
Am Fam Physician. 2019;99(9):584-586
Author disclosure: No relevant financial affiliations.
Clinical Question
When a patient presents with chest pain, how should the primary care physician use the patient’s history to decide the next steps?
Evidence Summary
Chest pain is one of the most common presenting symptoms in primary care. Three prospective studies in the primary care setting found that among patients with chest pain, 10.5% to 11.3% had stable angina and 1.5% to 3.7% had acute cardiac ischemia.1 Other serious causes of chest pain are less common in the primary care setting.
Based on the patient history, the physician must make a subjective judgment about the likelihood of coronary artery disease (CAD) as the cause and then decide whether to perform a diagnostic test. In many cases, the diagnosis is clearly not CAD (e.g., pain when pressing the chest and no characteristics of CAD in a young patient), but the history is often equivocal. In such cases, diagnostic tests may be valuable, but the potential for misleading results (e.g., false-negative results when the pretest probability of CAD is very high, false-positive results when the pretest probability is very low) complicates the interpretation of test results.
Since 1990, five clinical decision rules for interpreting the history in patients with chest pain in primary care have been published. Calling their collaboration INTERCHEST, the authors of these rules agreed to combine the data from their studies to develop a new chest pain clinical decision rule for primary care.2 Their statistical analysis identified five predictors of CAD; each was assigned a weight of +1 when present and zero when absent. A sixth finding (localized pain when pressing the chest wall) reduced the probability of CAD, so this finding was assigned a weight of –1 when present (Table 1).2
| Clinical predictor | Points |
|---|---|
| Pain reproduced by palpating the chest wall | −1 |
| Older age (men ≥ 55 years; women ≥ 65 years) | 1 |
| Physician initially suspected a serious condition | 1 |
| Chest discomfort feels like “pressure” | 1 |
| Chest pain related to effort | 1 |
| History of coronary artery disease | 1 |
| Total (range −1 to 5): | ____ |
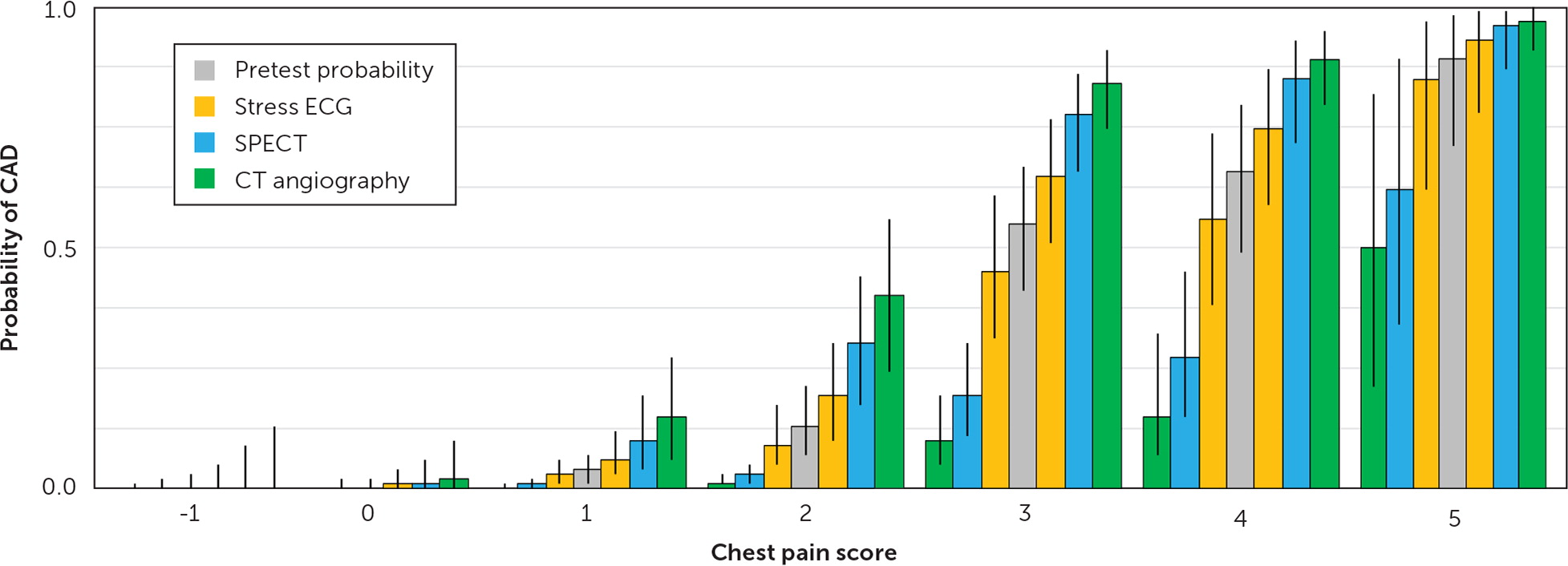
In Figure 12–5 (a graph based on the numbers in eTable A), the gray bar shows the pretest probability of CAD for each chest pain score in an INTERCHEST study site, in which the overall prevalence of CAD was 13% in patients presenting for evaluation of chest pain. The figure also shows—for each chest pain score—the posttest probabilities of CAD after stress electrocardiography (ECG), single-photon emission computed tomography (SPECT), or computed tomography (CT) angiography. The bars to the left of the gray bar denote the probability of CAD after a negative test result, and the bars to the right of the gray bar denote the probability of CAD after a positive result. The vertical black lines on each bar denote the 95% CIs, which reflect uncertainty in the chest pain score 2 and in the sensitivity and specificity of stress ECG, SPECT, and CT angiography.3,4
| Chest pain score (Table 1) | |||||||
|---|---|---|---|---|---|---|---|
| Parameter | –1 | 0 | 1 | 2 | 3 | 4 | 5 |
| Pretest | |||||||
| CAD prevalence (patients with CAD/total patients)* | 0/87 | 1/208 | 6/160 | 11/85 | 29/53 | 21/32 | 17/19 |
| Probability (95% CI) | 0.00 (0.00 to 0.03) | 0.00 (0.00 to 0.02) | 0.04 (0.01 to 0.07) | 0.13 (0.07 to 0.21) | 0.55 (0.41 to 0.67) | 0.66 (0.49 to 0.80) | 0.89 (0.71 to 0.98) |
| Posttest probability after stress ECG (95% CI) | |||||||
| Positive result | 0.00 (0.00 to 0.05) | 0.01 (0.00 to 0.04) | 0.06 (0.02 to 0.12) | 0.19 (0.10 to 0.30) | 0.65 (0.51 to 0.77) | 0.75 (0.59 to 0.87) | 0.93 (0.78 to 0.99) |
| Negative result | 0.00 (0.00 to 0.02) | 0.00 (0.00 to 0.02) | 0.03 (0.01 to 0.06) | 0.09 (0.05 to 0.17) | 0.45 (0.31 to 0.61) | 0.56 (0.38 to 0.74) | 0.85 (0.62 to 0.97) |
| Posttest probability after SPECT (95% CI) | |||||||
