
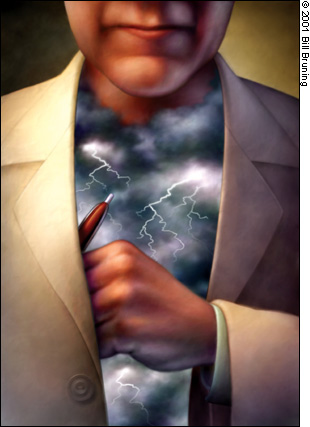
Malpractice accusations can be emotionally devastating. Here's how to withstand the pressure.
Fam Pract Manag. 2001;8(5):41-44
Chances are better than 50/50 that you'll be sued for malpractice at least once during your career.1 So, what's the good news? Most lawsuits don't go to trial and those few that do usually find in favor of the physicians. However, that's little consolation to a physician dealing with the stress of malpractice litigation. If you're ever in the unfortunate situation of being the target of a malpractice lawsuit, having some familiarity with the litigation process and the emotions that accompany it will help you maintain your equilibrium.
The summons
Often the first clue you have that you're being sued is when you receive a summons. Many physicians describe their initial reaction as one of shock, disbelief or denial. Intense distress follows, including feelings of depression, anger and physical illness, and usually lasts about two weeks. It's called the “period of disequilibrium.”2 It's during this time that lawyers and the malpractice insurance company begin to get involved, requiring you to hand over at least partial control of the situation to them. Relinquishing control is generally difficult for physicians who are used to taking charge and being the decision makers.
What you may feel. Shock, denial, shame, loss of control, anxiety, anger, depression or physical symptoms.
What you should do. An important first step in coping with malpractice litigation is to understand that it happens, regardless of whether negligence actually occurred, and that being sued is truly a traumatic experience. Placing your professional reputation in someone else's hands can make you extremely anxious. To retain some sense of control, learn as much as possible about the litigation process. Ask your lawyer or a representative from your malpractice insurance carrier to explain the steps of the litigation in detail. To reduce stress, stay actively involved in your case by working closely with your lawyer.
KEY POINTS
Regardless of whether negligence actually occurred, it is normal for physicians to feel depressed, angry, ashamed and isolated – even two years following a lawsuit.
Excessive self-blame can be detrimental not only to your morale but also to your ability to take whatever corrective action is necessary.
One way to prevent future lawsuits is simply to improve your communication skills with your patients.
The discovery
After you receive the summons, the discovery period begins. Interrogatories will probably be served, which will ask you to respond in writing (and under oath) to questions from the plaintiff's attorney. A deposition usually follows. Again under oath, you'll be asked to respond verbally to the plaintiff's attorney's questions. It's difficult to predict how long the discovery period will last. If information clearly in your favor is disclosed, the plaintiff may decide to drop the case immediately. Or, the discovery period could last months or even years, after which your case could be dropped or settled or proceed to full trial. Legal proceedings are commonly subject to postponements and last-minute changes.
To minimize your frustration, anticipate that there will be frequent disruptions to your schedule during this time. You may feel you're on an emotional roller coaster as your feelings intensify every time you are called upon to deal with some aspect of the case; these feelings are normal.
During litigation, the traits that serve us well as physicians can also make us susceptible to an exaggerated sense of responsibility and feelings of guilt and self-doubt.3 Under stress, we are more likely to accept guilt even when it's not warranted. If you aren't careful, these traits could make you a poor defendant in your own malpractice case. Instead, answer questions factually and accurately and take care not to assume unwarranted blame. This is important not only during the discovery period, but at all stages of litigation.
What you may feel. Depression, hurt, anger, isolation, guilt or shame.
What you should do. Although studies of physicians dispel the assumption that incompetent doctors get sued and competent ones do not,4,5 being accused of falling below the standard of care can be devastating. To cope with this accusation, you may find yourself pushing harder and working longer hours. Instead of burying yourself in your work, continue to pursue personal interests or hobbies, and strive to keep your professional and personal lives balanced. Social support is also extremely important to you now.
Even if your attorney has rightly advised you not to discuss the legal or clinical aspects of the case with anyone, it is perfectly acceptable and, in fact, beneficial to talk with someone about your feelings about being sued. Although you may find it awkward at first, talking with your spouse, a trusted friend, a colleague or a trained professional helps counteract the shame and isolation you may feel. With the prevalence of malpractice litigation these days, it's very likely that you already know of a colleague who has been sued. Someone who has actually been through the litigation process can be a powerful source of support during this time.
Another source of support may be your malpractice insurance carrier. Some carriers offer support services to the physicians they insure. These vary depending on the company, but may include one-on-one sessions with a consultant, telephone consultations with a trained professional or with a physician who's also been sued, or support groups for physician defendants. State medical societies may also offer similar services. [The box lists some additional resources.]
