
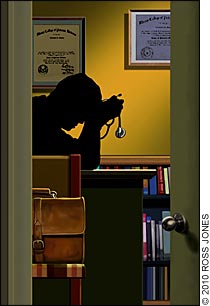
Effectively addressing a colleague's impairement requires care, planning and courage.
Fam Pract Manag. 2010;17(1):27-31
Joseph R. Yancey, MD, CPT, MC, is a family physician practicing in Fort Bragg, N.C. Harry D. McKinnon Jr., MD, LTC (Ret.), MC, is a family physician practicing in Dover, N.H. The authors would like to thank Ms. Elizabeth Brill, MPS, for her assistance in editing this article. Author disclosure: nothing to disclose.
Imagine that you are a family physician in a small, private group practice where for 10 years you've practiced with a colleague we' ll call Dr. D. Dr. D's responsibilities are similar to your own and include both outpatient medicine in your practice and inpatient medicine at three local community hospitals. He has earned a reputation as a superb physician and eager team player. However, in recent months, colleagues and staff have expressed concern to you about behavioral and personality changes in Dr. D. He has become confrontational about trivial things and is increasingly withdrawn. You witness him yelling at a member of the nursing staff over a minor issue. When you approach Dr. D, he is dismissive and states that he is “just stressed out.”
Health care providers and behavioral health professionals have made great effort to characterize psychiatric illnesses such as addiction and depression as diseases rather than as moral failings. Nevertheless, physicians who suffer from such illnesses often have difficulty acknowledging that they are susceptible, while in fact addiction and depression are as common in health care providers as in the general population.1,2 In addition, other mental illness – such as dementia, bipolar disorder or a personality disorder – or physical injury can lead to an inability to safely perform one's duties as a health care provider.3
Any health condition that could interfere with a health care provider's judgment or other faculties needed as a clinician is referred to as impairment. An impaired physician may have deleterious effects on his or her patients and medical group. As a colleague of an impaired physician, you face a tough moral question: What is my responsibility? The importance of intervening with a struggling colleague cannot be overstated. This article offers advice that may enable you to address the situation productively.
Epidemiology
Not only are physicians as likely to suffer from the spectrum of addictive disorders as the general population1, but it has also been suggested that psychosocial factors which influence people to choose the medical profession are also associated with addiction.4 Alcohol, the most commonly abused drug in the United States, is used more frequently by medical professionals than by the general population, although the prevalence of alcohol use among medical professionals is thought to be similar to the prevalence among others of similar socioeconomic status. Physicians as a group are less likely than the overall population to abuse “street” drugs but are more likely to abuse prescription drugs and narcotics, to which they have ready access through self-prescribing or through prescriptions from colleagues. Differences in access to specific drugs are also thought to create variances in drug use among different specialties. Anesthesiologists are more susceptible to narcotic dependence, while emergency medicine physicians are thought to be more prone to illegal drug addictions. Psychiatrists are more likely to abuse prescription mood-altering substances.1
Depression is as common in physicians as in the general population. Gender differences in the prevalence of depression are also similar between physicians and the general population, with 12 percent prevalence for male physicians and 19.5 percent prevalence for female physicians. Suicide rates are higher for physicians than for the general population, and suicide is a disproportionately high cause of mortality in physicians, particularly among female physicians.2
It should be mentioned that data regarding rates of addiction and mental illness are collected by survey or from physicians' health programs. Self-reporting bias in surveys is likely to produce underestimation of the prevalence of impairment. Information from physicians' health programs will not include impaired physicians who are not being treated or those who have sought treatment without informing their health program. Thus, it is difficult to find reliable figures on physician impairment.
Confrontation
The staff has noticed that Dr. D is working very unusual hours. Rumors are swirling that he and his wife are having problems at home. Patient complaints about Dr. D have increased. Many say that he seems tired, constantly distracted and uninterested in conversation. A member of the hospital nursing staff reluctantly mentions to you that she smelled alcohol on his breath.
