
Fam Pract Manag. 2002;9(4):20-23
Docs expected to refuse new Medicare patients due to payment cuts
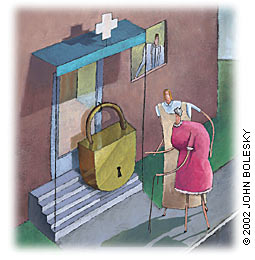
“For the first time, significant numbers of doctors are refusing to take new Medicare patients, saying the government now pays them too little to cover the costs of caring for the elderly,” reports the March 17 New York Times. Earlier this year, Medicare cut the conversion factor used to calculate payments to doctors by 5.4 percent for 2002. The cut only adds to the frustration doctors have expressed for years with low Medicare reimbursement. Many fear the drop in Medicare payments will also lead to payment decreases from private insurers who often set their reimbursement rates according to what Medicare pays.
The AAFP has reported that 17 percent of family physicians are not taking new Medicare fee-for-service patients. The payment cuts are expected to increase those numbers, making it more difficult for Medicare beneficiaries to find physicians.
Proposals are being considered in Congress to increase Medicare payments to physicians, but Congress has not yet taken action.
According to the AAFP’s Government Relations office, this year’s decrease marks the largest ever cut in Medicare physician payments and the fourth time in 11 years that rates have been reduced. Over that same 11-year period, Medicare payments have risen an average of just 1.1 percent a year, less than the average rate of inflation. (For more information, seewww.aafp.org/fedgov/x2400.xml.)
While the 5.4 percent cut in the Medicare conversion factor will reduce physician payments overall, five E/M codes will see slight increases in 2002, according to the Nov. 19 Part B News: 99211 (1.9 percent increase), 99212 (.67 percent increase), 99214 (.13 percent increase), 99203 (.56 percent increase) and 99321(.36 percent increase).
PRACTICE PEARLS from here and there
More meaningful medicine
As the practice of medicine becomes more pressured and complex, physicians are looking for ways to prevent burnout or to rediscover their calling. One simple suggestion is to buy a journal and review your day each evening, recording brief answers to the following three questions: “What surprised me today?”, “What touched me today?” and “What inspired me today?” As you review your day, try to look at the events through the eyes of a writer, not a doctor. In other words, look for the stories. It may be difficult to do at first, but in time you’ll become more attuned to recognizing these moments as they happen and capturing them in your journal.
– Remen RN. Crisis of meaning. Fam Pract News. Jan. 15, 2002:10.
Medicare payment error rate lowest to date
The percentage of improper Medicare payments in fiscal year 2001 was an estimated 6.3 percent ($12.1 billion) of all fee-for-service Medicare payments – less than half of the 13.8 percent ($23.2 billion) reported when the government started conducting overpayment audits in 1996, according to the Department of Health and Human Services’ Office of Inspector General. Improper payments occur when a claim involves coding errors, documentation errors, medically unnecessary services or “noncovered/other” services.
Burned out already?
Is it possible to burn out in your career before you’ve really begun? Yes, according to a study in the March 2002 Annals of Internal Medicine, which found that 76 percent of residents met the criteria for burnout. Fifty-three percent said burnout resulted in suboptimal care at least monthly, while 32 percent said it resulted in suboptimal care weekly.
Insuring your own
Health care workers are leading the pack when it comes to workers losing their health insurance coverage. Between 1988 and 1998 the number of uninsured health care workers increased 83.4 percent to total 1.36 million. The households of uninsured health care workers account for 10 percent of all uninsured children in the United States, according to a study published in the March 2002 American Journal of Public Health.
Patients urged to speak up
The Joint Commission on Accreditation of Healthcare Organizations, with support from the Centers for Medicare & Medicaid Services, has launched a national campaign to prevent medical errors by encouraging patients to become more active in their care. Based on research which shows that patients who take part in decisions about their health care are more likely to have better outcomes, the program advises patients to speak up if they have questions or concerns and to pay attention to the medications and medical services they are receiving. Individuals can download a “Speak Up” patient education brochure atwww.jcaho.org/trkgen_frm.html.
No harm in full disclosure
Disclosing financial incentives that managed care organizations offer to doctors to control health care costs does not harm patients’ trust in their physicians, according to a study published in the March/April 2002 Health Affairs. The study found that after patients whose HMOs used capitation were informed of financial incentives, their trust in their doctors increased 1.4 percent.
A force to reckon with
The number of drug representatives has nearly doubled over the last five years to 80,000, reports the March 14 Wall Street Journal. Drug companies now spend about $7.2 billion on their sales forces per year, or more than 2.5 times what they spend on direct-to-consumer advertisements. Meanwhile, between 1996 and 2001, the number of drug advertisements submitted to the FDA for approval increased nearly 35 percent to more than 34,000 annually. But the FDA says it is finding fewer drug company ads or marketing materials to be false, misleading or otherwise out of compliance.

"Doctor will have your paperwork ready just as soon as he finishes figuring out the codes."