
Am Fam Physician. 2022;105(5):479-486
Author disclosure: No relevant financial relationships.
Tendinopathies of the foot and ankle, including posterior tibial, peroneal, and tibialis anterior, are commonly overlooked by primary care physicians. The posterior tibial tendon is the main dynamic stabilizing muscle of the medial longitudinal arch. Patients who have posterior tibial tendinopathy present with medial ankle pain, pes planovalgus deformity, and a positive too many toes sign. Nonoperative treatment options include support for the medial longitudinal arch and physical therapy focusing on eccentric exercises. Surgical treatment is considered for patients who do not respond to nonoperative treatments after three to six months and is based on the specific stage of tendinopathy. Peroneal tendon disorders are commonly mistaken for or occur concomitantly with lateral ankle sprains. Varus hindfoot is a known risk factor for peroneal tendinopathy. Treatments include immobilization, laterally posted orthotics, and physical therapy for progressive tendon loading. Tibialis anterior tendinopathy presents as anterior ankle and medial midfoot pain and can be diagnosed with a positive tibialis anterior passive stretch test. Initial treatment includes immobilization followed by physical therapy. Surgical debridement can be considered if nonoperative treatment is ineffective.
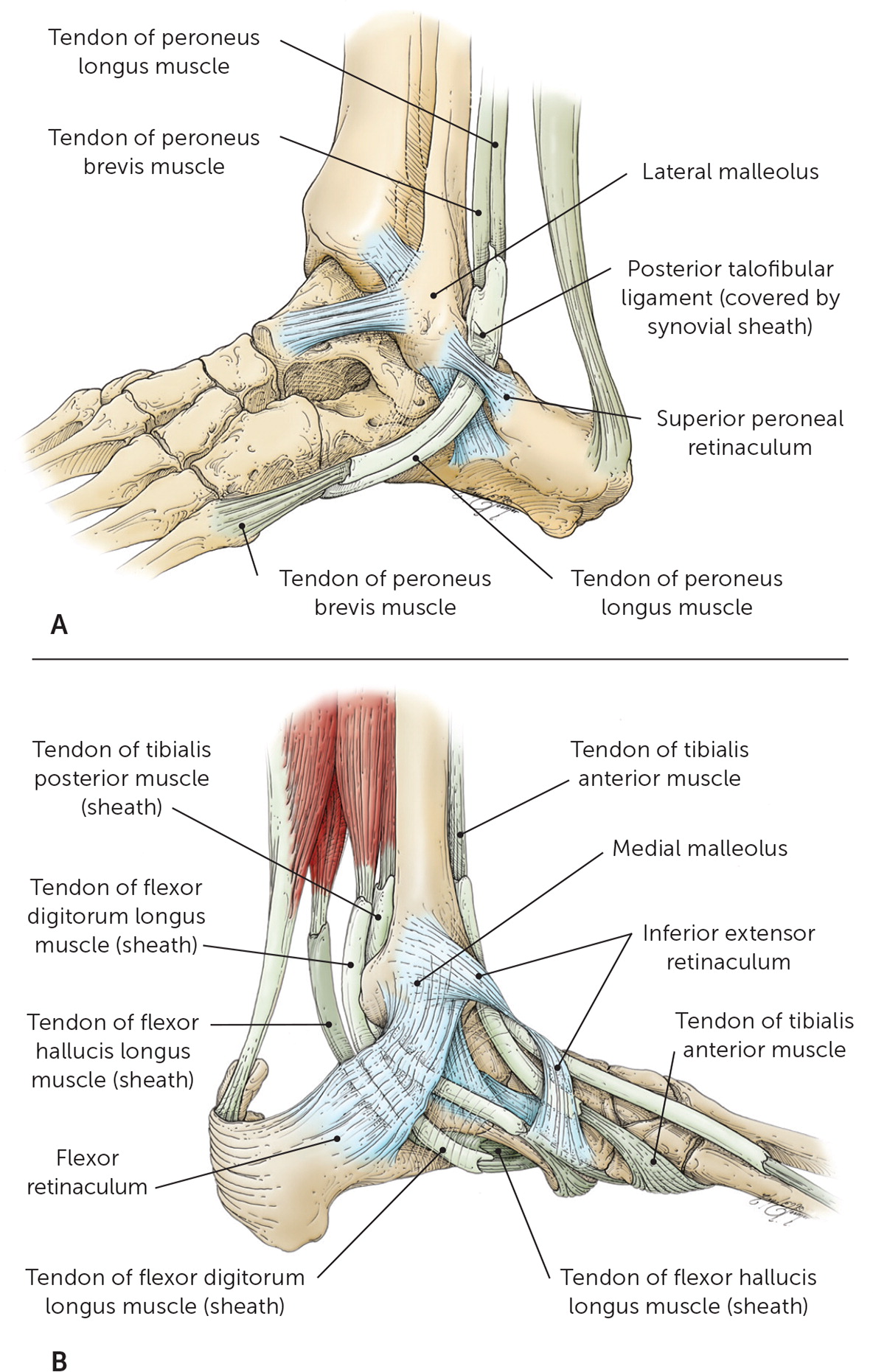
Lower extremity musculoskeletal conditions, such as ankle sprains,1 Achilles tendinopathy,2,3 and plantar fasciitis,3 are commonly diagnosed by primary care physicians, whereas other tendon injuries involving the medial (i.e., posterior tibial), lateral (i.e., peroneal), and anterior (i.e., tibialis anterior) ankle can be missed. The biomechanics of the foot and ankle are intricate. They are responsible for energy absorption and transfer during propulsion, stability during stance, and proprioception. Abnormal mechanics can result in connective tissue changes and alterations in muscle function. Tendinopathy refers to tendon degeneration without substantial inflammation and a generally chronic presentation. The cause of tendinopathy is often multifactorial, involving intrinsic and extrinsic risk factors (Table 1).4–7 The anatomy (Figure 18) and pathophysiology of ankle tendinopathy have been described in detail.2 This article reviews the diagnosis and treatment of posterior tibial, peroneal, and tibialis anterior tendinopathies (Table 2).
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Orthotics may be effective in the early stages of posterior tibial tendinopathy by providing arch support.27 | B | Systematic review, lower-quality studies |
| Eccentric exercises are recommended over concentric exercises for posterior tibial tendinopathy.6,7 | B | Systematic review and case series, lower-quality studies |
| Physicians should screen for peroneal tendinopathy and consider it in the differential diagnosis when evaluating for lateral ankle sprains.31–33 | C | Review, consensus statement, and case series |
