
Am Fam Physician. 2023;108(6):online
Author disclosure: No relevant financial relationships.
A 71-year-old man presented with a persistent dry cough that had been gradually worsening over the past 30 years. The cough was worse at night, especially while lying flat. He was treated with famotidine for gastroesophageal reflux disease (GERD) and completed a trial of albuterol, without improvement. After a two-week course of omeprazole, the patient perceived moderate improvement in his cough, but it persisted at night. The patient had no other gastrointestinal, cardiac, or respiratory symptoms. He did not have sick contacts, fever, chills, myalgias, headaches, chest pain, fatigue, rash, or dyspnea. He had a history of smoking, seasonal allergies, and eczema. He was not a current smoker.
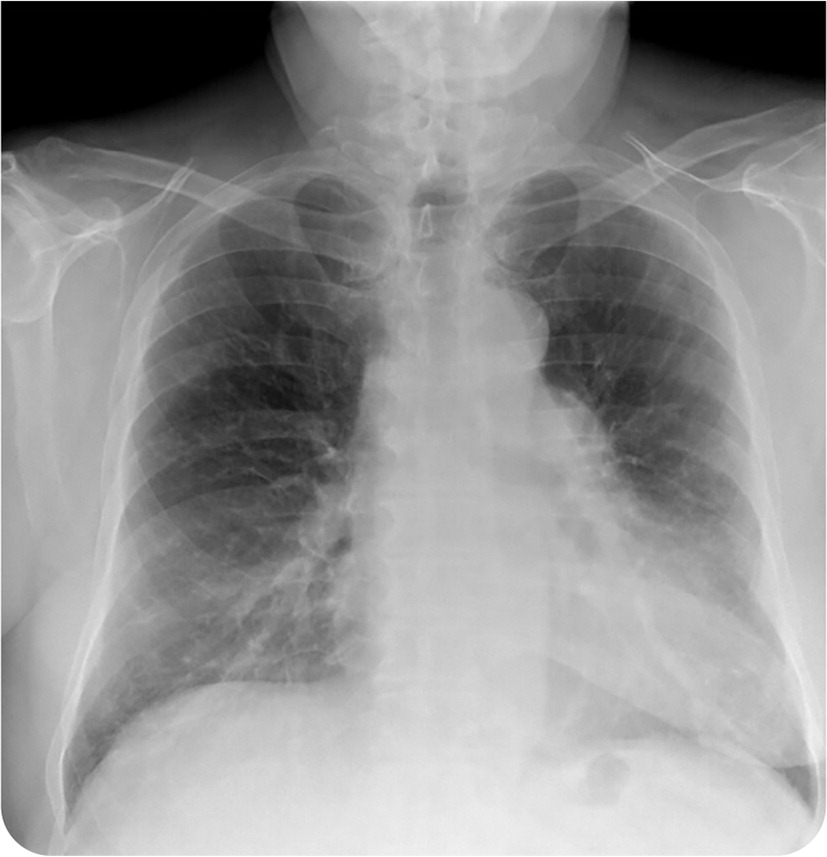
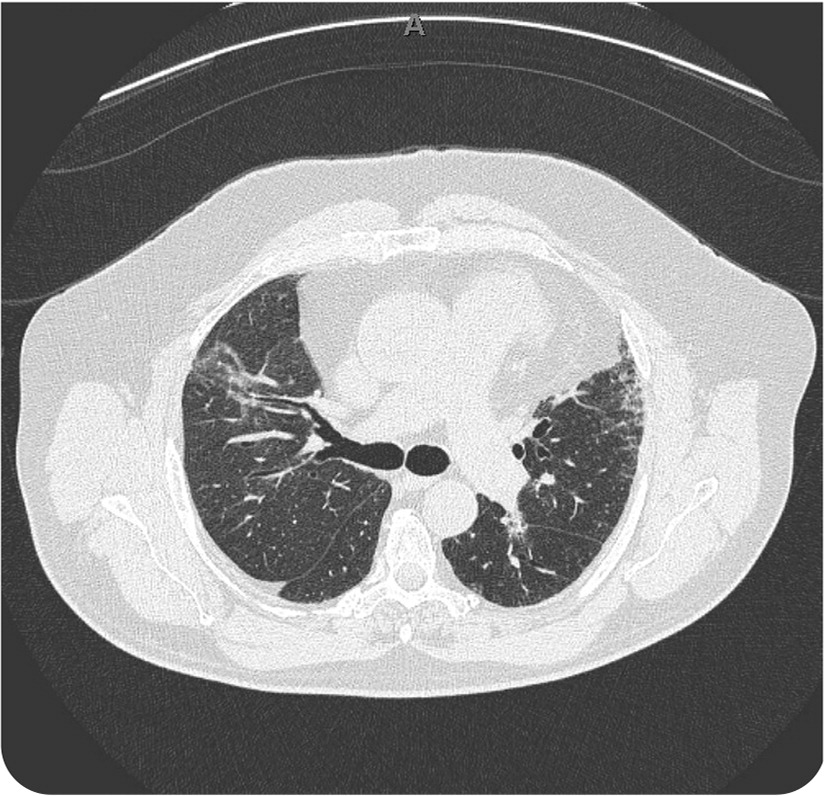
On examination, the patient was afebrile and normotensive. He had a body mass index of 38 kg per m2 (class 2 obesity) and an oxygen saturation of 92% on room air. He had normal respiratory effort but decreased aeration in the bilateral lung bases. The rest of the physical examination was unremarkable. Chest radiography and subsequent computed tomography (CT) were performed (Figure 1 and Figure 2).
Question
Based on the patient’s history and physical examination findings, which one of the following is the most likely diagnosis?
A. Chronic obstructive pulmonary disease.
B. Desquamative interstitial pneumonia.
C. Idiopathic pulmonary fibrosis.
D. Sarcoidosis.
Discussion
