
Am Fam Physician. 2020;102(4):202-204
Published online July 13, 2020.
Author disclosure: No relevant financial affiliations.
Although overshadowed by the coronavirus disease 2019 (COVID-19) pandemic, results of the 2020 National Residency Match Program (The Match) are in. This is the first year for a fully integrated single match because the American Osteopathic Association accreditation of residency programs will soon sunset, completing its consolidation into the Accreditation Council for Graduate Medical Education. What did we learn?
A record number of family medicine positions were filled. It is significant that even when adjusting for the previous American Osteopathic Association match positions shifting to The Match, 44 more total family medicine slots were filled with graduating U.S. medical students than in 2019. Although the number of osteopathic and international medical school graduates matching in family medicine increased, the number of U.S. allopathic fourth-year students matching in family medicine fell from 1,617 to 1,557 (Figure 1).1
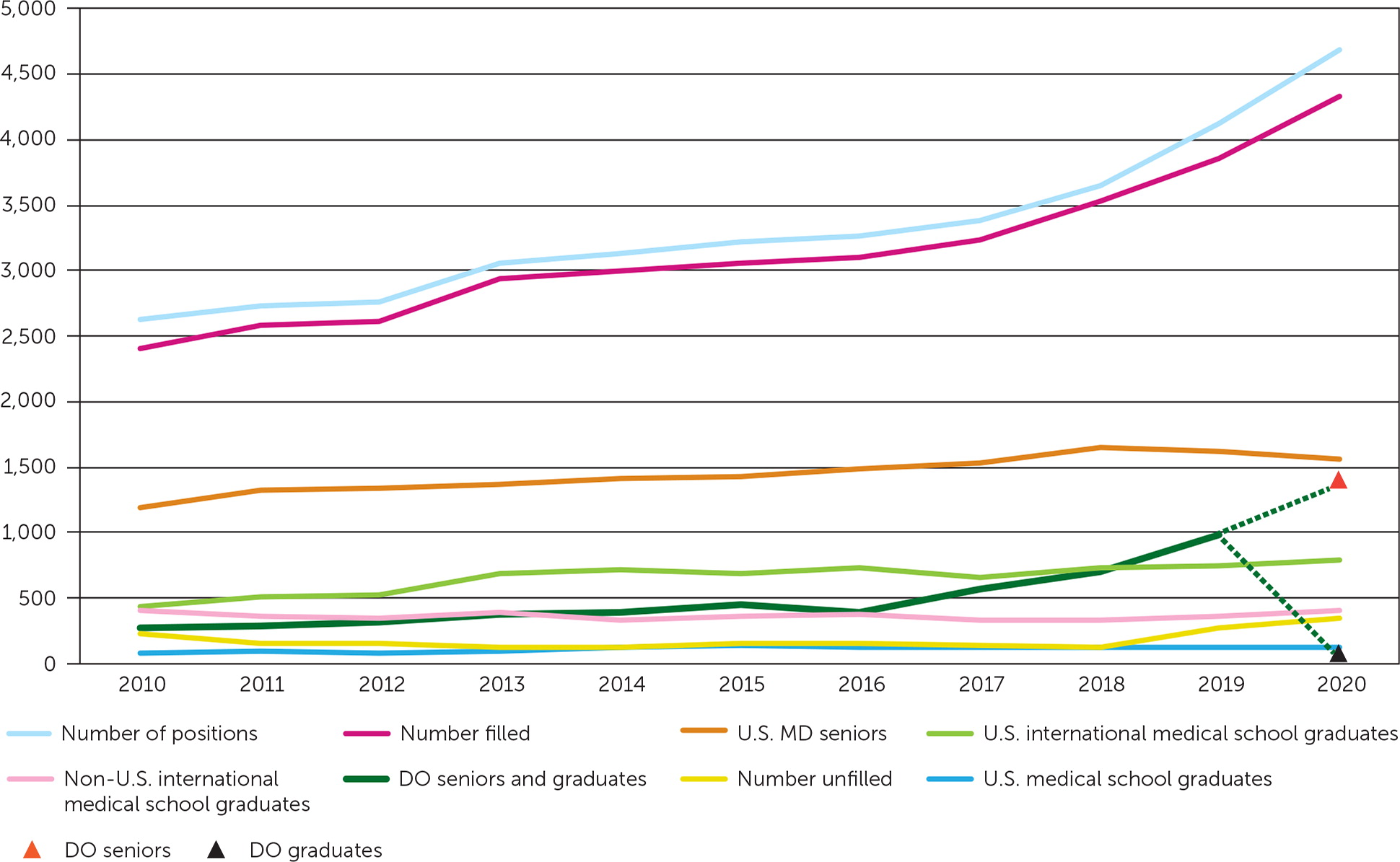
Despite multiple family medicine organizations prioritizing increasing the percentage of medical students choosing family medicine, the overall increase was essentially stagnant with 12.6% choosing family medicine. This is merely one-half of America Needs More Family Doctors' ambitious goal of 25% of U.S. medical school graduates choosing family medicine by 2030.1
In 2014, four key factors were identified to increase the number of medical students choosing family medicine as a career: pipeline, educational process, practice transformation, and payment.2 These pillars of influence remain the root factors requiring improvement. Family medicine is not failing America; the American health care system is failing family medicine. The current crisis caused by the COVID-19 pandemic has amplified the significant flaws in a mostly fee-for-service business model. Recovering from this crisis must include a shift to prospective, population-based payment, which better serves communities. Telemedicine, perhaps considered the modern house call, has been widely and rapidly embraced because of the compelling circumstance created by COVID-19 and needs a permanent and prominent role in care provision moving forward. Integrating telemedicine as a sustainable tool requires the adoption of a financial support model for this engaging approach to patient care.
The increasingly prominent role of family physicians during the past few months highlights the versatility of family medicine training and competencies.3–5 Family physicians have flexed into inpatient, community outreach, and emergency coordination roles. Individuals, families, communities, and health systems need effective family physicians and family physician leaders. In one setting, this shift has meant that family physicians have gone from being viewed as unnecessary to indispensable.6 The future for family physicians will be promising in the postpandemic era if the opportunities to appropriately reform primary care practice, regulation, and payment are enacted swiftly and with permanence.