Most people would agree that it is difficult to confront someone who is impaired. The level of denial, especially for addicts who work in health care, can be surprising and challenging.5 The level of importance that is placed on work by those in the health professions is often very high; as a result, social, financial and interpersonal decay often occur before the addiction interferes with the job. Dr. D's wife and children are likely to have suffered the effects of his illness long before you noticed it at work. By the time a physician's job performance is impaired, the disease is often getting out of control.6
If Dr. D is truly under the influence of alcohol at work, then his patients' safety is being compromised. Even if he has made no overt error, the patient-physician relationship is harmed by his impairment. A physician is less likely to recognize mental illness in a patient while suffering from one himself.2 Colleagues of the impaired physician suffer from increased workloads and a negative work environment. In the event of a malpractice suit, colleagues should expect legal scrutiny, particularly if they knew about the physician's impairment and did not intervene.4
The first approach to Dr. D in the scenario described might be a simple personal communication. A genuine expression of concern – just asking “How are you?” – is a good start, but the denial that comes with impairment often limits the question's effectiveness.7 Most experts recommend a more formal group process known as an intervention. The purpose of an intervention is to present the evidence of impairment to the impaired person in a controlled setting in the hopes of being able to convince him or her to accept help. Participation from co-workers and family members is encouraged, and if possible someone who is experienced with interventions should be present to facilitate the communication. A physicians' health program is a good place to look for a facilitator; contact information for each state's program can be found at the Federation of State Physicians' Health Programs. It is important that those conducting the intervention be prepared to help the impaired physician get treatment immediately following the discussion, including transfer to an inpatient facility as appropriate. Finally, individuals involved in the intervention must establish and clearly communicate consequences for rejecting help, such as suspension of clinic or hospital privileges, a report to the state licensing board and even separation from a spouse.5 Without the threat of consequences, an impaired colleague is less likely to accept help and patient safety remains compromised. (See additional suggestions for interventions in the box below.)
RECOMMENDATIONS FOR SUCCESSFUL INTERVENTIONS
The intervention should be conducted by a team, not an individual.
The team leader should be experienced in interventions.
Team members should be educated about interventions and treatment possibilities.
It is important to collect and evaluate as much data as possible prior to the intervention.
Presentations during the intervention process should be focused on facts.
The team should include only members whose attitude is conducive to the objective tone of the intervention.
Source: Angres D, Talbott G, Bettinardi-Angres K. Healing the Healer: The Addicted Physician. Psychosocial Press; 1998.
Treatment
Dr. D's condition has grown more serious. There are increasing absences from the clinic, more adverse confrontations with staff and more patient complaints. Nurses in the hospital have been paging you to correct some of his erroneous written orders. As a result, you and your partners decide to do an intervention. You anonymously contact your state's physician health program to find someone to assist you with the intervention. After meeting with the intervention expert and conducting a rehearsal, you select a date and time for the intervention. Dr. D enters the meeting to find you, the expert, his wife, two other physicians who know him well and the head nurse for the clinic. Each attendee calmly presents evidence to Dr. D about his impairment, detailing his absences, his behavior at home and at work, and his errors. At the end of the presentation, Dr. D is silent and appears angry. The intervention expert then presents Dr. D with his options: either he reports to an inpatient facility immediately for evaluation and treatment or he will be terminated from the practice and have his hospital privileges suspended. The practice will also file a formal complaint regarding Dr. D to the state medical board if he refuses treatment. Dr. D chooses to report to treatment and boards a plane that evening with bags that his wife has already packed.
