
The presenting problem is often just the tip of the iceberg.
Fam Pract Manag. 2012;19(2):22-28
William McLeod is a fourth-year DO/MBA candidate at Kansas City University of Medicine and Biosciences and Rockhurst University. Dr. Eidus is a family physician in private practice in Cranford, N.J., a member of the American Academy of Family Physicians’ National Research Network (NRN), and a participant in DARTNet. His practice also participated in the TransforMed National Demonstration Project. Elizabeth Stewart is director of evaluation for the NRN in Leawood, Kan. Author disclosure: no relevant financial affiliations disclosed.
Does this sound familiar? You glance down at the chart for your next patient visit and see “Mary Jones, 56-year-old female, congestion and drainage for one week.” You cannot remember the last time you saw Mrs. Jones. Upon entering the exam room, you quickly address her chief complaint. Then, trying to squeeze in some preventive care, you ask if she remembers when she last had a mammogram and a colonoscopy. She confirms she had both “a few years ago.” After searching in several possible locations, you can’t find documentation of the colonoscopy in the electronic health record (EHR), and when you finally locate documentation of the mammogram, you see that she’s four years overdue. She’s also two years overdue for blood work for her hyperlipidemia and previous elevated glucose levels. All this EHR detective work has taken several minutes and dozens of mouse clicks, and all the while Mrs. Jones has sat waiting, coughing, and wanting relief for her immediate problem.
Identifying unmet needs
Visits like Mrs. Jones’ demonstrate the three types of needs evident at almost every visit:
The immediate problem (Mrs. Jones’ congestion),
Unmet chronic care needs (Mrs. Jones’ overdue lipid profile),
Unmet preventive needs (Mrs. Jones’ overdue mammogram and possibly colonoscopy).
When a patient is sitting in front of us, we typically see only the tip of the iceberg, the immediate need, as opposed to the full set of needs. Furthermore, we only see the tip of the iceberg for those patients seeing us that day, never mind the hundreds of other patients on our panel who may not be seen for weeks, months, or even years. In the ideal practice, we would be able to view the entire iceberg, but how?
Clinical decision support systems are designed to help us do just that. They augment the EHR with a medical knowledge base (such as evidence-based guidelines) and an inference engine that together generate patient-specific advice and population-level reports.1 Thus, if a patient with diabetes comes in with a sore throat, the clinical decision support system might link the underlying data points and realize that this patient also needs a flu shot. The system is blind to why the patient is coming to the doctor at that moment – the tip of the iceberg – but has the ability to see every other need the patient has. Used correctly, a clinical decision support system can advance your EHR from a glorified word processor to a sophisticated tool that helps you aggregate and synthesize data at the patient and population levels.
This article presents advice for selecting, implementing, and optimizing a clinical decision support system based on the experiences of users participating in the DARTNet collaborative. (See below for more information on DARTNet.)
Picking and implementing a system
As EHRs become more sophisticated, many are providing additional embedded clinical decision support functions with each upgrade. However, many physicians prefer not to use EHR-based systems or wait for the upgrade to their system because EHRs typically require the end user to develop and maintain the knowledge-base algorithms and may not be as robust as stand-alone systems designed to interface with an EHR. (See the list of products below.) If you’re in the market for a decision-support system, we suggest you look for a product that offers, at a minimum, the following features:
Point-of-care reports. These individualized, patient-specific reports (see below) not only summarize the patient’s active diagnoses, medications, labs, risk factors, etc., but also outline the patient’s unmet preventive and chronic care needs such as diabetic foot checks, flu shots, and mammograms. Most of these reports, when viewed on screen, can be designed to display pop-up reminders for patients with specific characteristics. For example, for all patients who have a diagnosis of diabetes, a pop-up reminder might prompt the physician to discuss details of an upcoming group visit.
Overdue reports. These reports (see below) identify patients who have not been seen in the office recently and are overdue for chronic care or preventive services. They serve as a tickler file that prompts the practice to contact these patients and get them in for a visit.
A population registry. The registry (see below) takes the overdue reports one step further by offering a more comprehensive view of the patient panel. Using specific diseases and markers, practices can identify patients with unmet needs and measure clinical performance for quality improvement (QI) purposes.