The answer is C: idiopathic pulmonary fibrosis. The patient showed significant improvement after two weeks of treatment with a proton pump inhibitor. A correlation has been shown between GERD and the development of idiopathic pulmonary fibrosis. Idiopathic pulmonary fibrosis is a chronic, progressive disease characterized by the deposition of fibrotic tissue in the pulmonary interstitium, without a clear pathophysiologic mechanism. Animal studies have shown that chronic aspiration leads to pulmonary inflammation and fibrosis.1–3 Gastric contents, such as pepsin and bile acid, has been found on broncho-alveolar lavage in patients with idiopathic pulmonary fibrosis.4,5
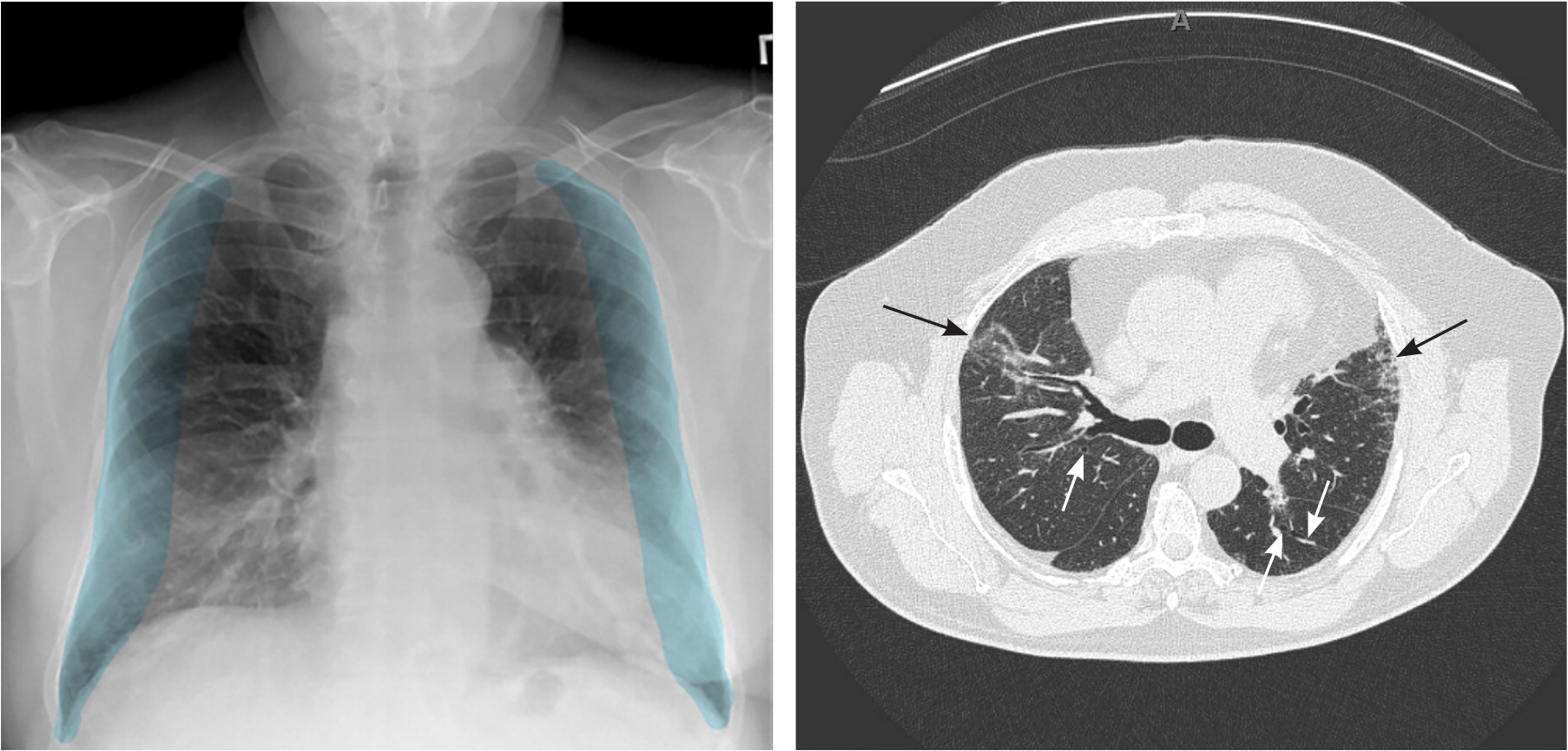
Chest radiography of patients with pulmonary fibrosis shows reticular shadowing of the lung peripheries, predominantly in the lung bases (Figure 3A). High-resolution CT is needed for diagnosis, with findings typically characterized by bilateral reticular opacities, honeycombing, and architectural distortion of the subpleural lung regions and lower lobes6 (Figure 3B).
Chronic obstructive pulmonary disease (COPD) is an obstructive lung disease, unlike the other diagnoses, which are restrictive disorders. COPD is characterized by dyspnea, chronic cough, and sputum production. Chest radiography shows a flattened diaphragm, hyperexpanded lungs, decreased vasculature at the bases, and possible bullae associated with emphysema. CT can show the extent of emphysema. Spirometry is the diagnostic standard for COPD.