What can we expect ahead in the process of recruiting medical students into family medicine? The COVID-19 pandemic and its impact on routine activities has led to remarkable uncertainty. Anxiety is running high for medical students experiencing disruption of medical training that is unprecedented in the United States. For good reasons, hands-on clinical training is being suspended and supplemented with virtual learning. For many, perhaps most, of us who chose family medicine as our calling, our decision was significantly influenced by a family physician role model. For me, this occurred early in my fourth year of medical school in an “away” elective rotation experience. This pathway has been truncated for many medical students.
In response to current uncertainties, the Coalition for Physician Accountability has released important recommendations to guide an alternative approach to residency recruiting and interviewing for The 2021 Match.7 These recommendations are meant to provide an equitable and consistent process that lessens health risk with the added benefit of decreased financial costs. Recommendations include minimizing away rotations for medical students, adopting exclusive use of virtual residency interviews, and delaying the opening of the electronic residency application service to allow more time for applicants and medical schools to gather and provide key application information important to residency programs.
In May 2020, multiple family medicine organizations responded with a letter to the family medicine community outlining support for the Coalition for Physician Accountability's recommendations but with important modifications and clarifications specific to family medicine. These include assuring medical student access to family medicine elective experiences.8
Predicting the results of The 2021 Match is impossible. For medical students to envision and trust their future in family medicine,9 medical schools and family medicine residency programs must find ways to connect learners with family physician role models early, and preferably often. The American Academy of Family Physicians' Family Medicine Interest Groups (https://aafp.org/fmig) help support meaningful connections between medical students and family medicine role models.
In our new reality, many relationships must, by necessity, be created and nurtured virtually. We must move quickly. Efforts are well underway with the American Academy of Family Physicians recently having the 2020 National Conference of Family Medicine Residents and Medical Students completely online (https://www.aafp.org/events/national-conference.html), including connecting medical students with family medicine residencies in a virtual exhibit hall.
Editor's Note: Dr. Knight is AAFP's senior vice president, education.