RESOURCES
If you are being sued for malpractice and need help handling the stress, contact your state medical association, specialty medical society or your malpractice insurance carrier. These organizations may offer support services or may be able to direct you to support groups or trained professionals in your area. Some additional resources are listed below.
Support
Center for Personal and Professional Well-Being
21 W. Colony Place, Suite 150
Durham, NC 27705
Phone: 919–489–9167
Fax: 919–419–0011
Web site: www.cpwb.org
The Center for Professional Well-Being offers workshops and seminars, as well as individual assessments and telephone consultations.
Suggested reading
The Health Care Providers Guide to Facing the Malpractice Deposition. Uribe CG. CRC Press; 1999.
The Jurisprudent Physician: A Physician's Guide to Legal Process and Malpractice Litigation. Dean M. Legis Press; 1999.
The trial and the settlement
As the discovery period progresses, you may find yourself in agonizing discussions with your lawyer and malpractice insurer about whether to settle out of court or proceed to trial. Although it's your life and your future being discussed, your opinion is likely to be just one of several factors that determine how your case will proceed. You may feel that agreeing to settle your case won't sufficiently clear your professional name, especially if the settlement is listed in the National Practitioner Data Bank. However, settling your case out of court is not necessarily an indication that you were at fault. Whether a settlement is reached depends on various factors, including how well your case could be defended in terms of the quality of the medical records, the credibility of the witnesses or the physician-defendant and possible juror sympathy toward the plaintiff.
Approximately 6 percent of all lawsuits eventually proceed to trial. If your case goes to trial, you may find that being in the public eye intensifies the shame you feel about being sued. You may also feel betrayed as you face the plaintiff and his or her family in court for the first time. And, of course, there's the tremendous uncertainty and suspense that a trial brings. Your future rests in the hands of a jury whose knowledge of your abilities is limited to the medical record and the information introduced by the lawyers. Although juries tend to find for the physician-defendant, even a favorable verdict may not help you feel vindicated for the pain and stress you endured during the lawsuit. As a result, some physicians continue to be angry long after their ordeal is over.
Whether a case is dropped, settled or tried, the issue of medical mistakes merits attention. If you did indeed make a clinical error, you certainly need to explore why the mistake was made and how it can be prevented in the future. At the same time, however, we must face the reality that, as physicians, we are human and do sometimes make mistakes. This can be difficult, especially when our society and, indeed, our own profession hold us to such high standards, often without providing the necessary systems to ensure those standards can be met. In fact, physicians have admitted to experiencing feelings of panic, guilt, embarrassment, humiliation, inadequacy and isolation after making mistakes, even when these mistakes do not result in a lawsuit.6 These feelings, if not addressed, may interfere with your ability to deal with the mistake constructively.
What you may feel. Frustration, shame, betrayal, anger or a desire to make something good out of the experience.
What you should do. Continue to use the same coping strategies during the trial as you used leading up to it. If a medical mistake led to the lawsuit, it may be helpful for you to recognize that you aren't the only physician to have ever made a mistake; they happen regularly.7 Again, talking to a trusted individual can help you deal with your feelings. Self-evaluation and even an appropriate amount of guilt can be motivators for change, but excessive self-blame can be detrimental, not only to your morale but also to your ability to take corrective action. Analyzing why you made the mistake, dealing with the mistake responsibly and taking remedial steps to help prevent future malpractice litigation can help you feel you're making something good out of the experience.
The aftermath
A malpractice lawsuit can leave you with distressing memories, negative expectations about the future and a tendency to practice defensive medicine. Don't be surprised if you run into reminders of the experience long after it's over (for example, every time you're asked to report your malpractice history on applications for license renewals, credentialing or hospital privileges). As long as two years after their lawsuits, physicians have reported experiencing more job strain, more shame and more doubt than they did prior to their lawsuits, although these feelings are less intense than during the lawsuit itself.8 On the other hand, physicians who have been sued have also reported more active coping both during the lawsuit and two years later.
What you may feel. Continued stress, self-doubt, job strain, an increased ability to cope or a desire to make something good out of the experience.
What you should do. Taking an active role in malpractice prevention is a constructive way to deal with being sued and the aftermath of a lawsuit. One way to reduce your risk of being sued again is to improve your communication skills. One study showed that family physicians and internists who have never been sued tend to use more statements of orientation (such as patient education), more facilitation (such as checking that patients understand your instructions and encouraging them to talk) and also more humor than those who have been sued.9 Many continuing medical education courses specifically address improving patient-physician communication. Additionally, some malpractice insurance carriers offer courses on litigation. This may help you identify deficiencies in your practice such as chart documentation or administrative problems.
If, at any time, you feel overwhelmed by the stress of your experience, you may want to seek the help of a mental health professional. A continued attention to maintaining life balance and social support is crucial. It can help you stay on the path of active, healthy coping and enable you to go on with your personal and professional lives.