
Am Fam Physician. 2022;105(4):412-420
Author disclosure: No relevant financial relationships.
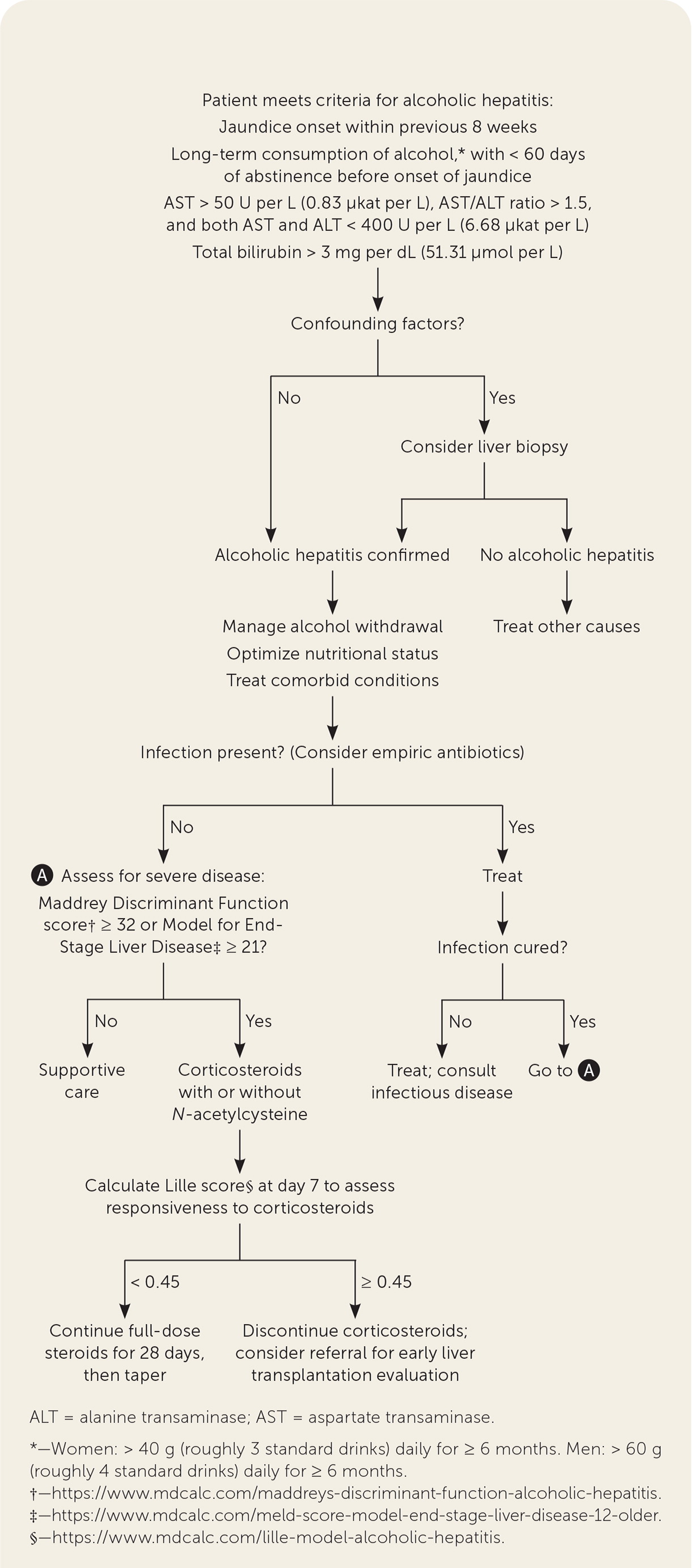
Alcoholic hepatitis is a clinical syndrome characterized by acute-onset jaundice and liver enzyme abnormalities in the setting of long-term heavy alcohol use. High rates of concomitant infections, systemic inflammation, and multiorgan failure lead to significant morbidity and mortality. Diagnosis of alcoholic hepatitis is primarily clinical, based on a consensus definition from the National Institute on Alcohol Abuse and Alcoholism. Initial workup should include chest radiography and cultures of peritoneal fluid, blood, and urine. Close monitoring for inflammation and organ failure is crucial throughout hospitalization. Laboratory-based prognostic scores, including Maddrey Discriminant Function and the Model for End-Stage Liver Disease, help determine disease severity and treatment options. Treatment for moderate disease primarily consists of supportive care, including alcohol cessation and nutritional support. Corticosteroids are recommended for severe alcoholic hepatitis. Responsiveness to corticosteroid therapy should be evaluated using the Lille score on day 7 of treatment. Hospital physicians should involve a multidisciplinary team, including substance abuse specialists, gastroenterologists or hepatologists, nephrologists, dietitians, and intensivists, as appropriate. Long-term follow-up should focus on abstinence from alcohol, management of underlying cirrhosis, and evaluation for liver transplantation if indicated. Pharmacologic treatment of alcohol use disorder can aid patients in maintaining abstinence from alcohol. The presence of underlying cirrhosis and continued alcohol use negatively impact long-term prognosis.
