
Just when you thought declining reimbursement and rising expenses had squeezed your practice dry, liability insurance premiums began to climb dramatically. Here’s what’s behind the increases.
Fam Pract Manag. 2002;9(9):47-51
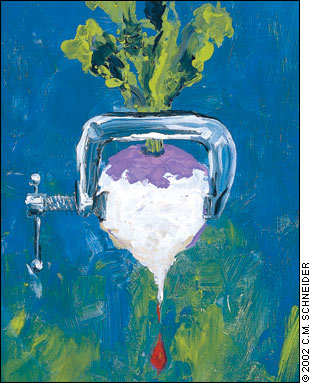
In certain areas of the country, skyrocketing medical liability insurance premiums are pushing physicians out of practice and denying patients access increased an average of 30 percent or more last year. Another 12 states saw average premiums increase 25 percent during the same period, and problems are emerging in several other states as well. (See the map.) The hot spots are states where insurers have either left the market or gone bankrupt, where awards are particularly high or where there is very active litigation in certain areas (e.g., pregnancy-related cases). Premium increases as high as 80 percent have been reported in some areas.1
The premium differences between these areas and those in other parts of the country are dramatic. In Wisconsin, a family doctor who delivers babies and performs cesarean sections pays about $14,000 a year for coverage that extends to infinity. Family physicians with far less coverage pay three to five times as much in some other states. Physicians in other specialties are suffering, too. In southern Florida, obstetricians spend $209,000 for $250,000 in coverage and, in effect, are essentially self-insured.
Dimensions of the problem
The most important factor in rising medical liability premiums appears to be the size of the awards, rather than the frequency of lawsuits. In Wisconsin, the number of claims filed actually decreased from 348 in 1990 to 249 in 2001.2 In 1995, the national median for jury awards was $500,000 and the median pretrial settlement amount was about $350,000. By 2000, the median jury award had risen to $1 million, with the median pretrial settlement award at $500,000. In 2000, defendant doctors prevailed in 60 percent of all the cases that went to a jury.3
The size of the awards is driven primarily by the medical care costs of the successful plaintiff. Pain and suffering, along with other noneconomic damages, can be factors in the increase in awards, but the rising cost of medical care appears to be the most significant factor.
Other important data describing the medical liability insurance crisis come from the Physician Insurers Association of America (PIAA), which represents 51 companies, many of which are doctor owned or doctor directed. In 2001, the companies’ loss ratio, the amount of money they paid out for malpractice claims compared to the amount they took in, was about 116 percent. In other words, for every dollar that they received in premiums, they paid out $1.16.4 Malpractice insurers can be profitable with a loss ratio as high as 105 percent because the difference between the amount received in premiums and the amount paid out in losses may be more than made up for by investment income earned on the premiums that are held in reserves for future pay-outs.
What happened? A robust economy in the 1990s meant more visits to doctors and excess capital. More patients going to their doctors meant a greater chance for more lawsuits in the future with higher liability costs. Excess capital meant that there was more money to invest, and the companies invested their funds in the industry they knew best – their own – by discounting their premiums below actuarial risk in order to obtain or preserve market share. The increased suits, and awards, that began to roll in toward the end of the 1990s coincided with a drop in the investment economy. Suddenly, malpractice carriers faced the “perfect storm” in 2001: Higher loss ratios (116 percent) occurred at the very time investment income plummeted (−8 percent yield), resulting in significant losses. Consequently, major carriers decided to leave the market. Among them was the second largest carrier, The St. Paul Companies, which reported nearly $1 billion in losses for medical liability in 2001.
KEY POINTS
Medical liability insurance premiums have increased significantly for some physicians during the last two years.
The trend is the result of increasingly large plaintiffs’ awards and higher loss ratios for insurers.
Public education, improved legal defense and tort reform are among the solutions.
Costs of medical liability
Several factors are crucial in understanding the true costs of medical liability: insurance premiums, defensive medicine, physician time and medical care costs.