| Positive result | 0.00 (0.00 to 0.09) | 0.01 (0.00 to 0.06) | 0.10 (0.04 to 0.19) | 0.30 (0.17 to 0.44) | 0.78 (0.66 to 0.86) | 0.85 (0.72 to 0.93) | 0.96 (0.87 to 0.99) |
| Negative result | 0.00 (0.00 to 0.01) | 0.00 (0.00 to 0.00) | 0.01 (0.00 to 0.02) | 0.03 (0.01 to 0.05) | 0.19 (0.11 to 0.30) | 0.27 (0.15 to 0.45) | 0.62 (0.34 to 0.89) |
| Posttest probability after CT angiography (95% CI) | |||||||
| Positive result | 0.00 (0.00 to 0.13) | 0.02 (0.00 to 0.10) | 0.15 (0.06 to 0.27) | 0.40 (0.24 to 0.56) | 0.84 (0.75 to 0.91) | 0.89 (0.80 to 0.95) | 0.97 (0.91 to 1.00) |
| Negative result | 0.00 (0.00 to 0.00) | 0.00 (0.00 to 0.00) | 0.00 (0.00 to 0.01) | 0.01 (0.01 to 0.03) | 0.10 (0.05 to 0.19) | 0.15 (0.07 to 0.32) | 0.50 (0.21 to 0.82) |
For scores of −1 and 0, the pretest probability of CAD (gray bar) is very low. The main question facing the physician is whether a test result could change the next steps. Very few patients with a score of −1 or 0 would have a positive result on SPECT or CT angiography, and the probability of CAD after a positive test result would be very low. Most test results would be negative, and the probability of CAD after a negative test result would be very low.
The interpretation of chest pain scores that reflect higher probabilities of CAD is more complicated. In patients with a high probability of CAD (chest pain score of 5), it is reasonable to perform a diagnostic test because positive test results are common in these patients and would confirm a diagnosis of CAD, but it is important to not be misled by a negative result. As shown in Figure 1,2–5 the probability of CAD in patients with a chest pain score of 5 and negative results on stress ECG is 85%. Even after a negative CT angiography result, the probability is 50%.
A test result has the largest effect on the probability of CAD when diagnostic uncertainty is greatest, which it is in a patient with a chest pain score of 3 or 4. Compared with low- or high-risk patients, the probability of CAD in these intermediate-risk patients changes much more after CT angiography or SPECT than after a stress ECG (Figure 12–5 ). But, a negative result on CT angiography does not rule out CAD, except in patients with chest pain scores of 2 or less.
Applying the Evidence
A 70-year-old man presented to his primary care physician with a one-month history of intermittent chest pain. The physician became concerned about CAD because the pain occurred with exertion and the patient described it as “pressure.” The patient did not have a history of CAD and did not take medications. The physical examination findings were normal, including a blood pressure of 110/80 mm Hg. Applying pressure on the anterior chest did not reproduce the pain.
Based on the examination, the physician calculated a chest pain score of 4, which corresponds to a 66% probability of CAD before any testing is performed. The physician considered ordering a stress ECG, but, according to Figure 1,2–5 she realized that regardless of the results, she would still be too uncertain of the diagnosis to take definitive action (the posttest probability would have been 75% if the test result was positive and 56% if it was negative). Instead, she opted for CT angiography, which was negative, giving this patient a 15% posttest probability of CAD. The physician prescribed sublingual nitroglycerin as needed for chest pain and scheduled a two-week follow-up phone call.
The foundation of this article is the chest pain clinical decision rule developed by the INTERCHEST Collaboration. The authors note that although the INTERCHEST Collaborators nominated them to author this article, the authors did not consult with them during the preparation of this article, and they are not responsible for any errors. The other members of the collaboration are Minalu G, Bösner S, Buntinx F, Burnand B, Herzig L, Knottnerus JA, Nilsson S, Renier W, Sox CH, and Donner-Banzhoff N.
The statements presented in this article are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors, or its Methodology Committee.