Alcohol-associated liver disease encompasses a range of pathologies from hepatic steatosis to cirrhosis. Decompensated liver disease can manifest as ascites, variceal hemorrhage, hepatic encephalopathy, spontaneous bacterial peritonitis, hepatorenal syndrome, hepatopulmonary syndrome, or hepatocellular carcinoma. Alcoholic hepatitis is a clinical syndrome associated with acute-onset jaundice and liver failure.1 High rates of concomitant infections, systemic inflammation, and multiorgan failure lead to significant morbidity and mortality.
Epidemiology and Risk Factors
The incidence of alcoholic hepatitis is difficult to estimate because of inconsistency in diagnosis of the disease and overlap with concurrent, more easily diagnosed liver diseases, such as hepatitis C.1,2 However, hospital admissions for alcoholic hepatitis are on the rise in the United States, accounting for 0.83% of all admissions in 2010.1 Risk factors for the development of the disease include prolonged and heavy alcohol use, younger age, female sex, genetic susceptibility, higher body mass index, and comorbid liver disease.1,3–5 Overall and in-hospital mortality are high for severe alcoholic hepatitis, with a 28-day mortality rate of 16% to 30% and a one-year mortality rate of 56%.6 The presence of underlying cirrhosis and continued alcohol use negatively impact long-term prognosis.4,7–9
Diagnosis
Because of historical variability in the diagnosis of alcoholic hepatitis, the National Institute on Alcohol Abuse and Alcoholism developed a consensus statement for diagnosing the disease (Table 1).1,7,10 The diagnosis is primarily clinical and must include acute-onset jaundice, specific laboratory abnormalities, and characteristic history of alcohol use (i.e., long-term consumption of roughly three standard drinks daily for women and four standard drinks daily for men). Liver biopsy is necessary only if the diagnosis is unclear and accurate diagnosis would impact management.7,10