| The initial treatment of tibialis anterior tendinopathy involves immobilization or orthotics to assist with dorsiflexion.41 | C | Retrospective case series |
| Intrinsic factors |
| Age-related: decreased healing response, decreased vascularity, increased tendon stiffness, middle age (women), tendon degeneration4,5 |
| Anatomic: eccentric muscle use, imbalance, inflexibility, malalignment, muscle weakness4 |
| Systemic: collagen vascular disease, diabetes mellitus, gout, hypertension, inflammatory enthesophytes, obesity, smoking4–7 |
| Extrinsic factors |
| Corticosteroid exposure, improper activity or exercise form, inappropriate use of equipment, lack of protective gear, mechanical overload4 |
| Condition | Diagnosis | Physical examination | Treatment |
|---|---|---|---|
| Posterior tibial tendinopathy | Pain around the posteromedial ankle that radiates along the arch of the foot; pain worsened with weight-bearing activity | Pes planovalgus deformity; positive too many toes sign; pain or inability to perform single-limb heel raise; pain or weakness with resisted inversion of plantar-flexed foot | Activity modification; arch support (taping, orthotics, a brace with air cell to lift arch); immobilization with walking boot; physical therapy (eccentric exercises) |
| Peroneal tendinopathy | Peroneal brevis pain posterior to the lateral malleolus; peroneal longus pain distal at the lateral cuboid | Hindfoot varus; pain with passive stretch in inversion and dorsiflexion; pain or weakness with active resisted eversion and plantar flexion | Activity modification; orthotics (lateral hindfoot post, lateral forefoot wedge); immobilization with walking boot; physical therapy; corticosteroid injections |
| Tibialis anterior tendinopathy | Pain over the anterior ankle and medial midfoot | Pain with resisted dorsiflexion; positive tibialis anterior passive stretch | Activity modification; immobilization with walking boot; ankle-foot orthosis for dorsiflexion; physical therapy |
Diagnosis and Treatment: General Considerations
HISTORY AND PHYSICAL EXAMINATION
Components of the history for foot and ankle tendinopathies include asking about previous or new activity level, location of pain, timing of pain in relation to activity or rest, swelling, and aggravating and relieving factors. Commonly, patients report starting a new physical activity or increasing the intensity of an existing activity, leading to overuse injuries. Patients may experience pain over the involved tendon with activity, which can progress to pain at rest. Physical examination should be bilateral noting any asymmetry. Possible findings include the presence of swelling and tenderness over the involved tendon and pain with tendon activation. Passive range of motion and strength deficits should be assessed. During weight-bearing, the arch type and overall foot and ankle alignment can be noted. A video of a complete foot and ankle examination is available.
