
Am Fam Physician. 2021;103(11):698-700
Author disclosure: No relevant financial affiliations.
Key Points for Practice
• Structured diabetes self-management education programs are recommended because they improve self-efficacy and clinical outcomes.
• First-line antiglycemic treatment for type 2 diabetes and CKD with eGFR as low as 30 mL per minute per 1.73 m2 should include metformin and an SGLT2 inhibitor to improve cardiovascular outcomes and limit CKD progression.
• ACE inhibitor or ARB treatment should be maximized in patients who have diabetes with albuminuria and hypertension unless complicated by symptomatic hypotension, uncontrolled hyperkalemia, or more than a 30% increase in creatinine level.
From the AFP Editors
Diabetes mellitus affects more than 450 million people globally, which could increase to more than 700 million people by 2045. Up to 40% of cases of diabetes are complicated by chronic kidney disease (CKD), with persistent abnormalities of kidney function demonstrated by elevated urine albumin excretion or reduced estimated glomerular filtration rate (eGFR). The Kidney Disease: Improving Global Outcomes (KDIGO) group, an international organization dedicated to nephrology clinical practice guidelines, has developed a new guideline for management of diabetes with CKD.
Team-Based Care
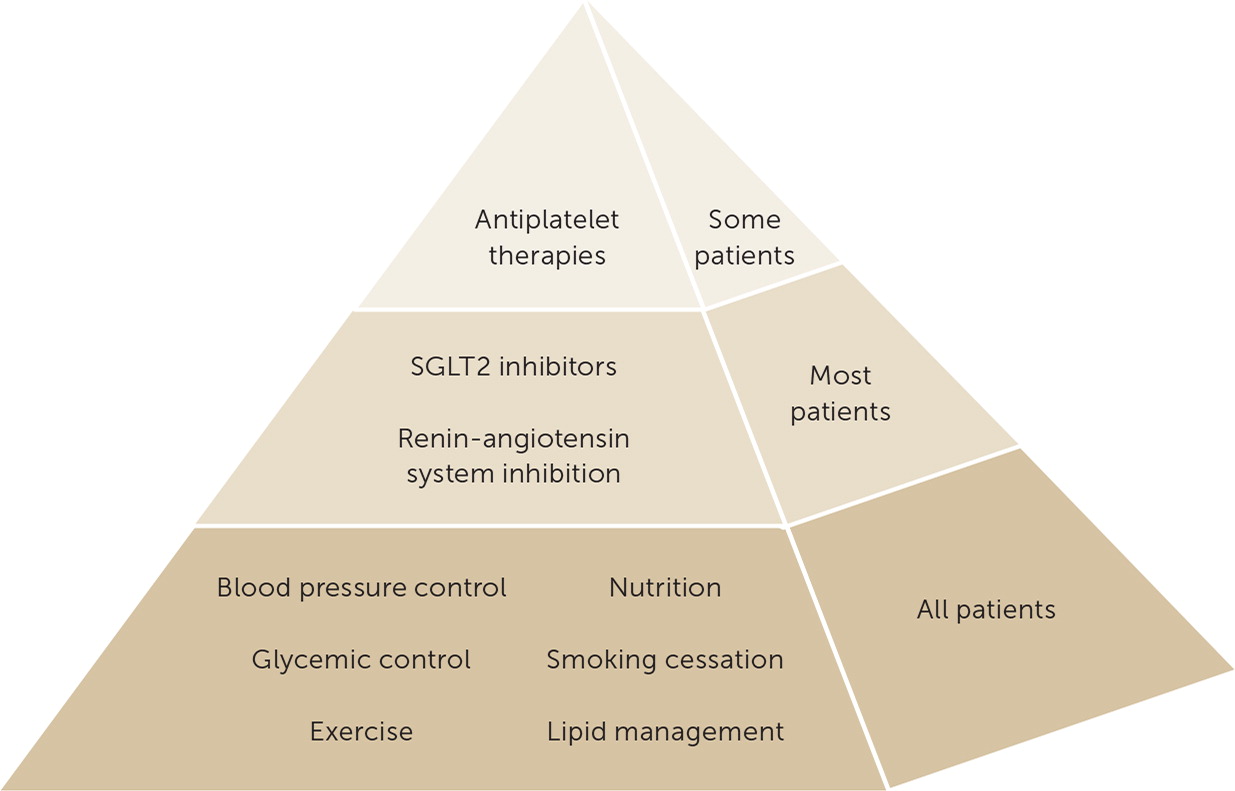
People with diabetes and CKD have high risks of CKD progression, cardiovascular disease (CVD), and mortality, which can be reduced with a comprehensive approach to lifestyle and risk factor management in combination with appropriate pharmacotherapy (Figure 1). Optimal care includes primary care, cardiology, nephrology, endocrinology, psychology, nutrition, and disease management nursing support.
Self-Management Education
Structured education in diabetes self-management is recommended for people with diabetes and CKD because education improves long-term clinical outcomes and quality of life. Group-based education programs improve A1C level, fasting blood glucose level, body weight, self-efficacy, and patient satisfaction.
Dietary and Lifestyle Management
Dietary advice for people with diabetes and CKD should include consumption of a balanced, healthy diet that is high in vegetables, fruits, whole grains, fiber, legumes, plant-based proteins, unsaturated fats, and nuts and lower in processed meats, refined carbohydrates, and sweetened beverages. Nutritional recommendations may have to be adjusted for conditions such as hyperkalemia as well as personal and cultural preferences. Daily dietary protein intake should be maintained at 0.8 g per kg, which is recommended for all people. Neither higher- nor lower-protein diets are advised, although people on dialysis should have daily dietary protein intake of 1.0 to 1.2 g per kg to offset muscle catabolism. Sodium intake should be limited to less than 2 g per day or less than 5 g of sodium chloride.