| Diagnostic criteria |
| Jaundice onset within previous 8 weeks |
| Long-term consumption of alcohol: > 40 g (roughly 3 standard drinks) daily for women or > 60 g (roughly 4 standard drinks) daily for men for ≥ 6 months, with < 60 days of abstinence before onset of jaundice |
| AST > 50 U per L (0.83 μkat per L), AST/ALT ratio > 1.5, and both AST and ALT < 400 U per L (6.68 μkat per L) |
| Total bilirubin > 3 mg per dL (51.31 μmol per L) |
| Absence of confounding factors |
| Confounding factors |
| Possible ischemic hepatitis (suggested by severe upper gastrointestinal tract bleed, hypotension, cocaine use within seven days of symptom onset) |
| Possible metabolic liver disease (Wilson disease, alpha1-antitrypsin deficiency) |
| Possible drug-induced liver disease (use of offending drug within 30 days of jaundice onset) |
| Uncertain alcohol use assessment (patient denies excessive alcohol use) |
| Atypical laboratory findings (AST < 50 U per L or > 400 U per L, AST/ALT ratio < 1.5, antinuclear antibodies > 1: 160, or anti–smooth muscle antibodies > 1: 80) |
| If diagnostic confirmation would change management in the presence of confounding factors, perform liver biopsy |
CLINICAL PRESENTATION AND LABORATORY FINDINGS
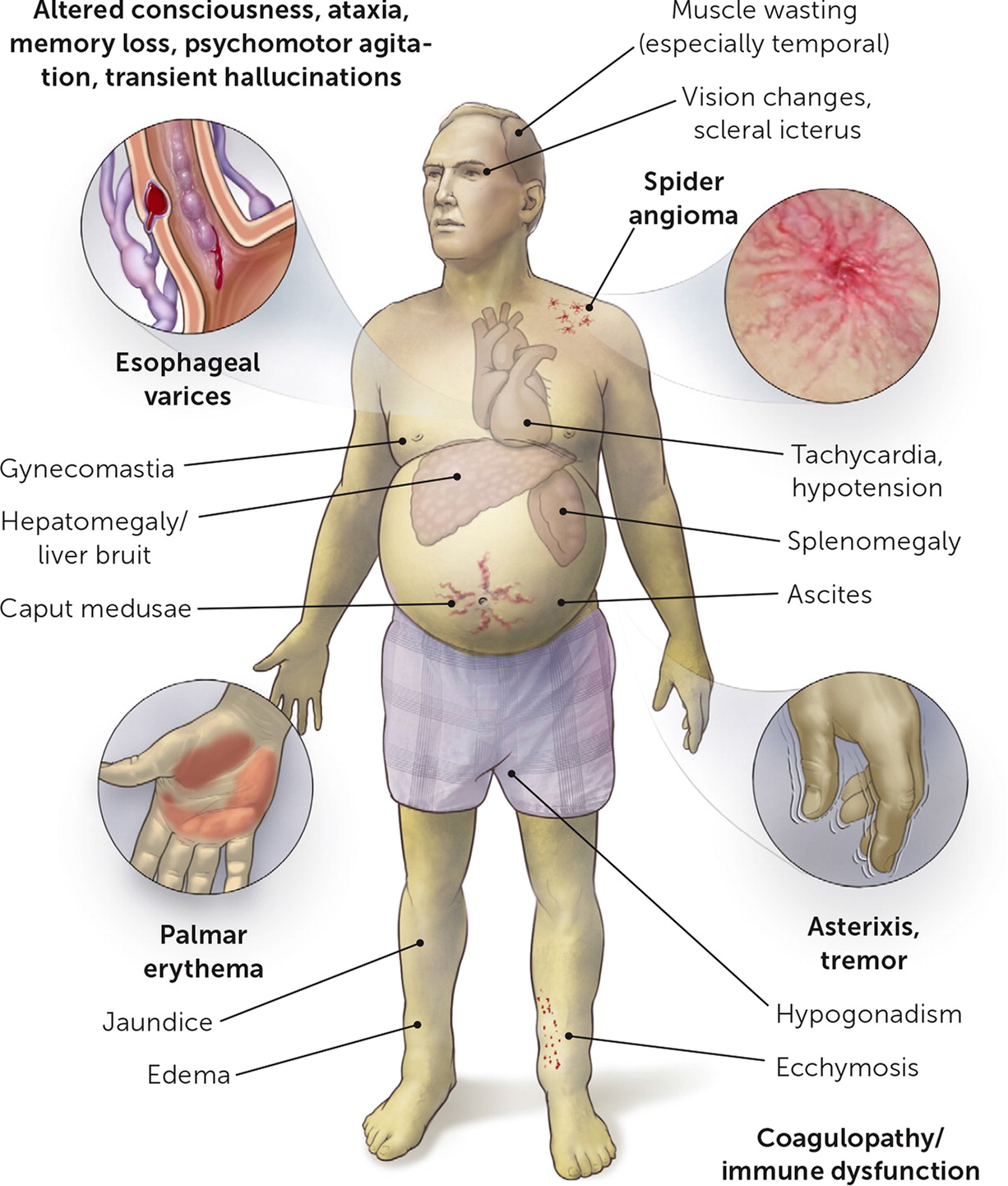
Acute onset of jaundice is the only clinical sign or symptom required for the diagnosis of alcoholic hepatitis.7,10 However, other nonspecific signs and symptoms (Table 21,11,12 and Figure 1) can support the diagnosis of alcoholic hepatitis and suggest underlying chronic alcohol-associated liver disease. Because these signs and symptoms can be subtle, a high index of suspicion is required. Laboratory findings that are diagnostic for alcoholic hepatitis or characteristic of alcohol-associated liver disease are outlined in Table 21,11,12; deviation from the specified diagnostic pattern should prompt consideration of alternative diagnoses.
