
Am Fam Physician. 2018;97(8):531-532
Author disclosure: No relevant financial affiliations.
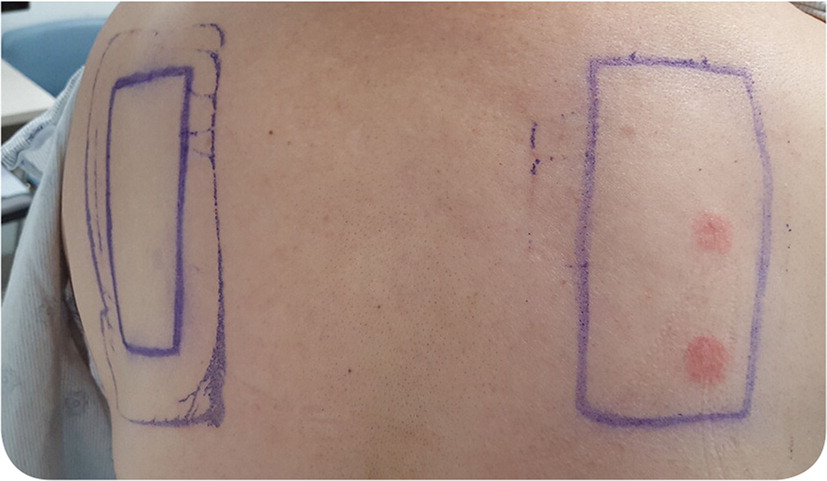
A healthy 62-year-old woman presented with a pruritic rash on her left ankle (Figure 1). The rash began five days earlier as numerous discrete, 2- to 3-mm erythematous papules, which coalesced into a large rectangular plaque. The patient noted the eruption three days after she applied a lidocaine patch to the area for pain. She had no history of similar symptoms. She had no history of allergy to latex, plastic, or other personal care products; atopic dermatitis; asthma; or allergic rhinitis. Patch testing was performed (Figure 2).

Question
Discussion
The answer is A: allergic contact dermatitis. The patient's history, the geometric nature of her eruption, and a positive patch test result are consistent with delayed T cell–mediated (type IV) hypersensitivity reaction to lidocaine. On the patch test, the patient had a reaction to lidocaine, the lidocaine patch, and the lidocaine injection (not shown in Figure 2). She was tested against all potential allergens contained in the patch (paraben preservative, adhesive, and plastic) but reacted only to lidocaine. Treatment of allergic contact dermatitis is symptomatic and usually includes a topical corticosteroid. The initial eruption typically subsides in three to four weeks.
Patch testing is used to diagnose type IV hypersensitivity reactions by exposing an area of skin to a suspected allergen for 48 hours. The skin is evaluated at 48 to 72 hours and again on day 5 to 7.1,2 A positive reaction may range from mild erythema and induration to severe vesiculation.3 Indications for patch testing include suspected allergic contact dermatitis; treatment-resistant chronic dermatitis; eczematous dermatitis in persons with high-risk occupations such as health care professionals, dental assistants, machinists, or rubber and plastic workers; and dermatitis of unknown etiology.3
Reactions to bites from arthropods such as fleas or bedbugs can appear as wheals or pruritic papules.4 Symptoms may not present until hours after the bites occur.5 Bedbug bites classically follow vascular structures and can present with a linear distribution called “breakfast, lunch, and dinner.”4 Flea bites often occur on the feet and legs as the arthropod jumps from the floor to exposed skin.
Irritant contact dermatitis is a nonimmunologic reaction to topical or environmental irritants, such as soap, latex, bleach, or battery acid.5 These irritants disrupt the skin barrier and cause an eczematous eruption that typically involves the hands. The skin eruption usually begins within minutes to hours of exposure to the irritant and normally resolves within two weeks.5
Morbilliform drug eruption is a common type of reaction to medications, often sulfa drugs, penicillin, allopurinol, and phenytoin (Dilantin).6 The presentation (macules and thin papules that blanch with pressure) resembles measles. Symptoms occur five to 14 days after exposure to the medication but may occur earlier (within two or three days) in patients who have been previously sensitized.6
| Allergic contact dermatitis | Type IV hypersensitivity reaction to an allergen |
| Arthropod bite reaction | Wheals or pruritic papules following arthropod bites |
| Atopic dermatitis | Genetic skin barrier defect results in pruritus and rash, often on the flexor surfaces in adults and extensor surfaces in infants; present since childhood |
| Irritant contact dermatitis | Nonimmunologic reaction to topical or environmental agent; erythematous eruption that typically involves the hands |
| Morbilliform drug eruption | Common type of reaction to medications such as sulfa drugs, penicillin, allopurinol, and phenytoin (Dilantin); presentation resembles measles (macules and thin papules that blanch with pressure) |
