
You have one minute to identify the first-line therapy for a pregnant patient with tuberculosis. How will you find the answer?
Fam Pract Manag. 2008;15(6):23-28
Author disclosure: Dr. Hubbard disclosed that he is a reviewer for DynaMed, a point-of-care clinical reference resource. He receives a free subscription to DynaMed in exchange for this work.
Every 15 minutes, on average, family physicians face the difficult challenge of practicing evidence-based medicine (EBM), educating the patient and staying on time. While some believe these three items are mutually exclusive, I happen to disagree. I have practiced EBM at the point of care since 1998. Although I am a faculty member of the University of Wisconsin Department of Family Medicine, I practice clinical medicine 99 percent of the time (with an occasional student or resident shadowing me) in the department's clinical group, which operates like many highly productive private practices. I practice with 20 other physicians and conduct 20 visits per day.
Over the years, I have observed that students and residents seem to grasp these EBM skills readily, whereas many clinicians seem to be too busy to learn new tricks. The point of this article is to share some of the tips and shortcuts that have helped me – and can help you – to practice EBM and deliver effective patient education at the point of care. Methods I will outline in this article require a minimum of work and time, and as you become more familiar with them, efficiency improves, resulting in quicker and more effective information searches. To demonstrate these methods, let's look at some scenarios physicians encounter every day:
Clinical scenario #1: Getting acquainted with EBM resources
Yesterday, you saw a 27-year-old at 39 weeks who had a urine dipstick of 1+ protein, so you ordered a panel of labs that included uric acid. The next day, while the patient's labs are in process, your EBM-savvy partner sees your order. He says he read an article in American Family Physician (AFP) that said uric acid is no longer a useful predictor of preeclampsia. You have one minute before you start seeing patients for the day. What might you do?
Here are your options:
A: Do nothing and trust him because he is probably right.
B: Look on the AFP Web site for the article.
C: Do a Google search for “uric acid preeclampsia predictive value.”
D: Do your own EBM search to verify the study your colleague mentioned.
Here are the results you can expect for each option:
A: You slide down the slippery slope of practicing on hearsay, not EBM.
B: After several minutes of searching the AFP site, you find some answers in a 2004 review article.
C: Your Google search returns hundreds of hits that include links to the American College of Obstetricians and Gynecologists Web site and The Green Journal, but these resources are too research oriented for you to apply quickly.
D: You quickly find the evidence-based answer in an EBM resource, such as DynaMed.
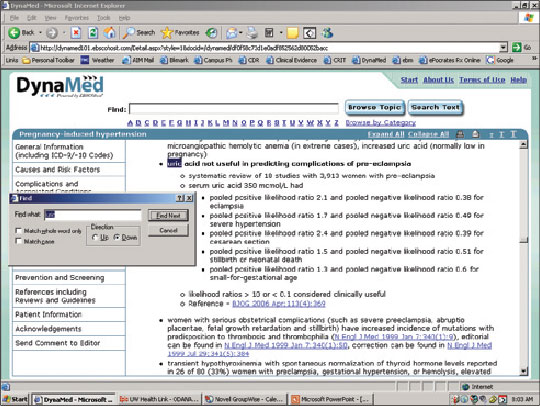
The screen shot below shows how I actually did this in one minute. First, go to the DynaMed Web site (http://www.dynamicmedical.com). You have to subscribe to this service, but once you do, you can quickly access it through your Internet browser. At the top of the DynaMed screen, click on the letter “P” (for “preeclampsia”); this is quicker than typing the whole word, which you might misspell. Then use the “Find” shortcut (Ctrl + F on a PC, or Cmd + F on a Mac) to search for “preecl” on the page (you don't need to type the entire word). In seconds, you will be linked to the pregnancy-induced hypertension section. Click on diagnosis to expand that section. Use the “Find” shortcut again to find “uric,” which will present you with the most recent EBM summary. It states that uric acid is not a useful predictor in preeclampsia.
DynaMed is just one of several online EBM resources you can subscribe to. Other useful resources include Essential Evidence Plus (formerly InfoRetriever; http://www.essentialevidenceplus.com), First Consult (http://www.firstconsult.com) and UpToDate (http://www.uptodate.com). (AAFP members can receive discounts on some of these programs; see https://www.aafp.org/online/en/home/membership/resources/memberdiscounts.html.) After signing up for one of these resources, spend some time exploring the site. After that, you'll be ready to start using the resource at the point of care, and with each subsequent use, you will become more efficient.
Clinical scenario #2: Using Google effectively
A patient comes to you from the public health office because of a positive tuberculosis (TB) skin test. The public health nurse told the patient to start TB treatment, but she is pregnant and wants to make sure it is safe to start therapy. How can you find out?
Here are your options:
A: Call the public health nurse and ask her what medications are safe.