| Symptoms Abdominal pain (right upper quadrant, epigastric) Anorexia Confusion (encephalopathy) Fatigue Fever Malaise Nausea and vomiting Peripheral neuropathy Sleep-wake inversion Weight gain (ascites) Weight loss (loss of muscle mass, malnutrition) Laboratory tests Diagnostic findings AST > 50 U per L (0.83 μkat per L) AST/ALT ratio > 1.5 AST and ALT < 400 U per L (6.68 μkat per L) Total bilirubin > 3 mg per dL (51.31 μmol per L) Other characteristic findings Decreased serum albumin and prealbumin Elevated gamma-glutamyltransferase Elevated international normalized ratio Elevated white blood cell count with neutrophil predominance Macrocytosis Thiamine deficiency Thrombocytopenia Vitamin B12 and/or folate deficiency |
CHARACTERISTIC ALCOHOL USE HISTORY
Presence of the characteristic alcohol use history is an important component of the clinical diagnosis, and patient reluctance to disclose alcohol use is a significant issue.13 Validated screening tools (Table 310,14–17) and collateral history from family members can aid in identifying high-risk alcohol use.1 The Alcohol Use Disorders Identification Test-Concise screening questionnaire is a more targeted screening tool for identifying alcohol misuse than the CAGE (cut down, annoyed, guilty, eye-opener) questionnaire.14
| Test | Comments |
|---|---|
| Screening questionnaires | |
| Alcohol Use Disorders Identification Test-Concise14 | Three-question screen (frequency of alcohol use, number of drinks in one sitting, frequency of ≥ 6 drinks in one sitting), with tiered point system depending on response; online calculator available at https://www.mdcalc.com/audit-c-alcohol-use Men with a score ≥ 4: sensitivity = 86%, specificity = 89% Women with a score ≥ 3: sensitivity = 73%, specificity = 91% |
| National Institute on Alcohol Abuse and Alcoholism Single Alcohol Screening Question15 | “How many times in the past year have you had five or more drinks in one day (for men) or four or more drinks in one day (for women)?” Sensitivity = 80%, specificity = 74% |
| Biomarkers | |
| Ethyl glucuronide or ethyl sulfate16 | Urine alcohol biomarker that detects use in the preceding three days Prolonged by renal insufficiency Ethyl glucuronide: sensitivity = 76%, specificity = 93% Ethyl sulfate: sensitivity = 82%, specificity = 86% |
| Phosphatidylethanol17 | Blood alcohol biomarker that detects use in the preceding two to three weeks Not affected by age, body mass index, patient sex, kidney disease, or liver disease More costly than urine tests Sensitivity = 100%, specificity = 96% |
RULING OUT CONFOUNDING AND CONCOMITANT DIAGNOSES
Because of significant overlap in presenting symptoms of alcoholic hepatitis and other diagnoses, a thorough history, laboratory studies, and imaging tests should be performed to rule out confounding and concomitant diagnoses (Table 4).1,10,12 Testing for infections is crucial in the initial management of patients with suspected alcoholic hepatitis.1 The disease is most commonly associated with spontaneous bacterial peritonitis, urinary tract infection, pneumonia, enterocolitis, and cellulitis.1,12
| Diagnosis | Tests/findings |
|---|---|
| Autoimmune liver disease | Antinuclear antibodies > 1:160, anti–smooth muscle antibodies > 1:80 |
| Biliary obstruction | Right upper quadrant ultrasonography or abdominal computed tomography with contrast |
| Drug-induced liver injury | Assess for offending drug exposure, including acetaminophen levels, within 30 days of jaundice onset |
| Infection | Blood cultures, chest radiography, peritoneal fluid cultures if ascites is present, urinalysis and urine culture |
| Ischemic hepatitis | Urine drug screening Assess for presence of severe upper gastrointestinal tract bleeding, hypotension, and cocaine use within seven days of symptom onset |
| Metabolic liver disease | Alpha1-antitrypsin deficiency, hemochromatosis (high ferritin level), Wilson disease (low ceruloplasmin level) |
