
Am Fam Physician. 2023;108(4):337-340
Author disclosure: No relevant financial relationships.
Many family physicians are familiar with the U.S. Preventive Services Task Force (USPSTF) evidence-based recommendations for clinical preventive services. However, they may not be aware of the Community Preventive Services Task Force (CPSTF), which differs from USPSTF in its focus on population health. Family physicians know that health is improved by interventions outside the examination room that impact social, behavioral, environmental, and community factors. CPSTF evaluates evidence and recommends effective interventions to improve health in the community, home, school, work, and health care settings. Systematic evidence reviews form the basis for these recommendations, which target upstream structural, economic, and social factors that affect health outcomes.
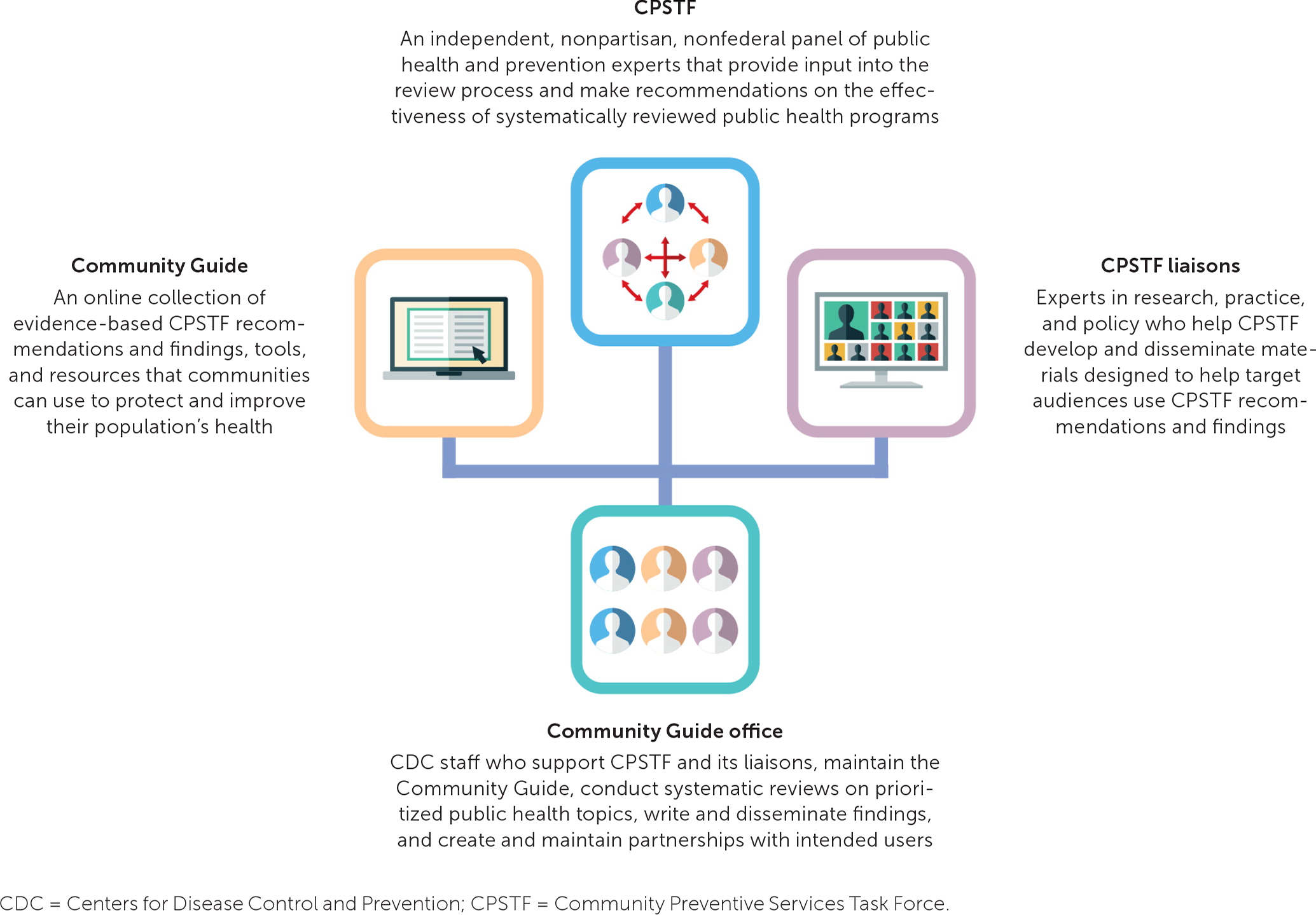
CPSTF, established by the U.S. Department of Health and Human Services in 1996, is an independent, nonfederal panel of 15 experts in public health and prevention, with broad geographic representation and training in medicine, public health, nursing, and behavioral health. Task force members are appointed by the director of the Centers for Disease Control and Prevention (CDC) for five-year terms. CDC staff provide scientific and administrative support to CPSTF, and 32 liaison organizations provide scientific input and facilitate dissemination and translation of CPSTF findings. Liaison organizations include federal agencies and other national organizations focused on health, including primary care organizations (e.g., American Academy of Family Physicians [AAFP], American Academy of Pediatrics). Figure 1 illustrates these collaborative relationships.1