B: Ask a colleague.
C: Prescribe isoniazid (or INH) because you think you heard in residency (10 years ago) that it is safe in pregnancy.
D: Verify the answer yourself, making the patient and you feel most comfortable.
Here are the results you can expect for each option:
A: You are on hold for five minutes before you get the nurse's voice mail and leave a message.
B: Your colleague doesn't know either.
C: You prescribe INH anyway and risk practicing out-of-date medicine.
D: You complete an Internet search within minutes in the exam room and prescribe the appropriate medication.
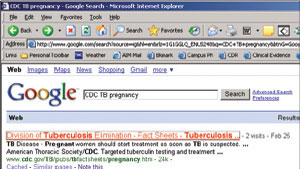
Choice D can be accomplished in several ways. Surfing a medication site such as http://www.epocrates.com will quickly tell you that INH is category C in pregnancy and should be used with caution, but it will not tell you the first-line choice of drug in this situation. Using the DynaMed method described earlier would reveal studies and treatment for TB in pregnancy. However, another option would be the Centers for Disease Control and Prevention (CDC) Web site, http://www.cdc.gov. To avoid the CDC's overwhelming home page and search engine, simply do a Google search for “CDC TB pregnancy” (without the quotes). The first hit is a CDC fact sheet on tuberculosis and pregnancy (see the screen shot below). Use the “Find” shortcut (Ctrl + F on a PC, or Cmd + F on a Mac) and enter “INH” or “treatment,” and you'll quickly find this statement: “Isoniazid (INH) administered either daily or twice weekly for 9 months is the preferred regimen for the treatment of LTBI in pregnant women. Women taking INH should also take pyridoxine (vitamin B6) supplementation.” You now have no doubt about the treatment plan.
Don't forget: If your Google search includes only medical terms (e.g., “tuberculosis”), Google displays the following links just above your list of hits: Treatment, Tests/diagnosis, For patients, From medical authorities, Symptoms, Causes/risk factors, For health professionals and Alternative medicine. This makes it easy to refine your search, if needed.
Clinical scenario #3: Creating easy access to favorite resources
At 4:30 p.m., a 69-year-old male with Alzheimer's presents as a new patient with his daughter. After 15 minutes of discussion, the daughter mentions he has had some dizziness for months, but the previous doctor didn't know the etiology. You now notice 1+ leg edema. On auscultation, you hear an irregular heart beat. His ECG shows atrial fibrillation. Since the patient is stable, you don't need to admit him, but you do need to do a lot of teaching and ordering of tests before the workday ends at 5 p.m. You're worried because it often takes days for a patient to understand the diagnosis and treatment plan when in the hospital. You realize you also have a dozen phone calls and refills to attend to with the nurse before she leaves.
Here are your options:
A: Admit the patient to the hospital. After all, he could sue the last doctor who missed this diagnosis, and you don't want to get in trouble.
B: Tell the patient that he has atrial fibrillation and needs some tests, and instruct his family to call back next week to schedule another appointment.
C: Talk to the patient and his daughter for another 20 minutes about the causes, symptoms and treatment.
D: Use the Internet to help teach the patient and his daughter about this new diagnosis.
Here are the results you can expect for each option:
A: Your actions result in poor use of resources and defensive medicine, which increase health care costs.
B: The family leaves confused and worried.
C: The patient and his daughter appreciate your time but promptly forget 80 percent of what you told them. Your nurse is now gone, doubling the amount of time you must spend on after-hours care.
D: Although you could direct the patient and his daughter to familydoctor.org or MD Consult, where they could read simple explanations about atrial fibrillation, in this case you set up the family with an interactive tutorial on Medline Plus (http://www.nlm.nih.gov/medlineplus/tutorials/atrialfibrillation/htm/index.htm), which you have saved to your iGoogle list for easy access from any location. (More about iGoogle in a moment.) As the patient watches the 15-minute tutorial, you ask your nurse to set up an echocardiogram, labs, an office appointment with cardiology, and a head CT (which later confirms multi-infarct dementia). You also fax in refills and call a few patients before re-entering the exam room for a brief question-and-answer session with the newly educated patient and family member and present them with a printed list of all of the appointments your nurse has scheduled.
Quick access to your favorite EBM and patient education sites from any location is crucial. Creating bookmarks, or favorites, on your Internet browser is one method for accessing them; however, these favorites are only available on the computer on which you created them and aren't portable from room to room in the clinic or at the hospital. As an alternative, Web sites such as iGoogle allow you to create Web-based, personalized lists of your favorite Web sites, documents and information, which you can access from any computer by logging in to your account (see the screen shot below).
