Am Fam Physician. 2024;109(4):298-300
Author disclosures: Dr. Skolnik reports serving as a speaker, consultant, or advisory board member for Abbot, AstraZeneca, Bayer, Boehringer Ingelheim, Boehringer Ingelheim/Lilly, Genentech, GSK, Heartland, Idorsia, Lilly, Merck, Novartis, Novo Nordisk, Sanofi, Sanofi Pasteur, and Teva, and reports receiving research support from AstraZeneca, Bayer, GSK, Novo Nordisk, and Sanofi.
Dr. Mahler reports serving as a speaker, consultant, or advisory board member for AstraZeneca, Boehringer Ingelheim, GSK, Theravance Biopharma, Verona Pharma, and Viatris, and receives royalties from Johns Hopkins University Press.
Dr. Yawn reports serving as a speaker, consultant, or advisory board member for AstraZeneca, Boehringer Ingelheim, GSK, Sunovion, and Teva.
To the Editor:
The article by Zeller and colleagues discusses how to distinguish asthma from chronic obstructive pulmonary disease (COPD).1 This distinction is important because the treatments for the two diseases differ. The authors state, “Asthma is diagnosed if airway obstruction on spirometry is reversible (greater than 12% and greater than 200 mL improvement in FEV1 [forced expiratory volume in 1 second]) with administration of bronchodilators.… COPD is diagnosed if airway obstruction … on spirometry is not reversible with bronchodilators.”
However, studies have shown reversibility in a significant proportion of patients with COPD. In the UPLIFT trial of patients with COPD, 54% of patients had bronchodilator reversibility based on the American Thoracic Society criteria of FEV1 improvement of 12% or greater and 200 mL or greater, and 73% of patients had reversibility when using the sole criteria of 12% or greater improvement in FEV1.2 A comprehensive review of COPD reversibility in multiple studies concluded that “… many patients with COPD do indeed exhibit bronchodilator reversibility and that reversibility testing is not a reliable measure to differentiate between asthma and COPD.”3
The European Respiratory Society/American Thoracic Society definition of reversibility was recently revised to greater than 10% of the predicted value in FEV1 or forced vital capacity.4 Using this updated definition would lead to a greater proportion of people with COPD being classified as having bronchodilator reversibility compared with the previous American Thoracic Society criteria of 12% or greater.
The 2023 GOLD report states, “… assessing the degree of reversibility of airflow obstruction … to inform therapeutic decisions is no longer recommended … and has not been shown to differentiate the diagnosis [of COPD] from asthma, or to predict the response to long-term treatment with bronchodilators or corticosteroids.”5
In Reply:
We appreciate the opportunity to respond to this letter. Our article does not address therapy for asthma and COPD, but rather the diagnosis of the two disease entities and distinguishing between them.
We agree that the critical difference between COPD and asthma is that COPD is characterized by airflow limitation that is not fully reversible with bronchodilators. In contrast, asthma is characterized by airflow limitation that is variable and reversible to near normal with bronchodilators.
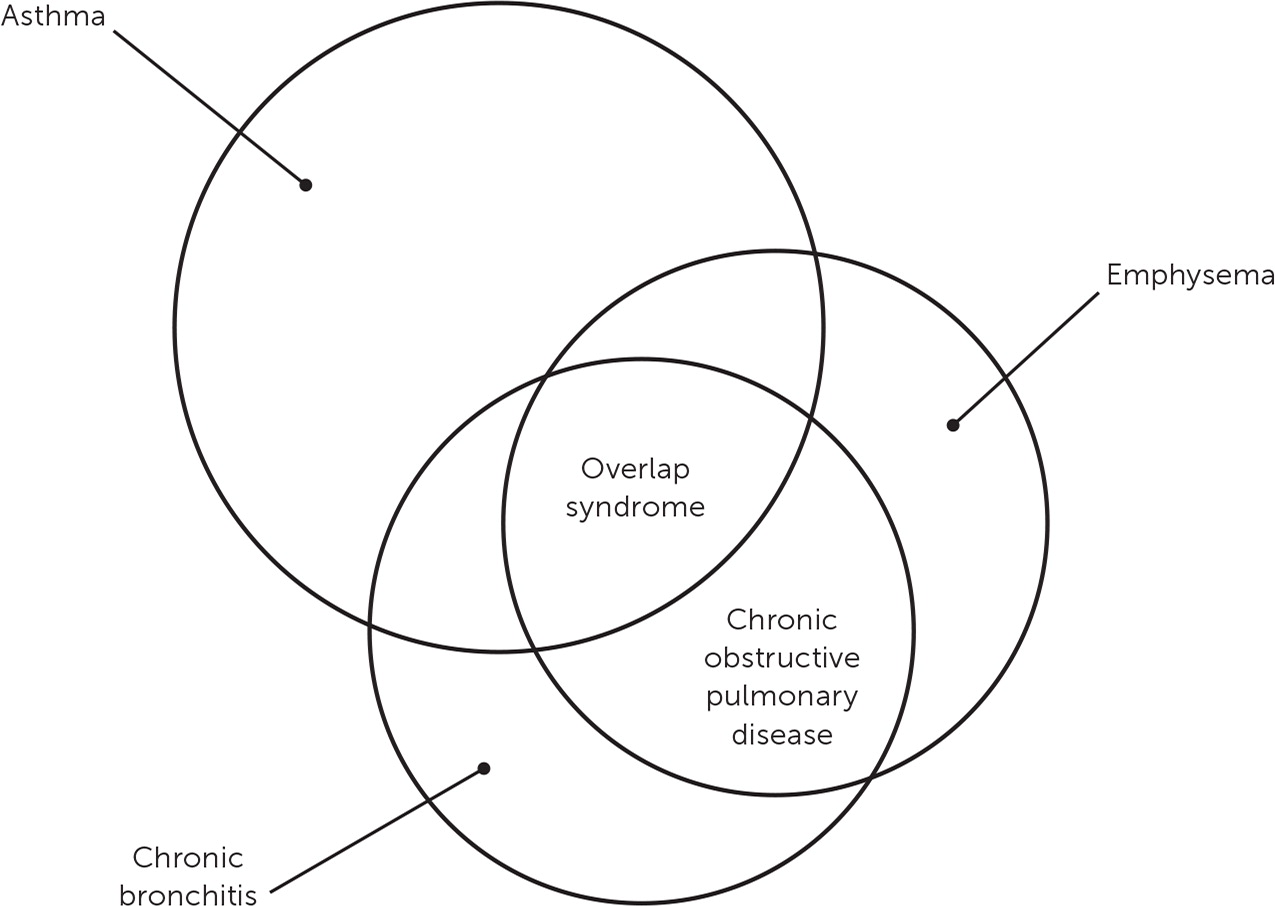
As briefly discussed in our article, robust literature has developed around the clinical reality of coexisting asthma and COPD.1–4 The natural history of asthma is to progress to fixed obstruction over time.5 Some have labeled the coexistence of the two disease entities “asthma-COPD overlap syndrome,” and for a time, it appeared that this might become a separate diagnosis. However, it is now standard clinical practice to diagnose both asthma and COPD if the patient meets spirometry criteria for both conditions. Distinguishing between asthma and COPD is not strictly an either/or, but sometimes a both/and situation. A Venn diagram has been useful as a visual aid (Figure 1).6 We hope this response helps readers in their clinical practice, and we encourage physicians to follow widely available guidelines for treating asthma and COPD.