Every five years, CPSTF chooses priority topics that guide the selection of evidence reviews.2 Nine priority topics for 2020 to 2025 were selected through a review of Healthy People 2020 goals and nominations from liaisons and the public. fte topics are heart disease and stroke prevention; injury prevention; mental health; nutrition, physical activity, and obesity; preparedness and response; social determinants of health (SDOH); and substance use, tobacco use, and violence prevention. Within each priority area, CPSTF applies a health equity lens to the selection and evaluation of interventions.3
CPSTF recommendations often address interventions in community settings, including schools, worksites, or homes. In some cases, community-based interventions have more evidence of beneTht. For example, the CPSTF evaluation of interventions to prevent and manage obesity found insuffcient evidence for six interventions conducted in health care settings (e.g., education, feedback, reminders, offce systems to change practice and assist patients) but found suffcient or strong evidence for three school-based interventions (e.g., increase healthier food and beverage options in schools, with or without physical activity) and five community-based interventions (e.g., behavioral interventions to reduce sedentary screen time in children, worksite programs, technology-supported coaching).4 Outcomes for all types of interventions included weight loss and reduced weight gain.
All CPSTF recommendations are provided in The Community Guide, an online resource of interventions to improve health.5 Table 1 lists interventions recommended by the CPSTF in the past six years.5 the interventions are presented in three groups: clinician-provided or health system–based, school-based, and community-based. In health care settings, for example, older adults presenting to the offce with hypertension and diabetes mellitus may benefit from team-based care, digital health interventions to assist with blood pressure self-management and increased physical activity, and community health workers supporting blood pressure and blood glucose control.