IMAGING
Imaging is generally not necessary unless trauma is suspected. For chronic tendinopathy (i.e., more than six weeks' duration), radiography should be considered as the initial imaging study.9 It can identify bony abnormalities that may be contributing to the patient's symptoms. Further imaging with ultrasonography or magnetic resonance imaging can be performed if the diagnosis is unclear or nonoperative treatment is ineffective. Ultrasonography has become more readily available and is a less expensive alternative to magnetic resonance imaging. An added benefit of ultrasonography is its dynamic nature, enabling evaluation of abnormal motion or subluxation.10 If ultrasonography is unavailable, magnetic resonance imaging can be obtained if surgery is being considered.
TREATMENT
Although chronic tendinopathies are not inflammatory processes,2 short-term use of acetaminophen and nonsteroidal anti-inflammatory drugs can help provide pain relief. However, they can alter tendon and skeletal muscle extracellular matrix remodeling, which may interfere with recovery.11 It is necessary to address footwear, including high heels or worn-out athletic shoes, and over-the-counter orthotics that can help correct arch deficits. Pain with ambulation can be treated with short-term immobilization.12 Rehabilitation should focus on eccentric exercises13 and foot intrinsic muscles.12 Topical low-dose nitroglycerin patches, studied in the setting of Achilles, rotator cuff, and patellar tendinopathies, produced improvements in pain, strength, and patient satisfaction for up to six months in the treatment of those tendinopathies,14 but headaches are a common adverse effect that may limit their use.15 If pain and function do not improve after eight to 12 weeks of treatment, minimally invasive procedures can be used.
Corticosteroid injections have shown effectiveness in the short-term, but there is concern that they can weaken the tendon structure and increase the likelihood of rupture, especially if the corticosteroid is injected into the tendon.16 It is prudent to limit corticosteroid treatment to a single injection. A six-year retrospective review of 109 corticosteroid injections in 96 patients reported only one tendon rupture in patients who received corticosteroid injections into the peroneus tendon sheath,17 and a systematic review of randomized controlled trials with more than 2,600 participants resulted in one tendon rupture.16
Newer treatments have marginal evidence of effectiveness for common foot and ankle abnormalities, including Achilles tendinopathy and plantar fasciitis,18,19 but the benefits for other foot and ankle tendinopathies are unclear. Despite limited evidence, these treatments may be considered as second-line options and include prolotherapy,20 platelet-rich plasma injections,21–23 shockwave therapy,24,25 and needle tenotomy.26 These treatments are often accompanied by rehabilitation.
Foot and Ankle Tendinopathies
POSTERIOR TIBIAL TENDINOPATHY
The function of the posterior tibial tendon is to plantar flex and invert the ankle. It is the main dynamic stabilizing tendon of the medial longitudinal arch,27 absorbing shock during heel strike, stabilizing the foot during midstance, and generating force during heel lift and toeoff.12 Factors associated with posterior tibial tendinopathy include overuse and overload in the setting of hypovascularity, high body mass index, hypertension, diabetes mellitus, collagen vascular disease, corticosteroid exposure, and excessive pronation; the condition is common in women with obesity between 40 and 60 years of age.4–6
The Johnson and Strom classification was the first to categorize posterior tibial tendon dysfunction (Table 3).28 During the early stages of posterior tibial tendinopathy, there is no deformity and pain occurs around the posteromedial ankle and radiates along the arch of the foot. As it progresses, individuals develop pes planovalgus deformity caused by complete loss or collapse of the medial longitudinal arch, and pain on the lateral aspect with impingement of the lateral structures.5 Pain is worse with weight-bearing.

| Variable | Stage I (mild, medial pain) | Stage II (moderate, medial pain) | Stage III (severe, medial and lateral pain) |
|---|---|---|---|
| Swelling and tenderness | Mild swelling and tenderness along posterior tibial tendon | Moderate swelling and tenderness along the posterior tibial tendon | Not much swelling, but marked tenderness along posterior tibial tendon |
| Single-leg heel raise | Mild weakness | Marked weakness | Marked weakness |
| Too many toes sign | Absent | Present | Present |
| Deformity | Absent | Present (flexible) | Present (fixed) |
| Pathologic features | Normal tendon length, paratendinitis (tendon sheath involvement) | Elongated with longitudinal tears | Disrupted with visible tears |
| Images | No changes | Gross deformity | Deformity and diffuse arthritic change |
| Treatment | Nonoperative, tenosynovectomy | Flexor digitorum longus transfers | Arthrodesis, either subtalar or a triple fusion procedure of the subtalar talonavicular and calcaneocuboid joints |
The physical examination begins with the patient standing and the examiner observing alignment from behind. Figure 2 demonstrates notable findings, including pes planovalgus deformity, a positive too many toes sign, and heel valgus. Functional testing includes performing single-limb heel raises. See a video showing single-limb heel raises to test for posterior tibial tendinopathy. The patient should be able to perform five to 10 single-limb heel raises without difficulty.5 Visual inspection and palpation may find swelling and tenderness along the course of the tendon, proximal to the distal attachment on the navicular tuberosity.12 Pain or weakness can be tested with resisted inversion of a plantar flexed foot.