| Viral hepatitis | Viral hepatitis panel |
Risk Stratification
After establishing the diagnosis of alcoholic hepatitis, clinicians should use validated laboratory-based prognostic tools (Table 51,18–24) to determine severity, prognosis, and treatment options. Severe alcoholic hepatitis is defined as a score of at least 32 using the Maddrey Discriminant Function tool (https://www.mdcalc.com/maddreys-discriminant-function-alcoholic-hepatitis) or at least 21 using the Model for End-Stage Liver Disease tool (https://www.mdcalc.com/meld-score-model-end-stage-liver-disease-12-older or https://www.mdcalc.com/meldna-meld-na-score-liver-cirrhosis).7 The Lille score (https://www.mdcalc.com/lille-model-alcoholic-hepatitis) distinguishes patients who would likely be responsive vs. unresponsive to steroids, predicting who could have poorer outcomes if steroid therapy was continued beyond seven days.18
| Score | Components | Thresholds | Clinical significance |
|---|---|---|---|
| Lille Model for Alcoholic Hepatitis | Day 0: age, albumin, INR, creatinine, bilirubin, prothrombin time; day 7: bilirubin (https://www.mdcalc.com/lille-model-alcoholic-hepatitis) | Patient unresponsive to steroids (score ≥ 0.45) | Discontinue corticosteroids at day 718 |
| Maddrey Discriminant Function | Prothrombin time, total bilirubin (https://www.mdcalc.com/maddreys-discriminant-function-alcoholic-hepatitis) | Severe disease (score ≥ 32) | Initiate corticosteroids19 |
| MELD | Bilirubin, creatinine, INR, sodium (https://www.mdcalc.com/meld-score-model-end-stage-liver-disease-12-older) | Severe disease (score ≥ 21) | Initiate corticosteroids Predicts increased risk of in-hospital mortality if increases ≥ 2 in one week20 90-day mortality of 20% (sensitivity and specificity = 75%)21 28-day mortality of 30% to 50% (sensitivity = 86%, specificity = 48%)19,22 |
| MELD-Na | Bilirubin, creatinine, INR, sodium (https://www.mdcalc.com/meldna-meld-na-score-liver-cirrhosis) | Transplant eligible (score ≥ 21) | Refer for liver transplant evaluation |
| Child-Pugh Score for Cirrhosis Mortality | Total bilirubin, albumin, INR, ascites burden, encephalopathy grade (https://www.mdcalc.com/child-pugh-score-cirrhosis-mortality) | Class A: score 5 or 6 Class B: score 7 to 9 Class C: score 10 to 15 | Describes cirrhosis severity; less commonly used for prognosis given the advantages of MELD23 |
Management
Figure 2 is an algorithm for the diagnosis and treatment of alcoholic hepatitis.
ABSTINENCE FROM ALCOHOL
Abstinence from alcohol is the mainstay of treatment. Clinicians should counsel all patients on alcohol cessation, offer medications for alcohol use disorder when appropriate, and consider early consultation with a substance abuse counselor, social worker, and/or psychiatrist, depending on institutional resources.1,25,26 If resources for alcohol use disorder are not readily available, referral to a center with expertise in this disorder should be considered.1,12
During inpatient management, using a structured alcohol withdrawal protocol in conjunction with a standard instrument such as the Clinical Institute Withdrawal Assessment for Alcohol Revised (https://www.mdcalc.com/ciwa-ar-alcohol-withdrawal) to guide benzodiazepine dosing can prevent withdrawal symptoms, including delirium tremens and seizures.27 Because benzodiazepines can precipitate or worsen hepatic encephalopathy and possibly impair liver function, the dosage should be limited to the minimum needed for symptom control.
NUTRITIONAL SUPPORT
Protein-calorie malnutrition is a common comorbidity to alcohol-associated liver disease and alcoholic hepatitis as a result of decreased nutritional intake, decreased gut absorption, and catabolic metabolism. Because poor nutrition is associated with worse outcomes, dietitian consultation should be considered.