| Intervention | Year |
|---|---|
| Clinician-provided or health systems–based | |
| Cancer screening | |
| Patient navigation services to increase breast, cervical, or colorectal cancer screening | 2022 |
| Interventions engaging community health workers to increase breast, cervical, or colorectal cancer screening | 2019 |
| HIV prevention | |
| Digital health interventions to improve adherence to HIV pre-exposure prophylaxis | 2021 |
| Partner services interventions to increase HIV testing | 2021 |
| Clinical decision support system to increase HIV screening | 2020 |
| Chronic disease prevention and management | |
| Team-based care to improve blood pressure control | 2020 |
| Tailored pharmacy-based interventions to improve medication adherence | 2019 |
| Digital health interventions for adolescents who are overweight or obese | 2019 |
| Digital health interventions for adults 55 years and older to increase physical activity | 2019 |
| Exercise programs to prevent gestational hypertension | 2019 |
| Lifestyle interventions to reduce the risk of gestational diabetes | 2017 |
| Activity monitors to increase physical activity for adults who are overweight or obese | 2017 |
| Cell phone apps within health care systems for self-management of type 2 diabetes mellitus | 2017 |
| Comprehensive telehealth interventions to improve diet for patients with chronic diseases | 2017 |
| Text messaging interventions for medication adherence among patients with chronic diseases | 2017 |
| Interactive digital interventions for self-management of blood pressure | 2017 |
| Engagement of community health workers to help patients manage type 2 diabetes | 2017 |
| Mobile health interventions for treatment adherence in those with newly diagnosed heart disease | 2017 |
| Tobacco | |
| Text messaging interventions for tobacco cessation | 2020 |
| School-based | |
| Tobacco | |
| Internet-based interventions for tobacco cessation | 2019 |
| Nutrition and physical activity | |
| Healthy school meals for all programs | 2022 |
| Classroom-based physical activity interventions | 2021 |
| Meal interventions or fruit and vegetable snacks combined with physical activity | 2018 |
| Gardening interventions to increase vegetable consumption among children | 2017 |
| Mental health | |
| School-based antibullying interventions | 2021 |
| School-based cognitive behavior therapy (universal or targeted) to reduce depression and anxiety symptoms | 2019 |
| Asthma | |
| School-based self-management interventions for children and adolescents with asthma | 2019 |
| Community-based | |
| Nutrition and physical activity | |
| Home-based exercise interventions for adults 65 years and older | 2022 |
| Home-delivered and congregate meal services for older adults | 2021 |
| Park, trail, and greenway infrastructure combined with additional interventions | 2021 |
| Digital health and phone interventions to increase healthy eating and physical activity among students at institutions of higher education | 2021 |
| Worksite digital health and phone interventions to increase healthy eating and physical activity | 2021 |
| Community-based digital health and telephone interventions to increase healthy eating and physical activity | 2020 |
| Interventions to increase active travel to school | 2018 |
| Social determinants of health | |
| Tenant-based housing voucher programs | 2020 |
| Permanent supportive housing with housing first | 2019 |
| Violence prevention | |
| Primary prevention interventions to reduce intimate partner violence and sexual violence among youth | 2018 |
Although physicians traditionally have limited themselves to clinical settings, family physicians can play an important role in advocating for policies to improve health through school- and community-based interventions. Recommendations on a range of topics, such as pregnancy, mental health, vaccination rates, and SDOH, are listed in What Works Fact Sheets at https://www.thecommunityguide.org/pages/what-works-fact-sheets.html. Family physicians can advocate for CPSTF-recommended school-based cognitive behavior therapy to reduce student depression and anxiety; healthy school meals for all (interventions to increase participation in school meal programs that reduce food insecurity and school absenteeism); andtenant-based housing voucher programs to improve housing quality, access to health care, and physical and mental health.
Since its inception, the CPSTF has prioritized health equity and SDOH. In 2022, the CPSTF reiterated this commitment and adopted specific goals to consider health equity in the processes of topic prioritization, evidence evaluation, and evidence translation and to emphasize CPSTF membership diversity.3
AAFP, a liaison organization to CPSTF, recognizes the importance of addressing SDOH to advance health equity and acknowledges the contributions of poverty, systemic racism, and discrimination to health inequities.6 There is extensive overlap between the goals of family medicine and those of public health; family physicians are key in improving community health.6 AAFP encourages family physicians to incorporate SDOH in their work by addressing the social needs of individual patients, creating a practice culture that values health equity and supports cultural proficiency, learning about organizations working to improve health equity in their community, and advocating for public policies that improve SDOH and reduce health inequities.6 The EveryONE Project guide to physician advocacy describes how to promote health equity by detecting disparities, identifying root causes, and promoting policy solutions.7
The CPSTF Community Guide is a valuable resource for family physician advocates seeking concrete examples of interventions that improve health and equity.
Editor's Note: Dr. Melnikow is a member of the CPSTF.
