Am Fam Physician. 2015;91(11):758
Related Graham Center Policy One-Pager: Osteopathic Schools Are Producing More Graduates, But Fewer Are Practicing in Primary Care
Author disclosure: No relevant financial affiliations.
Trends in the composition of the primary care physician workforce since 2000 show a declining proportion of U.S. allopathic physicians, and increasing proportions of U.S. osteopath physicians and both U.S.-born and foreign-born international graduates.
Mounting evidence supports the need for more primary care physicians to care for an expanding, aging, and insured population. The U.S. primary care physician workforce is composed of graduates from both domestic and international medical schools. Trends in training, recruitment, and practice have policy and ethical implications. We used the American Medical Association Physician Masterfile to examine the sources of primary care physicians from three types of medical schools: U.S. allopathic, U.S. osteopathic, and international medical schools (Figure 1).
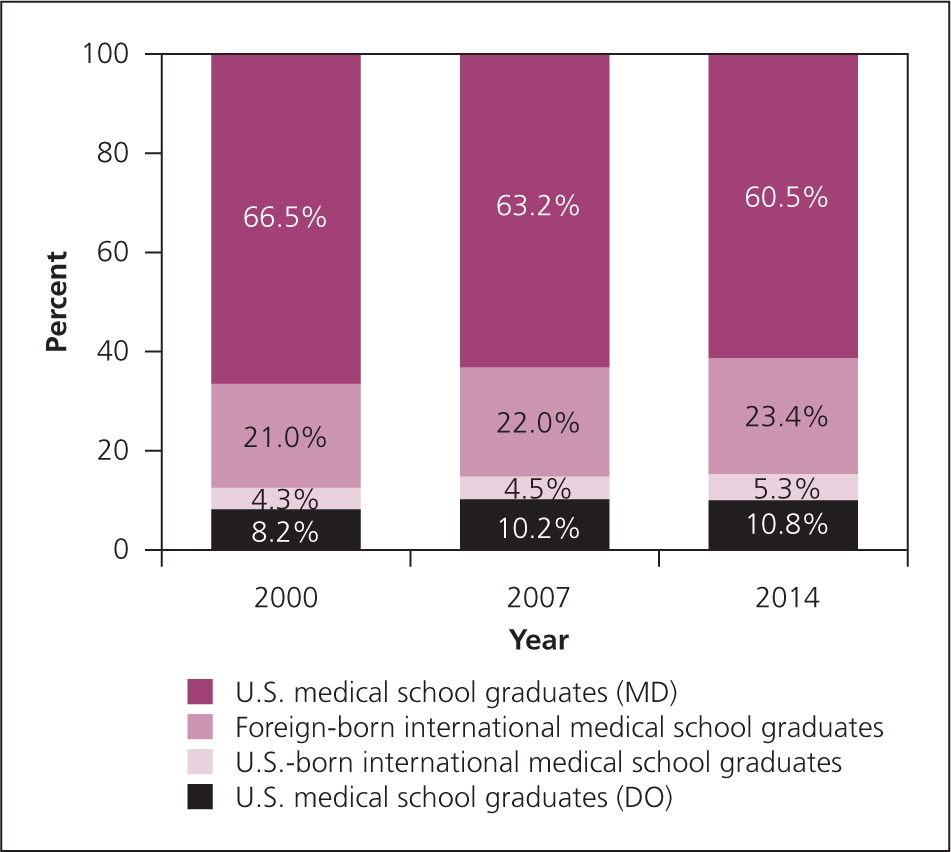
The total physician workforce expanded by 30% from 541,243 in 2000 to 705,498 in 2014, with primary care expanding at a slower rate (22.5%) than specialists (34%). The proportion of practicing primary care physicians trained in U.S. allopathic medical schools decreased from 66.5% in 2000 to 60.5% in 2014, whereas the proportion of international medical school graduates, both foreign- and U.S.-born (including “off-shore” schools with primarily U.S.-born students), has increased. An initial increase in the osteopathic contribution appears to be leveling.
There has been a steady decrease in U.S. allopathic medical schools' contribution to the primary care workforce, whereas osteopathic contributions have increased because of an increase in graduates, although the decline in the percentage of osteopathic graduates pursuing primary care is concerning.1 Graduates of international medical schools are increasingly a source of U.S. primary care physicians. However, relying on them to address the U.S. primary care physician shortage may contribute to the “brain drain” of low-income countries and also has ethical implications.2,3
Over the past decade, there has been substantial public investment in U.S. medical school expansion, and programmatic enhancement to increase primary care physician production.4 The outputs and outcomes of policies and investments to enhance primary care education and training should be closely monitored to assure that these investments are attaining intended objectives. Publicly supported educational institutions should incentivize desired outcomes and provide opportunities for effective programs to be expanded and replicated.
The information and opinions do not necessarily reflect AAFP views or policy.
Series coordinated by Sumi Sexton, MD, Associate Medical Editor.