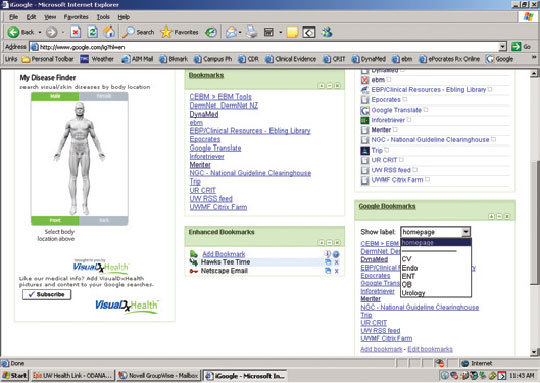
To use this free service, go to http://www.iGoogle.com and follow the instructions to create an account and select the general layout of your page. Then, click on “Add stuff,” select “Gadgets,” search for the “Google bookmarks” gadget and click on “Add it now.” Next, go back to your iGoogle home page, click on “Add bookmark” and type in an address and name for each Web page you want to save. You can also add labels, if desired, to make a bookmark show up on your iGoogle home page (by labeling it “homepage”) as well as under a category of your choice, such as “cardiology.” For example, I've added our University of Wisconsin hyperlipidemia guidelines (http://www.fammed.wisc.edu/our-department/media/614/hyperlipidemia-cholesterol-guidelines) to my iGoogle list. I could access them by doing a Google search or by going through the university's home page, but those routes require multiple clicks to get to the target page. Since I refer to these guidelines often, it is quicker to save them in iGoogle, under a tab I have labeled “cardiology.”
Be careful about bookmarking too many Web sites you won't really use; they can create clutter and inefficiency, much like those old metal filing cabinets. Practice will teach you what is worth saving versus looking up each time. For example, I often look up the exercises for rotator cuff and plantar fasciitis at https://familydoctor.org. Because I can do a Google search for “cuff familydoctor” or “plantar fasciitis familydoctor” and get the handout I need in seconds, there's really no advantage to saving these pages in iGoogle. I have memorized the process on how to find them with the right keywords.
Similarly, my iGoogle page used to include a diagram of fibromyalgia trigger points, but I never used it. So now, instead of storing the link in iGoogle, I can simply do a Google image search (http://images.google.com) for “fibromyalgia trigger points” when I need it. The first hit is a helpful AFP article with the image desired.
Clinical scenario # 4: Learning basic commands and shortcuts
You enter the exam room to find the computer screen locked by the nurse who was using the electronic health record (EHR). You can't log in.
Here are your options:
A: Panic and go searching for someone to help you.
B: Get mad and mumble something derogatory about your nurse.
C: Restart the computer by pushing the power button for three seconds.
D: Calmly use the Alt + Tab command on your PC (or Cmd + Tab on a Mac).
Here are the results you can expect for each option:
A: You waste time, and your patient loses confidence in your practice.
B: You take out your anger on your nurse later in the day – in front of a patient.
C: Restarting wastes time, and because you didn't do a proper shutdown, it damages your patient registry.
D: With two key strokes (Alt + Tab), you quickly see that the clinic EHR is right there for you to log in and proceed with your patient.
The Alt + Tab command is very useful when multitasking with several programs open. For example, you could secure your EHR, which locks your screen, and then use the Alt + Tab command to access other open applications, such as your Internet browser, in which you could open an online symptom index calculator for benign prostatic hyperplasia (http://cpsc.acponline.org/enhancements/238BPHSymptomCalc.html). Your patient could take the quiz on the computer while you see another patient or take care of tasks outside the room, and you wouldn't have to worry about your EHR's security.
Another efficiency tip is to right click on the bottom task bar to “minimize all windows” or “show desktop.” (PC users can also use Win + D for this; Mac users can use the F11 key.) This may be helpful when you have multiple programs open simultaneously (e.g., an e-mail program, a Web browser with multiple tabs active, an EHR, a Microsoft Word document, a Microsoft Access database and a shared network drive folder) and you need to see your desktop again to open a shortcut for your next task.
Learning basic commands and shortcuts such as these can make it easier to find the information you need.
(To download a PowerPoint presentation I've created with more point-of-care practice techniques, click here.)
Practice, practice, practice
As with any learned skill, using online resources at the point of care takes some getting used to. Practice these skills and you'll quickly become comfortable using them in real time with real patients. If needed, take classes on computers, typing and multitasking, or ask a tech-savvy colleague to walk you through the process of using an online EBM resource or setting up an iGoogle page. Don't be afraid of making a mistake or stumbling in front of a patient, or you will never become proficient. Patients are generally understanding and take great interest in this process. Think out loud to the patient as you type. Explain the steps during your search or EHR work so they don't feel ignored. It will fill the silence and give you more time to get the right information. And finally, try to have fun as you learn these new skills. You and your patients may actually enjoy it.