
Am Fam Physician. 2024;109(1):85-86
Author disclosure: No relevant financial relationships.
A 26-year-old man presented to the emergency department after having a five-minute tonic-clonic seizure. He was postictal for less than one hour and then returned to his baseline. Over the previous two days, he had experienced a mild diffuse headache and an intermittent blind spot in the center of his vision. For the previous three weeks, he had noticed left upper extremity weakness and dexterity issues in his left hand occurring after intense sessions of upper extremity weight lifting. He also reported having a lesion on his back that had been slowly growing for more than one year and occasionally bled. Otherwise, the patient appeared healthy. He had no history of recent travel.
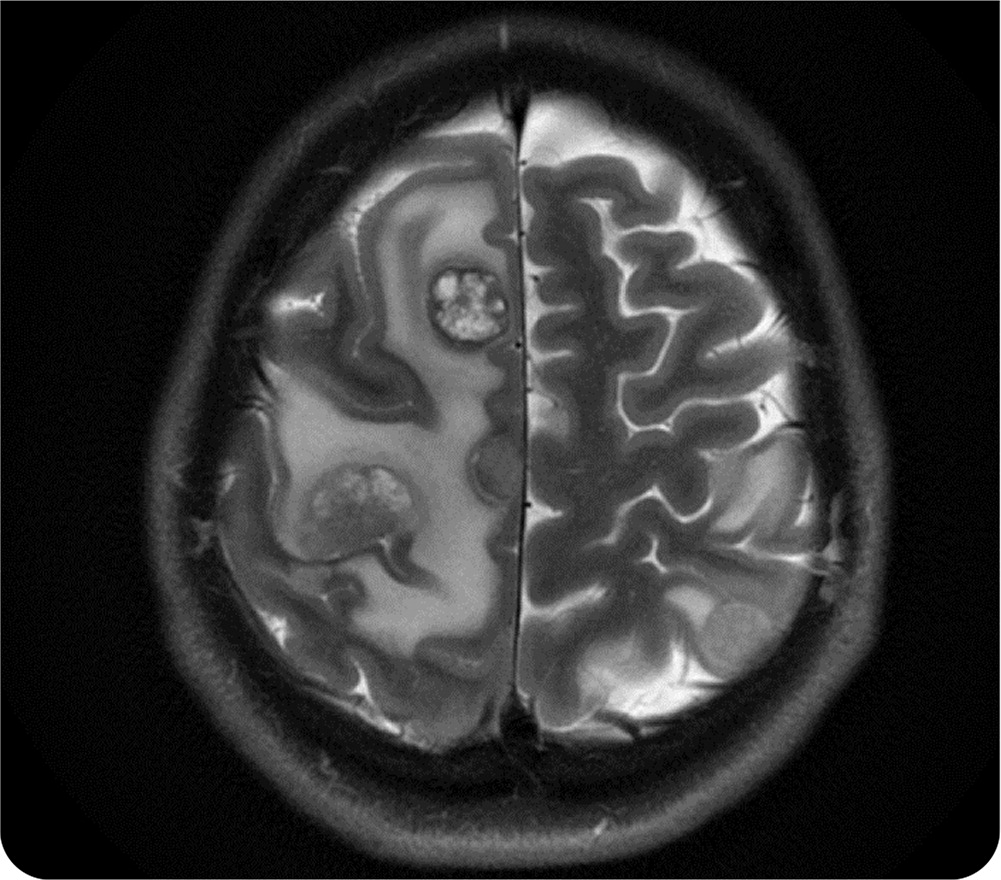
Physical examination confirmed left upper extremity weakness and impaired fine motor skills of the fingers. The patient had normal heart sounds. The remainder of the neurologic examination was unremarkable. Magnetic resonance imaging (MRI) of the brain was performed (Figure 1). A pedunculated lesion measuring 4.0 × 3.5 × 1.5 cm (Figure 2) was found on his left upper back.

Question
Based on the patient's history and physical examination findings, which one of the following is the most likely diagnosis?
A. Brain abscess.
B. Glioma with high-grade features.
C. Hemangioma.
D. Nodular melanoma.
Discussion
The answer is D: nodular melanoma, leading to brain metastasis. Nodular melanoma is the second most common type of melanoma, and it is the most aggressive form. The lesion can be pedunculated, polypoid, or an elevated plaque with ulcerations that may bleed intermittently. The primary lesion is commonly located on the trunk or limbs.1
Melanoma is the most lethal cutaneous malignancy; the five-year survival rate is 30% for patients with stage IV disease. However, early detection is associated with a 99.4% survival rate for patients with stages I and II disease.2 Risk factors for melanoma are sun exposure, indoor tanning, immunosuppression, personal history of nevi, family history of melanoma, and obesity.3
Any suspicious lesions should be completely excised, and a 1- to 3-mm border of healthy skin should also be excised around each lesion. Subsequent wide excision surgical treatment is based on biopsy results and disease staging. Treatment options for melanoma with large or symptomatic brain metastasis are limited to stereotactic radiosurgery, surgical resection with postoperative radiation therapy, or whole-brain radiation therapy. Approximately 50% of melanomas are associated with BRAF mutation (V600 mutation is the most common).4 Immunotherapy using ipilimumab (Yervoy) with nivolumab (Opdivo) may be effective for advanced disease in patients with the BRAF V600 mutation.
Brain abscesses can present with unilateral or progressive diffuse headache (69% of patients), fever (53%), focal neurologic deficits (48%), and seizures (25% have seizure as the first manifestation). The classic triad of headache, fever, and focal neurologic deficit occurs in less than 20% of patients.5 MRI is preferred for diagnosis and typically demonstrates a ring-enhancing lesion with central necrosis and vasogenic edema.
Gliomas with high-grade features typically develop over days to weeks, often with headache, seizures, and focal neurologic symptoms. MRI demonstrates an isolated ring-enhancing lesion with necrosis.6 Multiple lesions in the brain are uncommon; they are more typical of metastatic disease than primary brain malignancy.
Hemangiomas are benign tumors most often affecting the head and neck that typically present at birth or within the first few weeks of life. They are characterized as a well-defined papule, nodule, or plaque arising from a single focus; however, 20% of patients have multiple lesions. They are typically bright red to purple. They are most common in infants who are female, White race, or premature. Hemangiomas rarely progress after the infant reaches three months of age; most regress spontaneously.7 Known complications are ulceration, bleeding, scarring, infection, and functional impairment specific to location (e.g., periorbital [astigmatism, vision loss], airway [stridor/hoarseness]). Hemangiomas are commonly managed by observation. More complicated lesions can be treated with topical beta-blocker therapy or oral propranolol.8
| Condition | Characteristics |
|---|---|
| Brain abscess | Unilateral or progressive diffuse headache, fever, focal neurologic deficits, and seizures (in 25% of patients as the first manifestation) |
| Glioma with high-grade features | Develops over days to weeks with headache (dull and constant), seizures (50% to 80% of patients), and focal neurologic symptoms; MRI typically demonstrates an isolated ring-enhancing lesion |
| Hemangioma | Well-defined papule, nodule, or plaque arising from a single focus; however, 20% of patients have multiple lesions; the most characteristic color is bright red to purple |
| Nodular melanoma | Second most common type of melanoma; most aggressive form of melanoma; appears as a dark, pedunculated, or polypoid nodule |
The views expressed herein are those of the author and do not necessarily reflect the official policy of the U.S. Department of the Army, U.S. Department of Defense, or U.S. government.