Single-Limb Heel Raises
Untreated posterior tibial tendinopathy may progress to or worsen painful flatfoot, requiring extensive surgical reconstruction. Initial treatment for posterior tibial tendinopathy in the acute stage involves ice, nonsteroidal anti-inflammatory drugs, and activity reduction. Support for the medial longitudinal arch can be provided through taping, orthotics, or a brace with an air cell to lift the arch.6,12,27 Immobilization with a walking boot can be used for severe, acute cases. Studies have shown benefit from stretching and strengthening exercises, and eccentric exercises are recommended over concentric6,7,29 (Figure 3). See a video showing eccentric exercises for posterior tibial tendinopathy.
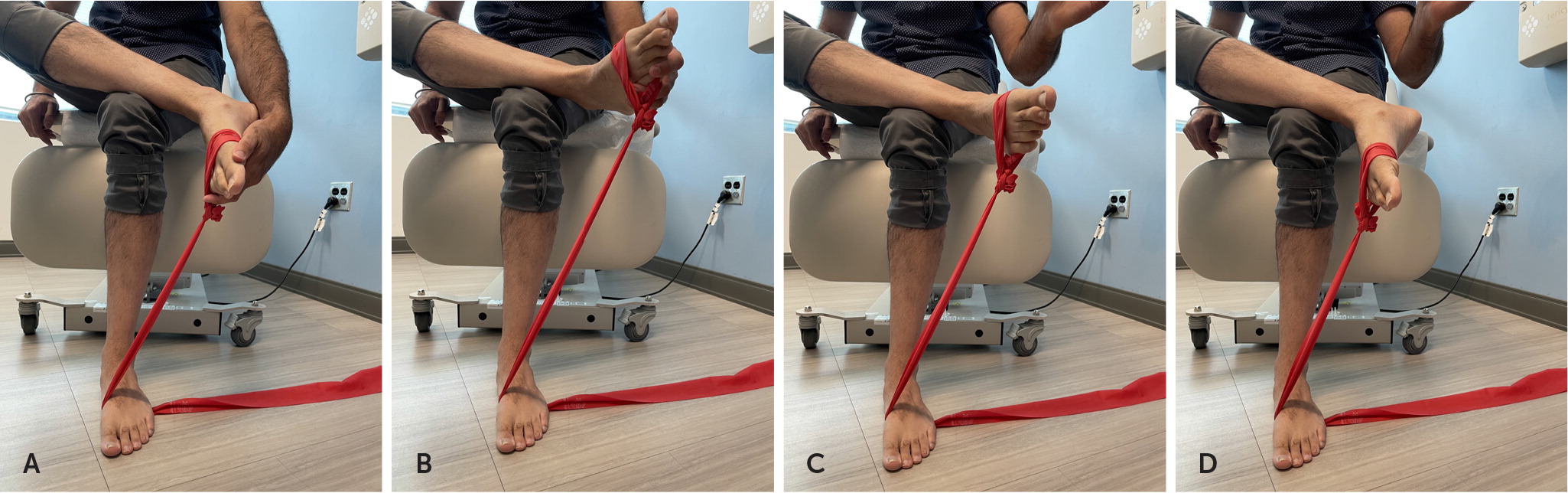
Eccentric Exercises for Posterior Tibial Tendinopathy
Surgical treatment is considered in patients when three to six months of nonoperative treatment is ineffective. In Stage I posterior tibial tendinopathy, debridement with or without tenosynovectomy of the posterior tibial tendon is performed. There is no consensus regarding a single surgical option for Stage II, but treatments include combined soft tissue and bony procedures. A retrospective review of studies with 10-year follow-up of postoperative patients with Stage II posterior tibial tendinopathy found that 86% of patients were totally satisfied with surgery or satisfied with minor reservations.30 Stage III posterior tibial tendinopathy involves arthrodesis, either subtalar or a triple fusion procedure of the subtalar talonavicular and calcaneocuboid joints.