Increased awareness of substance abuse among health care professionals in recent years has contributed to an increased emphasis on identification and reporting of concerns as well as on the establishment of monitoring and assistance programs.8 The Joint Commission has recently insisted that “medical staffs implement a process to identify and manage matters of individual physician health that is separate from the medical staff disciplinary function.”9 In addition to local committees at the hospital or medical school level, nearly all 50 states have established programs for identifying and monitoring the impaired physician. These programs are typically composed of an addiction medicine specialist, a psychiatrist and legal counsel. Their overall goal is to provide guidance and resources focusing on the education, rehabilitation and post-treatment monitoring of the impaired physician. The process should not be considered punitive in nature; it is important to treat these physicians as patients rather than criminals. Acceptance and willingness to participate in treatment may depend on this approach.
A treatment plan should be established only after completion of a comprehensive evaluation. The ideal components of a successful treatment program for physicians include these: immediate intervention, evaluation and triage to an appropriate facility, uninterrupted therapy and family involvement followed by rapid re-entry into practice, close monitoring and a contingency plan.10 The evaluation should include identification of any comorbid psychiatric or medical diagnoses that may influence treatment success. Once the initial evaluation is completed, efforts should focus on designing a treatment program best for the individual. Most substance abuse programs include detoxification, rehabilitation, ongoing group therapy and attendance at 12-step meetings such as Alcoholics Anonymous or Narcotics Anonymous.8 In addition, the Caduceus Society offers a support program especially for recovering health care providers. Many physicians will require inpatient treatment because of the severity of their dependence.5
Treatment does not end with discharge from an inpatient program. The ultimate treatment goals are abstinence and successful return to practice, so it is imperative that a realistic and comprehensive outpatient program be initiated immediately upon discharge. Once physicians have completed the inpatient program and demonstrated commitment to an outpatient treatment plan, consideration should be given to returning them to practice. It is common to have the physician sign a contract detailing the expectations for continued recovery and professional conduct.13 In many cases, the contract specifies that failure to adhere to its specific conditions will result in a report to the state licensing board for public citation or potential suspension of license. Periodic monitoring is an integral part of outpatient treatment, and although the specific requirements may vary, the duration is typically no less than five years.8 Inclusion of family members has been shown to produce better outcomes in the treatment and rehabilitation process.11,12
Outcomes
The majority of physicians will return to practice, and prognosis for recovery is better than among the general population.5 A 2008 British Medical Journal article discussing physicians monitored by several state physician health programs shows that 78.7 percent of monitored physicians were licensed and working five years after admittance to a program.14 It may be necessary to modify the work environment for some physicians by decreasing stress levels and restricting access to certain drugs. A factor that may be important to a successful return to practice is the possibility that relapse will entail financial, personal and professional losses. Modifiable factors that contribute to relapse include failure to understand and accept illness, continued denial, a dysfunctional family, poor mechanisms to cope with stress, overconfidence, poor relationship skills, shame and guilt.15,16 Nonmodifiable factors that are associated with relapse are a strong family history of addiction and the use of strong opioids with a coexisting psychiatric disorder.17 The struggle with addiction is often lifelong, and success typically depends on the level of support in both personal and professional settings.
As for Dr. D, he reported to an inpatient treatment facility for addictive disorders that specializes in physician impairment. His practice agreed to pay the required $35,000 for treatment with the understanding that Dr. D will repay the practice over time. Upon admission, a physician presented him with a treatment plan contract, which he signed. A full psychiatric evaluation revealed that he was suffering from depression as well as alcohol dependence. A physician at the center monitored his treatment and started him on a selective serotonin reuptake inhibitor for his depression. He attended twice-daily meetings similar to those of Alcoholics Anonymous. After six weeks of intensive rehabilitation, Dr. D returned home with a plan for continued monitoring.
A few days after returning home, Dr. D returned to work. His partners were eager to see him return, both from collegial concern and because they had been sharing his workload during his treatment period. He admitted that returning to work was awkward, but that everyone had been supportive. His reintegration at home was not as smooth. The pain of past events proved too much for Dr. D's marriage, and his wife filed for divorce. He continues to be monitored by a physician outside the practice and submits to unannounced monthly urine drug testing per his treatment contract. His patients remain unaware of his treatment, having been told only that Dr. D had a prolonged illness.