Nutritional support can include low-volume intravenous fluids for dehydration; intravenous or oral thiamine to decrease risk of Wernicke encephalopathy; and supplemental folate, vitamin B6, vitamin B12, and zinc for common vitamin deficiencies.1,28 Daily energy intake of 35 to 40 kcal per kg of body weight and daily protein intake of 1.2 to 1.5 g per kg of body weight are recommended.12,25,28–30
Nasogastric tube placement for enteral feedings can be considered if the patient is unable to eat orally; however, this is often poorly tolerated, and oral nutrition is preferred. Parenteral nutrition increases the risk of infection and liver injury, and there is no evidence supporting its use in patients with alcoholic hepatitis.30 As patients with severe malnutrition begin enteral feedings, close attention to electrolyte levels, including sodium, potassium, phosphate, and magnesium, is required to avoid refeeding syndrome, a potentially dangerous shift in fluids and electrolytes.28,30
MEDICATION MANAGEMENT
Given the high rate of concomitant infections in patients with alcoholic hepatitis, it is reasonable to administer broad-spectrum empiric antibiotics while awaiting culture results.1,25 After workup and culture findings rule out alternative diagnoses and any infections have been treated successfully, guidelines support initiating oral corticosteroids (prednisolone, 40 mg per day, or methylprednisolone, 32 mg per day) in patients with severe alcoholic hepatitis. However, the benefit of corticosteroids is questionable, and treatment should be limited to 28 days (with or without taper over three weeks) based on randomized controlled trials and meta-analyses.1,12,22,25,31,32 Corticosteroid use is associated with an increased risk of infections and gastrointestinal hemorrhage and can be harmful if administered to patients with unclear diagnoses, less severe disease, or concomitant infections.1,6,32
Corticosteroid use should be discontinued in patients who do not show an initial response (i.e., Lille score of 0.45 or more on day 7).1,18 If the Lille score suggests responsiveness, the corticosteroid dose should be continued for a total of 28 days and then tapered. One study indicates that a Lille score on day 4 may be as accurate at predicting response to corticosteroids as on day 7.32,33 Corticosteroids are not recommended for patients with moderate alcoholic hepatitis.1,32
Guidelines recommend intravenous N-acetyl-cysteine, 40 mg per day for five days, as an adjunct to corticosteroids in patients with severe alcoholic hepatitis.1,12,25,34 Pentoxifylline is no longer recommended because of a lack of data demonstrating benefit.1,6,12,32 Therapies targeting inflammation and oxidative stress, alcohol use disorder, and gut-liver axis dysfunction have shown early promise in the treatment of alcoholic hepatitis but require further study.8
EARLY LIVER TRANSPLANTATION
There is growing support for early liver transplantation in some patients with severe alcoholic hepatitis, rather than requiring six months of alcohol abstinence and engagement in alcohol cessation counseling. Patients with severe alcoholic hepatitis who are not responding to medical therapy (clinically or by Lille score) or are ineligible for medical therapy and are presenting with alcoholic hepatitis as their first liver-decompensating event may be candidates for early liver transplantation.1,4,12,25,32,35 Assessment should include psychosocial evaluation by a multidisciplinary team, including a social worker, psychiatrist/addiction specialist, mental health professionals, and liver transplant teams, to identify candidates at minimal risk of returning to alcohol use after transplantation.1,4,12,25,35
GUIDELINE-DIRECTED TREATMENT OF COMORBIDITIES AND COMPLICATIONS
Decompensated cirrhosis can precipitate or result from alcoholic hepatitis. Patients should be monitored for signs of decompensation on physical examination and with daily laboratory testing. Table 6 outlines guideline-directed treatment recommendations for comorbidities and complications in patients with alcoholic hepatitis.11,36–40 Early gastroenterology/hepatology, nephrology, intensive care, and palliative care consultations should be obtained as appropriate. Goals of care should be addressed with the patient and family early in the course of illness.