Insurance premiums. The dramatic premium increases experienced recently by many physicians have much to do with stable or even decreasing premiums paid during the mid-to-late 1990s. At that time, insurers were looking for ways to avoid paying taxes on their reserves, which were growing rapidly as a result of significant gains in their investment portfolios. Rather than maintain excess capital on the books and pay taxes on that capital’s investment income, the companies bought or preserved market share by selling policies for less than their actuarially predicted risk. The market was “soft.” In other words, they sold $10,000 of risk for $5,000 in premiums to sell twice as many policies. At the time, doctors were pleased with stable or declining premiums; insurance company shareholders were happy with their rising share prices and dividends. Eventually, when the under-reserved losses finally came due and the investment economy cooled, a correction was bound to occur. That day has arrived, and the medical liability insurance market has “hardened” dramatically in the past two years.
Defensive medicine. Doing additional tests or procedures more for liability protection than patient benefit costs an estimated $40 billion to $100 billion a year.
Physician time in litigation. Physicians who are sued for malpractice spend on average about one week of their professional life dealing with the claim.
Medical care costs. Rising liability insurance premiums are part of the reason for increasing medical care costs, as doctors attempt to pass on the additional costs of liability coverage in the form of higher patient fees. Similarly, rising medical care costs affect liability premiums as insurance companies have to pay out more for the medical care of successful plaintiffs.
Even more distressing are the indirect costs of the medical liability system, represented by changes in physician practices and relationships with their patients.
Practice changes. Without question, being sued for malpractice represents a very profound experience for physicians. According to one study of about 150 doctors who were sued for malpractice, 95 percent reported significant physical or emotional symptoms during the litigation process, 42 percent stopped seeing certain kinds of patients and 28 percent stopped doing certain kinds of procedures.5
Extensive media coverage of trauma centers closing in Nevada and women driving long distances to find maternity care in Mississippi spotlight the impact that the liability insurance crisis has had on access to medical care. Public and legislative interest in tort reform appears to increase when medical care access is restricted.
Changed relationships. Being sued can permanently change how doctors regard themselves and their patients. Some may contend that the risk of malpractice litigation is simply an inevitable cost of doing business for physicians. That point of view fails to recognize that doctoring is by its very nature an intensely personal endeavor, not one that can be treated as an arms-length commercial transaction.
Perspectives on malpractice
Doctors often assert that if there were fewer lawyers, there would be fewer medical malpractice lawsuits. While the U.S. has one-sixth of the world’s lawyers, studies have shown that it is the number of doctors, not lawyers, in an area that predicts the number of malpractice lawsuits.6 The explanation for this finding lies in the fact that more doctors in an area means more doctor-patient encounters. More encounters means a greater chance for more unwanted or unexpected outcomes, with more lawsuits as the result.
Plaintiffs’ lawyers commonly attribute the problem to “just a few bad doctors” and point to studies such as one in Southern California that reported that 0.6 percent of Los Angeles County’s doctors resulted in 10 percent of the lawsuits and 30 percent of the pay-outs in one year.7 The problem with this study and others like it is that they look at limited periods of time during which only a small number of doctors are likely to be named in suits, while virtually every doctor is likely to be named in at least one suit over the course of a career.
Insurance companies contend that the current crisis is about matching premiums to liability: Insurance policies were sold in the 1990s for less than their projected risk and now the piper has to be paid.
The public ends up confused in the media battle for their support. Consider the combatants: the poor underpaid doctors, the lowly downtrodden lawyers and the small struggling insurance industry. All look like villains to members of the public. At this time, however, the public appears to have heard the message about premiums rising too high and creating havoc in the availability and practice of medicine. If recent surveys are to be believed, the public is sympathetic on this point.
A poll conducted in April for the Health Care Liability Alliance by Wirthlin Worldwide showed that 73 percent of respondents favor reasonable caps on the “pain and suffering” component of malpractice awards, and 76 percent favor limiting attorney contingency fees. Some 78 percent of respondents were concerned that increases in medical liability costs could limit their access to care, and 71 percent felt that malpractice litigation is one of the main reasons that health care costs are rising. Almost half (48 percent) thought there are too many lawsuits filed against doctors, although about 17 percent thought there are too few.8
One reason for these different perspectives is that people are not in agreement on the goals of the tort system and whether it accomplishes those objectives. Most would argue that the tort system is supposed to accomplish three goals: make the injured party whole again, punish the individual who committed the harm and put others on notice that they should avoid the behavior that caused the injury. In fact, the system does not do any of these very well.
