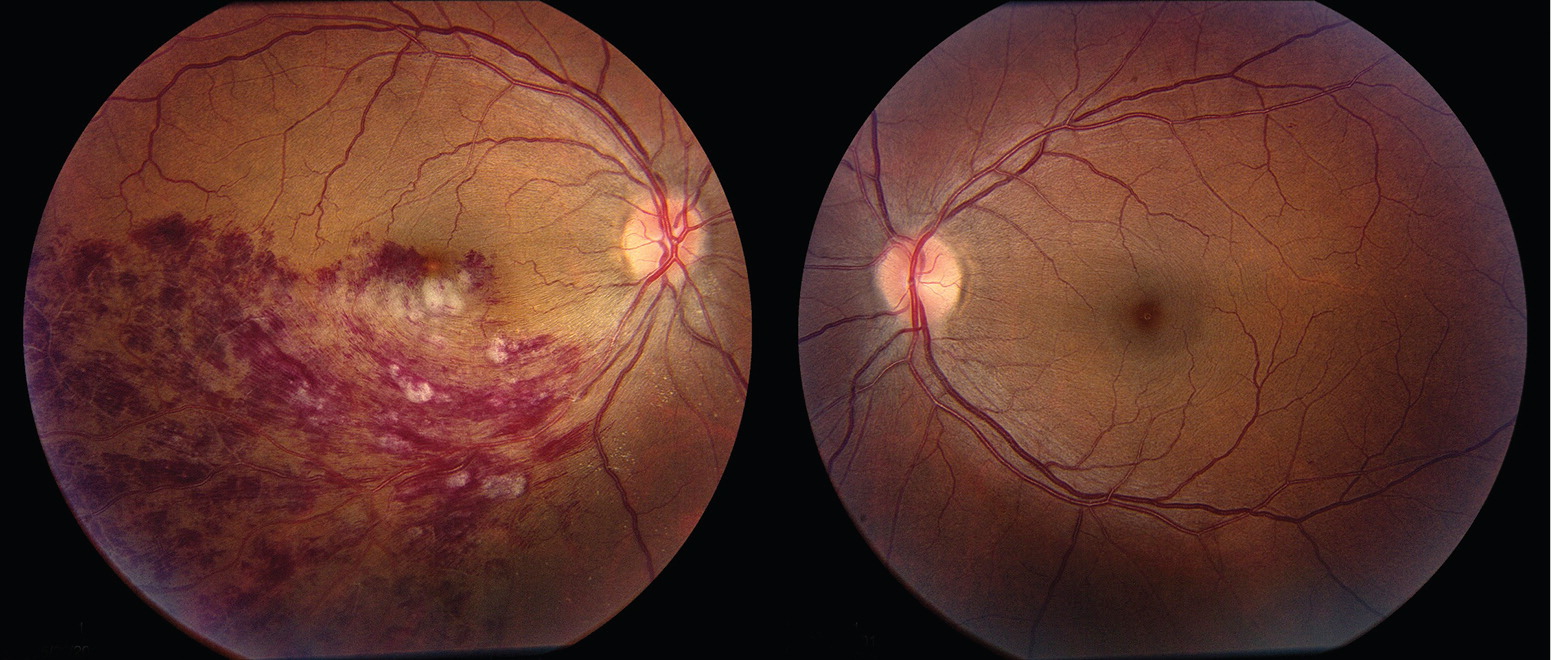
Her blood pressure was 180/104 mm Hg, and her pulse was 112 beats per minute. Her body mass index was 33 kg per m2. Visual acuity was 20/400 in her right eye and 20/20 in her left eye. No afferent pupillary defect was noted. Intraocular pressure was 15 mm Hg in each eye. Confrontation visual field testing demonstrated a superior scotoma in her right eye and no defect in the left eye. Findings on anterior segment examination were normal in each eye. Retinal examination revealed intraretinal hemorrhages in the inferior half of the retina in the right eye with edema extending into the macula (see accompanying figure). The left optic nerve and macula were normal. Complete blood count, creatinine, and blood glucose measurements were normal.
Question
Discussion
The answer is A: branch retinal vein occlusion. Retinal vein occlusion is the second most common cause of vision loss due to retinal vascular disease, after diabetic retinopathy, and can include branch or central occlusion.1 Risk factors include hypertension, diabetes mellitus, smoking, hypercoagulable conditions, obesity, and older age.
Branch retinal vein occlusions are characterized by dilated and tortuous veins, flame-shaped and dot and blot hemorrhages, and retinal edema. The amount of retina involved corresponds to the area drained by the affected retinal vein. Small occlusions are usually asymptomatic and require no specific treatment. Larger occlusions, such as in this case, can cause macular edema, resulting in significant vision loss. Treatment options for macular edema include retinal laser therapy and intravitreal injections of antivascular endothelial growth factor medications.2,3 Systemic risk factors should be aggressively treated in patients with either type of occlusion to prevent additional vascular events.
Central retinal vein occlusions appear similarly to those in branch veins, except that they involve hemorrhage in all quadrants of the retina with macular edema.
Diabetic retinopathy is a leading cause of blindness and vision loss. It is usually bilateral, although often asymmetric, and commonly includes hemorrhages, exudates, macular edema, and cotton-wool spots in various locations. Retinal exudates reduce vision when located in the macula. Proliferative retinopathy with neovascularization of the optic disc and/or retina can be followed by vitreous hemorrhage also resulting in vision loss.4
Optic neuritis is an inflammation of the optic nerve that is associated with multiple sclerosis in about 50% of cases.5 There is usually eye pain and an afferent pupillary defect with the swinging flashlight test (i.e., Marcus Gunn pupil). The optic nerve can appear swollen with hemorrhages on and around the optic disc. When the optic disc appears normal but the clinical history suggests optic neuritis, the term retrobulbar optic neuritis is used. Magnetic resonance imaging of the brain and orbits is useful for this diagnosis.
Papilledema is bilateral and a result of elevated intracranial pressure. Headache is a common symptom. Visual acuity may be normal or slightly reduced, and the blind spot may be enlarged. The optic discs are elevated and there is loss of central venous pulsation. There are often hemorrhages on and around the optic discs. Some causes of papilledema are serious, such as an intracranial mass lesion, brain hemorrhage, or cerebral edema.6
| Condition | Characteristics |
|---|---|
| Branch retinal vein occlusion | Unilateral; dilated and tortuous retinal veins, flame-shaped and dot and blot hemorrhages, retinal edema; limited to a section of the retina drained by the affected vein; macular edema may be present |
| Central retinal vein occlusion | Unilateral; dilated and tortuous retinal veins; all quadrants of the retina are involved; macular edema usually present |
| Diabetic retinopathy | Bilateral, although often asymmetric; hemorrhages, hard exudates with a yellow, waxy appearance, cotton-wool spots; neovascularization and vitreous hemorrhage possible; macular edema usually present |
| Optic neuritis | Unilateral; eye pain, afferent pupillary defect; optic disc may appear normal when the inflammation is retrobulbar |
| Papilledema | Bilateral; optic disc swelling, hemorrhage, enlarged blind spot, headache |