Lower levels of physical activity are common and associated with worse clinical outcomes. Moderate-intensity physical activity for at least 150 minutes per week and reduction in sedentary activity are recommended.
In addition to further increasing cardiovascular risk, cigarette smoking is associated with kidney disease progression, and patients should be advised to quit smoking.
Glycemic Treatment
For people with type 2 diabetes and CKD with an eGFR 30 mL per minute per 1.73 m2 or higher, metformin and sodium-glucose cotransporter 2 (SGLT2) inhibitors, in combination, are recommended for first-line medical treatment because they improve glycemic control outcomes. Metformin limits weight gain and reduces cardiovascular events, whereas the SGLT2 inhibitor improves cardiovascular outcomes and limits kidney disease progression.
Metformin is safe in patients with an eGFR above 45 mL per minute per 1.73 m2 unless risk for acute kidney injury is high. The dose of metformin should be reduced when eGFR is less than 45 mL per minute per 1.73 m2 and discontinued when eGFR is less than 30 mL per minute per 1.73 m2 or in people treated with dialysis.
SGLT2 inhibitor use can cause a reversible decline in eGFR that usually does not require stopping the medication. The SGLT2 inhibitor can be continued with an eGFR below 30 mL per minute per 1.73 m2 if well-tolerated and dialysis is not imminent. SGLT2 inhibitor use is associated with genital mycotic infections and rare diabetic ketoacidosis. Limb amputations were increased in one trial.
The guidelines recommend treatment with a long-acting glucagon-like peptide-1 (GLP-1) receptor agonist in patients with type 2 diabetes who have not achieved glycemic goals despite use of metformin and an SGLT2 inhibitor or who are unable to use those medications. Some of the GLP-1 receptor agonists have a beneficial effect in reducing cardiovascular events. GLP-1 receptor agonist trials are safe with an eGFR as low as 15 mL per minute per 1.73 m2, where they appear to reduce albuminuria and preserve eGFR. They should not be prescribed with dipeptidyl peptidase-4 inhibitors. They can be used with a sulfonylurea or insulin, although the doses of these medications may need to be reduced.
A1C is imprecise among people treated with dialysis but reasonably accurate with an eGFR of 30 mL per minute per 1.73 m2 or greater. A1C targets may vary from less than 6.5% to less than 8%, depending on patient factors, including risk for hypoglycemia.
Renin-Angiotensin System Inhibition
Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are recommended to slow kidney disease progression in people with albuminuria and hypertension. An ACE inhibitor or ARB should be titrated to maximal tolerated dosage with monitoring of blood pressure, serum potassium, and serum creatinine within two to four weeks of dosing changes. Medications should be reduced or discontinued for symptomatic hypotension, uncontrolled hyperkalemia, creatinine increase of greater than 30%, or acute kidney injury. Combination therapy with ACE inhibitors and ARBs may be harmful and should be avoided. Women prescribed an ACE inhibitor or an ARB should be offered contraceptive advice because of adverse fetal and neonatal effects, especially during the second and third trimesters. Mineralocorticoid receptor antagonists such as spironolactone and eplerenone (Inspra) are useful for resistant hypertension and are being studied in trials evaluating CKD and CVD outcomes.
Antiplatelet Therapy
Aspirin is recommended for secondary prevention of CVD. Primary prevention of CVD with aspirin is not recommended for routine use.
Guideline source: Kidney Disease: Improving Global Outcomes (KDIGO)
Evidence rating system used? Yes
Systematic literature search described? Yes
Guideline developed by participants without relevant financial ties to industry? No
Recommendations based on patient-oriented outcomes? Yes
Published source: Kidney Int. October 2020;98(4S):S1–S115
Editor's Note: KDIGO guidelines are a well-respected international resource for the treatment of CKD. This guideline summary was written by guideline authors, including the two cochairs.
The major recommendation that SGLT2 inhibitors be first-line therapy for diabetes with CKD requires scrutiny. All authors receive funding from companies that market SGLT2 inhibitors, and one receives funding from all four. The National Academy of Medicine recommends that a minority of guideline members have conflicts of interest and that chairs be free of conflicts.1 Conflicts of interest are common in practice guidelines reviewed by AFP. I am pointing out these conflicts of interest because we usually do not accept authors with this level of potential for bias. We are confident that the authors fairly represented the guideline recommendations.
The evidence to support the primary use of SGLT2 inhibitors is strong, with reductions in cardiovascular events, progression of CKD, and mortality.2 However, only 12% of patients with diabetes meet the inclusion criteria for studies that have shown cardiovascular benefits.3 SGLT2 inhibitor use is recommended for patients with diabetes and CKD by guidelines from the Department of Veterans Affairs and Department of Defense (https://www.aafp.org/afp/2020/0915/p378.html), which are free of conflicts of interest.—Michael J. Arnold, MD, Contributing Editor
References
1. Institute of Medicine (US) Committee on Standards for Developing Trustworthy Clinical Practice Guidelines; Graham R, Mancher M, Miller Wolman D, et al., eds. Clinical practice guidelines we can trust. National Academies Press; 2011. Accessed May 7, 2021. https://www.ncbi.nlm.nih.gov/books/NBK209539/
2. Zou C-Y, Liu X-K, Sang Y-Q, et al. Effects of SGLT2 inhibitors on cardiovascular outcomes and mortality in type 2 diabetes: a meta-analysis. Medicine (Baltimore). 2019;98(49):e18245.
3. Wittbrodt ET, Eudicone JM, Bell KF, et al. Eligibility varies among the 4 sodium-glucose cotransporter-2 inhibitor cardiovascular outcomes trials: implications for the general type 2 diabetes US population. Am J Manag Care. 2018;24(8 suppl):S138–S145.
