
Am Fam Physician. 2025;111(4):296-297
Author disclosure: No relevant financial relationships.
To the Editor:
A 26-year-old previously healthy woman presented to a community hospital in Oregon with acute-onset, left-sided weakness and headache. She had returned from Morocco 1 week earlier and experienced symptoms of an upper respiratory infection 2 weeks prior to arrival. Physical examination found left-sided upper and lower extremity weakness and numbness. Magnetic resonance imaging of the brain showed numerous enhancing nodules with leptomeningeal enhancement (Figure 1). Infectious Disease and Neurology departments were consulted. A lumbar puncture was performed, a cerebrospinal fluid culture found no organisms, and cytology and infectious serologies were negative. Erythrocyte sedimentation rate and C-reactive protein levels were mildly elevated. Serum angiotensin-converting enzyme level was normal. Echocardiogram was negative for vegetations. Interferon-gamma release assay was positive. Chest radiography was normal. Magnetic resonance imaging of the spine was negative for epidural abscess but showed an incidental pleural rim-enhancing fluid collection measuring 2.6 cm × 1.2 cm. Computed tomography of the abdomen found focal pleural thickening. Radiology performed a biopsy and a pleural fluid sample was obtained and sent to an outside laboratory for broad-spectrum polymerase chain reaction testing.
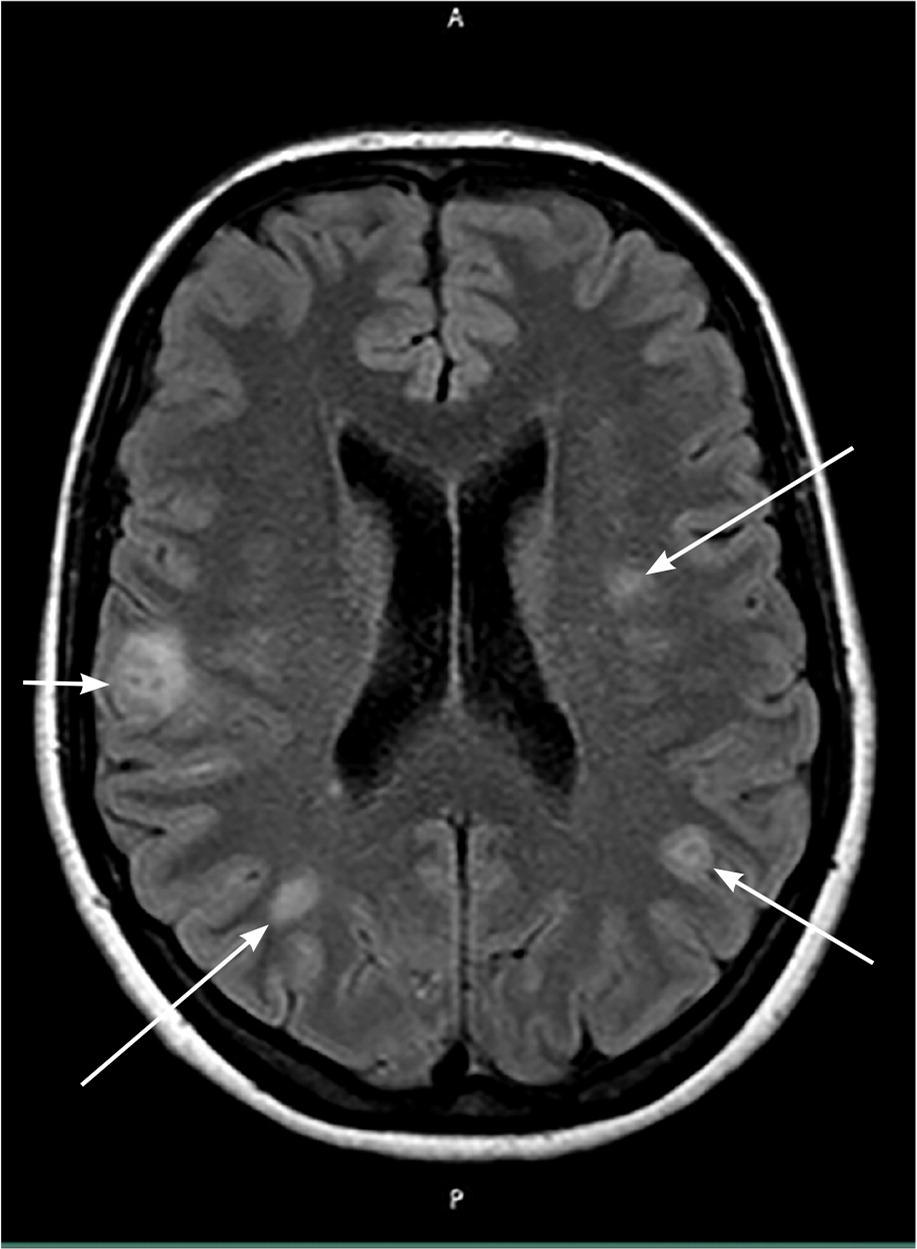
The patient’s weakness continued to worsen. Repeated magnetic resonance imaging of the brain found increased leptomeningeal enhancement and increased size and number of enhancing lesions. She was treated with prednisone for cerebral edema and empiric RIPE (rifampin, isoniazid, pyrazinamide, ethambutol) therapy and levofloxacin for presumed tuberculosis. The patient experienced clinical improvement, so brain biopsy was deferred, and she was discharged. Six weeks later, polymerase chain reaction test results returned positive for mycobacterium tuberculosis complex. At a follow-up visit, she reported feeling well and had regained her baseline strength.
Central nervous system tuberculosis occurs in 1% to 5% of tuberculosis cases.1 Tuberculomas are the least common presentation of central nervous system tuberculosis, found in 1% of cases.2 Tuberculomas are ring-enhancing brain lesions surrounded by edema.1 Multiple tuberculomas are seen mostly in endemic areas.2 Central nervous system tuberculosis has a mortality rate of 10% to 20% and can lead to neurologic disability in 5% to 24% of cases.3 Findings can resemble other conditions, such as sarcoidosis or malignancy.4 Cerebrospinal fluid can have normal or nonspecific findings.5 If clinical suspicion is high, RIPE therapy should not be delayed. As in our case, timely treatment is critical to ensure a return to baseline neurologic function.