As to making the patient whole, the Harvard study in New York State showed that fewer than two percent of patients injured as a result of negligence sued for malpractice. And the researchers estimate that “perhaps half the claimants will eventually receive compensation.”9 Several other large, important studies have found similar results. These studies suggest that there is more malpractice being committed than is being recognized, litigated or compensated. The system is not very efficient at making patients whole when fewer than 1 percent of those with injuries due to medical error ever get any money.
When it comes to punishing the individual who committed the harm, the tort system certainly exacts an emotional punishment on individual doctors, but insurance softens the financial blow.
The system also falls short at putting others on notice. Doctors rarely know the most likely reasons for being sued. Therefore, they do not know what they should be doing or not doing to avoid a particular harm.
Potential solutions
There are only two ways to go through a medical career and never be named in a suit. The first is to never see a patient. The second is to keep all patients deliriously happy, because happy patients do not sue. Of course neither approach is very realistic. Another “solution” doctors may contemplate is practicing without liability coverage. As tempting as this strategy may be, many states mandate coverage by making it a prerequisite to maintaining a medical license. The following are more practical strategies for improving the current malpractice climate:
COMING SOON
Look for Dr. Roberts’ article on malpractice risk reduction strategies in an upcoming issue of FPM.
Public education
One of the great dilemmas of American health care is that even as doctors are able to do more and better, patients expect more and better. It seems difficult, if not impossible, to meet public expectations. The media contribute to this problem by sensationalizing medical advances. Physicians and the media share a responsibility to provide realistic portrayals of medical care so people have more reasonable expectations of what physicians can do.
Improved legal defense
Emerging science has made some types of malpractice cases easier to successfully defend. For example, studies show that the cause of neonatal seizures, mental retardation or cerebral palsy in more than 90 percent of affected children is unknown, but it is not due to the birth process.
Tort reform
Adopted in the 1970s in California, the Medical Injury Compensation Reform Act (MICRA) has served as a model for many tort reform efforts. Experience with MICRA-type reforms has shown that a cap on noneconomic damages (pain and suffering, loss of consortium, etc.) is the single most effective way to moderate premiums – it lowers premiums by about 15 to 18 percent.
Reducing the statute of limitations to three years for an adult also reduces premiums by about 8 to 9 percent. Restraining attorneys’ contingency fees to a sliding scale that limits them to no more than a third of the overall award will bring premiums down by about 5 to 7 percent.6 Two other reforms that can help to moderate premiums are the collateral source rule, which allows the jury to hear that there are other sources of money for the patient, and periodic payment, which allows for payments to be paid over time as they are needed (e.g., future medical costs), rather than in a single lump sum.
Alternative dispute-resolution systems such as binding arbitration or mediation, though appealing in some respects, are not necessarily more cost-effective than more traditional approaches. Loser pay systems are popular, especially in Europe, but are not generally favored by Americans.
The Help Efficient, Accessible, Low-Cost, Timely Healthcare (HEALTH) Act, introduced by Rep. James C. Greenwood, R-Pa., would apply MICRA reforms to all states through federal law. Political pundits give the HEALTH Act a low chance for passage at this time. Many believe that the better strategy is to push for MICRA reforms at the state level in those states with the biggest problems.
Conclusion
Lawsuits alleging medical negligence date back as early as the founding of the Republic. The direct and indirect costs of malpractice litigation are considerable. Liability insurance premiums fluctuate based on patterns of medical care utilization and on returns from the investment economy. The key actors in the liability system all have different perspectives on the reasons and solutions for the current crisis. While the initial temptation is to push for any and all types of tort reform, experience has shown that some reforms are more effective than others and that some may actually make matters worse.