PERONEAL TENDINOPATHY
Peroneal tendinopathy is an under-recognized cause of lateral hindfoot pain and can go undiagnosed, especially when associated with lateral ankle sprains.31,32 Physicians should screen for peroneal tendinopathy and consider it in the differential diagnosis when evaluating for lateral ankle sprains. With ankle inversion injuries, the peroneal tendons can be injured when only one lateral ankle ligament is sprained.33 There are two lateral peroneal tendons, the brevis and longus, acting as primary ankle evertors and assisting with plantar flexion. The brevis is more typically injured. Varus hindfoot is a known risk factor for peroneal tendinopathy.34–37 A forefoot striking pattern is associated with increased stress to the ankle,38 which may lead to peroneal tendinopathy, particularly in runners.33
Physical examination begins with the patient standing to assess hindfoot varus and watch for repetitive visible peroneal tendon contractions while the patient is balancing.34 Pain can be induced with passive stretch in inversion and dorsiflexion, whereas pain and weakness may be appreciated with resisted eversion and plantar flexion. Subluxation of the peroneal tendons over the lateral malleolus with circumduction of the ankle should be assessed. The peroneal compression test (Figure 4) should be performed by palpating for pain along the fibular groove while resisting ankle plantar flexion and eversion.36,39 See a video showing the peroneal compression test.

Peroneal Compression Test
Most peroneal tendinopathies respond to nonoperative treatment, including activity modification, bracing, and physical therapy with early range of motion, progressive tendon loading, and proprioception.34,39 Orthotics to offload the peroneal tendons include a lateral wedge under the heel or a recessed depression for the first metatarsal head to increase foot valgus. A heel cushion can be used for comfort.37 Despite concerns about tendon rupture, corticosteroid injections in the peroneal tendon sheath have been shown to be safe and modestly effective, especially when performed with ultrasound guidance,40 with longer symptom duration being associated with a shorter period of relief.17 Patients with refractory pain, inability to bear weight past one to two weeks after injury, complete tears, and dislocations should be referred to an orthopedic specialist.31,32,36
TIBIALIS ANTERIOR TENDINOPATHY
The tibialis anterior tendon acts to dorsiflex and invert the foot and to eccentrically contract during heel strike to midstance in the gait cycle to control the forefoot contacting the ground. Patients with tibialis anterior tendinopathy present with anterior ankle and medial midfoot pain, most commonly at night, but also with activity.41 Tibialis anterior tendinopathy commonly occurs in women who are overweight or in active individuals, including runners, because of overuse secondary to increases in training mileage or addition of hills to the route.41 Patients exhibit tenderness to palpation over the distal tibialis anterior tendon, with possible swelling. Anterior ankle pain is elicited with resisted dorsiflexion. The tibialis anterior passive stretch test is positive when passive plantar flexion, hindfoot eversion, midfoot abduction, and pronation aggravate or reproduce symptoms41 (Figure 5). See a video showing the passive stretch test of the peroneal tendon. Initial treatment involves immobilization or an ankle-foot orthotic to assist with dorsiflexion.41 Surgical debridement can be considered if nonoperative treatment is ineffective. Surgical debridement has been successful when implemented between five and 25 months after onset of symptoms.42

Passive Stretch of the Peroneal Tendon
This article updates a previous article on this topic by Simpson and Howard.8
Data Sources: We searched the PubMed and Ebsco Host databases with Essential Evidence Plus for the following keywords: posterior tibial tendinopathy; tendinopathies of the foot and ankle; eccentric exercises in foot and ankle; platelet-rich plasma and foot and ankle; tendinopathy; corticosteroid injection and tendon rupture; foot ankle tendinopathy; tibial anterior tendinopathy; ankle tendinopathy and shock wave therapy or PRP or tenotomy or nitroglycerine or prolotherapy or rehabilitation; ankle tendinopathy and imaging or MRI or ultrasound or xray; ankle tendinopathy and treatment peroneal tendinopathy and peroneal tendinosis; flexor hallucis tendinopathy and flexor hallucis tendinosis and dancers tendinitis; peroneal tendon and cortisone or PRP or shock wave therapy or nitroglycerine or orthotics; and FHL and cortisone or PRP or shock wave therapy or nitroglycerine or orthotics. Search dates: February 14, 2021; April 20, 2021; May 1, 2021; May 31, 2021; June 6, 2021; and July 11, 2021.
The authors thank Jenni Weems, MS; Kerry Kennedy, BA; and Rachel Box, MS, of the editorial services group at The Johns Hopkins Department of Orthopaedic Surgery for their editorial assistance with this manuscript.