| Condition | Treatment recommendations |
|---|---|
| Acute kidney injury and hepatorenal syndrome | Stop diuretics, beta blockers, nonsteroidal anti-inflammatory drugs, nephrotoxic drugs, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, and vasodilators Albumin (1 g per kg per day titrated to a maximum dosage of 100 g per day) for two days Therapeutic paracentesis for tense ascites with albumin infusion for any volume of fluid For hepatorenal syndrome: vasoactive drugs with albumin infusions Terlipressin (not available in the United States), octreotide (Sandostatin) and midodrine, or norepinephrine Albumin, 20 to 40 g per day Consider TIPS or renal replacement therapy |
| Ascites | Diagnostic paracentesis with blood cell counts, cultures, fluid protein measurement, Serum Ascites Albumin Gradient calculation* Sodium restriction (< 2 g per day) Fluid restriction (1 to 1.5 L per day) if serum sodium < 125 mEq per L (125 mmol per L) Diuretics (spironolactone with or without furosemide [Lasix]) Spironolactone, 100 mg per day initially, then titrate by 100 mg every three days to a maximum dosage of 400 mg per day Furosemide, 40 mg per day titrated to a maximum dosage of 160 mg per day Avoid or adjust for severe hyponatremia (sodium < 125 mEq per L), hypo- or hyperkalemia, acute kidney injury, severe cramps For tense or refractory ascites: therapeutic paracentesis with albumin replacement (6 to 8 g per L of ascites fluid) when 6 L or more is removed Prophylactic ciprofloxacin (400 mg per day) in patients with a Child-Pugh score† ≥ 9 and bilirubin ≥ 3 mg per dL (51.31 μmol per L), impaired renal function or hyponatremia, and ascitic fluid protein < 15 g per L Consider TIPS for recurrent or refractory ascites Treat precipitating factors |
| Hepatic encephalopathy | Lactulose titrated to produce two or three bowel movements per day Rifaximin (Xifaxan); short-term alternatives are neomycin and metronidazole (Flagyl) If patient does not respond to treatment, consider oral branched-chain amino acids or intravenous L-ornithine L-aspartate |
| Spontaneous bacterial peritonitis | Peritoneal and blood cultures before treatment initiation Diagnosis requires peritoneal fluid polymorphonuclear leukocyte count > 250 per mm3 Antibiotics (third-generation cephalosporin; piperacillin/tazobactam [Zosyn] or carbapenems for resistance) Albumin (1.5 g per kg at diagnosis and 1 g per kg on day 3) Prophylactic ciprofloxacin after recovery |
| Variceal hemorrhage | Primary prevention of hemorrhage with nonselective beta blockers Avoid nonselective beta blockers during acute bleed Vasoactive drug therapy (somatostatin or octreotide) for three to five days Endoscopic ligation within 12 hours and after stabilization (preprocedure erythromycin) Antibiotic prophylaxis with ceftriaxone or quinolones for up to seven days Restrictive transfusion strategy with a hemoglobin goal > 7 g per dL (70 g per L) Consider TIPS |
Follow-Up
Ongoing treatment of alcohol use disorder is paramount to long-term survival of patients with alcoholic hepatitis.1,11,25,26 Alcohol rehabilitation is associated with a decrease in hospital readmission, relapse, and mortality.26 In patients who recover from alcoholic hepatitis without residual liver impairment, several medications have demonstrated effectiveness in the treatment of alcohol use disorder, including three that are approved by the U.S. Food and Drug Administration for this indication (acamprosate, disulfiram, and naltrexone [Revia]).1 These therapies are reviewed in a previous American Family Physician article (https://www.aafp.org/afp/2016/0315/p457.html) and editorial (https://www.aafp.org/afp/2019/0615/p733.html). In patients with continued liver impairment, acamprosate and baclofen (Lioresal) can be used based on limited data.1,8,12,25
| Diagnosis of hepatocellular carcinoma |
| Episode of spontaneous bacterial peritonitis |
| Model for End-Stage Liver Disease-Na score ≥ 21 (https://www.mdcalc.com/meldna-meld-na-score-liver-cirrhosis) |
| New-onset decompensation (ascites, encephalopathy, jaundice, or variceal hemorrhage) |
| Patients with alcohol-associated liver disease who do not improve after 3 months of abstinence, especially with a class C (10 to 15 points) Child-Pugh Score for Cirrhosis Mortality (https://www.mdcalc.com/child-pugh-score-cirrhosis-mortality) |
Data Sources: We searched the Cochrane Database of Systematic Reviews, PubMed Clinical Queries (search words: acute hepatitis, alcoholic and diagnosis and disease management), and Ovid (search words: acute hepatitis, alcoholic and diagnosis and disease management). Guidelines were consulted from the American Association for the Study of Liver Diseases, National Institute on Alcohol Abuse and Alcoholism, European Association for the Study of the Liver, American Gastroenterological Association, U.S. Preventive Services Task Force, and European Society for Clinical Nutrition and Metabolism. Reference lists from retrieved sources were also searched. Search dates: April 19, 2021, and February 1, 2022.