Desquamative interstitial pneumonia is a subtype of interstitial lung disease correlated with heavy smoking. It is characterized by macrophages accumulating in the alveolar spaces, leading to interstitial inflammation and fibrosis.7 Findings on chest radiography are normal in up to 20% of patients with this condition. Chest CT shows ground-glass opacities without the peripheral reticular opacities seen with typical interstitial pneumonia.8
Sarcoidosis, a subset of interstitial lung disease, is an inflammatory granulomatous disease of unknown etiology that can cause fibrocystic architectural distortion of the lungs. It is characterized by bilateral hilar adenopathy and pulmonary reticular opacities in the upper lung zone, and may involve the skin, joints, or eyes. The presence of small nodules in a perilymphatic distribution is the key finding on CT.9
| Condition | Chest radiography findings | Computed tomography findings |
|---|---|---|
| Chronic obstructive pulmonary disease | Flattened diaphragm, hyperexpanded lungs, decreased vasculature at the lung bases | Extent of emphysema |
| Desquamative interstitial pneumonia | Findings are minimal or absent | Ground-glass opacities without peripheral reticular opacities |
| Idiopathic pulmonary fibrosis | Reticular shadowing of the lung peripheries, predominantly in the lung bases (Figure 3A) | Bilateral reticular opacities, honeycombing, and architectural distortion of the subpleural lung regions and lower lobes (Figure 3B) |
| Sarcoidosis | Bilateral hilar adenopathy and pulmonary reticular opacities in the upper lung zone | Small nodules in a perilymphatic distribution |
