
Am Fam Physician. 2021;103(6):373-374
Author disclosure: No relevant financial affiliations.
A 35-year-old patient presented with a two-month history of progressive bilateral blurry vision and a rash on the trunk that developed two weeks before presentation. He was not taking any medications. The patient had a few days of flulike symptoms about four months earlier.
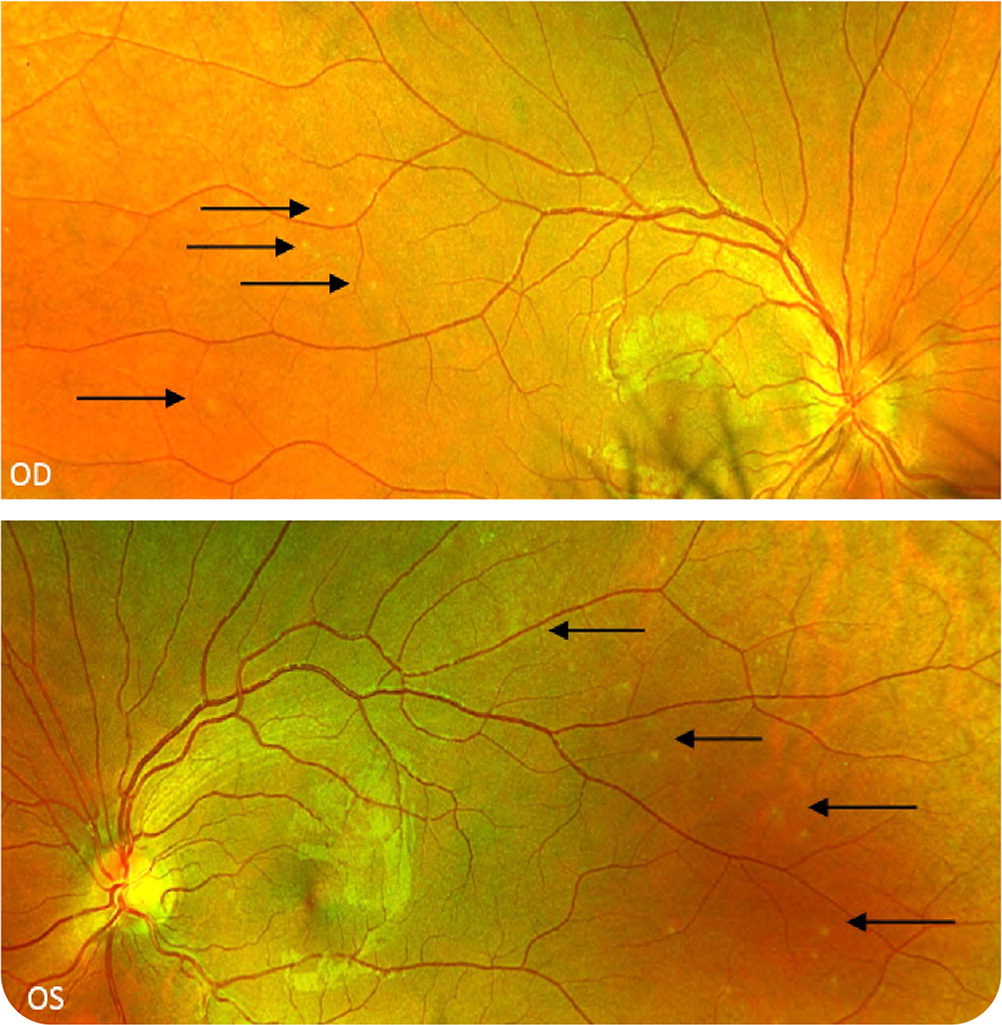
On examination, the patient appeared healthy and was in no distress. His visual acuity was 20/30 in each eye without a relative afferent pupillary defect. Ophthalmoscopy demonstrated bilateral asymmetric optic nerve head swelling and scattered tiny white spots in the retinas (Figure 1). There was an erythematous, maculopapular eruption on the trunk and left arm (Figure 2).

Question
Based on the patient's history, physical examination, and test findings, which one of the following is the most likely diagnosis?
A. Idiopathic intracranial hypertension.
B. Malignant hypertension.
C. Optic neuritis.
D. Secondary syphilis.
Discussion
Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum. Secondary syphilis occurs approximately two months after the initial infection and is typically associated with lymphadenopathy and a maculopapular rash.2 Ocular syphilis can occur at any stage of the disease but is most common in secondary syphilis. Inflammation results in swelling of the optic nerve head and retrobulbar optic neuropathy. Symptoms may include decreased visual acuity, decreased color perception, and pain with extraocular movements. Uveitis occurs in approximately 10% of cases and presents as red eye with pain and photo-phobia.1,2 An ophthalmologic evaluation is recommended for patients with syphilis and ocular symptoms.
Idiopathic intracranial hypertension most commonly occurs in obese women of childbearing age. It presents as bilateral papilledema accompanied by symptoms of increased intracranial pressure, such as headache, nausea, vomiting, and pulsatile tinnitus. Transient whitening of vision occurs when the patient bends down. Horizontal binocular diplopia may be present because of nonlocalizing sixth nerve palsy in some patients with increased intracranial pressure. Patients with idiopathic intracranial hypertension typically have normal visual acuity, whereas those with optic neuropathies usually have decreased central acuity.3
Malignant hypertension typically occurs in individuals with a blood pressure of 180/120 mm Hg or greater. It may cause blurred vision, but bilateral optic nerve head edema is rare. It may also present as retinopathy or optic neuropathy. Patients often have cotton-wool spots and may have flame hemorrhages due to poor autoregulation of blood vessels supplying the retina and the leakage of the serum from permeable capillaries.4
Optic neuritis is a manifestation of central nervous system demyelinating disease and most often occurs in women 20 to 40 years of age. It typically presents as subacute onset (hours to days) of unilateral vision loss accompanied by pain with eye movements. Objectively, relative afferent pupillary defects are present in the affected eye, and one-third of patients have mild optic nerve head swelling. Visual function spontaneously recovers to almost baseline in most patients.5
| Condition | Characteristics | Vision changes |
|---|---|---|
| Idiopathic intracranial hypertension | Bilateral papilledema accompanied by symptoms of increased intracranial pressure, such as headache, nausea, vomiting, and pulsatile tinnitus | Visual acuity is typically normal; transient whitening of vision occurs when the patient bends down; horizontal binocular diplopia is occasionally present |
| Malignant hypertension | Retinopathy or optic neuropathy; cotton-wool spots and flame hemorrhages; may cause optic nerve head edema; blood pressure is 180/120 mm Hg or greater | Blurred vision possible |
| Optic neuritis | Subacute onset (over hours or days); relative afferent pupillary defect and mild optic nerve head swelling | Unilateral vision loss accompanied by pain with eye movements |
| Secondary syphilis | Swelling of the optic nerve head and retrobulbar optic neuropathy; other symptoms of secondary syphilis are often present, most commonly lymphadenopathy and a maculopapular rash | Decreased visual acuity, decreased color perception, photophobia, and pain with extraocular movements are possible |