A direct interface with the EHR system. Every time patient data are updated in the EHR, the clinical decision support system should automatically update as well. This can be helpful for managing medication refills, for example.
Although it takes significant time to interview different vendors and host them for on-site training, do not skimp on this process. Choosing a clinical decision support system is like hiring a new member of the practice. You will need to interview this new “member” carefully, perhaps multiple times, do a test-run, and discuss the workflow integration with others.
You will also need to gain buy-in from the other members of your practice. “You need a core group dedicated to the idea,” said Brian Webster, MD, of Wilmington Health in Wilmington, N.C., and a DARTNet participant. “They are critical to winning over skeptics. And you need some nonphysicians in this group, because everyone in the practice will be affected.”
Eventually, this core group will champion the system by simply going about its daily work and demonstrating the utility of the system and the reports it can generate.
Doug Golding, MD, medical director of Lifetime Health Medical Group in Buffalo, N.Y., and a DARTNet participant, stressed the importance of finding pockets of time to meet with this core group to decide on the clinical content of the application before implementing it. “Our error was rolling out our system without an ‘all eyes on the protocol’ approach,” he said. “You really need to review the content of the tool up front – look at the guidelines as a group, and then decide together how to implement them.” For example, if the clinical decision support system’s guidelines for mammograms are based on the 2009 U.S. Preventive Services Task Force recommendations, the group needs to decide whether to default to those guidelines or customize them.
Golding cautions that a tremendous shift happens the first day the clinical decision support system is on the job. “In one day, you go from being the doctor whose brain alone knows what to do, to now having a tool that tells you what you should be doing all the time,” he said. “It’s like this piece of paper is another member of the care team, and you have to figure out how to integrate this new member with the nurses and medical assistants.”
Although doctors may feel uncomfortable with the idea of a piece of paper telling them what to do, the truth is that the doctor is still in control and must exercise medical decision making. The clinical decision support system is just that – a supporting tool.
Used correctly, a clinical decision support system can enable medical assistants to move from a role of simply processing patients for the physicians to participating in true patient care. “In their old role, the MAs in our group just checked patients in and took their vitals,” said Webster. “Now they are taking some of the history, verifying dates of procedures, requesting reports, and documenting. All of this has also empowered the check-in staff to do more and has allowed them to feel more of a part of the health care team, not just a service desk.”
One critical issue that often gets overlooked at the outset is data storage. For example, most clinical decision support systems cannot read scanned images, so when a document is scanned, the practice will need to enter the data so that the system can later retrieve it. As with any EHR-related component, there will be frustrating glitches as you implement the new system, so anticipate them and keep your eye on the end result, which is better care for your patients.
Optimizing the point-of-care reports
As discussed earlier, point-of-care reports are one of the most useful features of clinical decision support systems. The reports consolidate multiple EHR screens onto a single page, reducing mouse clicks and time spent squinting at the screen instead of looking at the patient. However, this new piece of paper will require the care team to change parts of its workflow.
If your practice team has worked hard to go paperless, nothing will make the team angrier than unexpectedly dropping a new piece of paper in their laps. Explain that the point-of-care report is intended as a one-time snapshot of the patient; it is not part of the permanent medical record. Then tackle the following questions:
Will every physician in the practice use the point-of-care report the same way, or will the practice allow wide variation in workflow depending on physician preference? Jamie Reedy, MD, MPH, medical director at Paramount Medical Group in N. J., says her group took a mixed approach. “We were rolling out the clinical decision support system in multiple practices in our system. We had to be vigilant about the way the data were entered, so we wanted to allow some flexibility in how the point-of-care reports were used,” she said.
Will the report be used as a form of standing orders? If so, how will staff interpret those orders? In the sample report shown above, the section titled “Action Items” includes reminders and standing orders for the medical assistants, such as “Document advanced directives status” and “Document/administer flu vaccine, if applicable.” Although everyone needs time to get used to a system like this, it allows care team members to function at the highest point of their licenses. Of course, every state has different guidelines on what registered nurses, licensed practical nurses, or medical assistants can do with standing orders versus direct physician orders, so someone on the care team should be responsible for confirming the rules in your state and communicating this to everyone.
Where will the piece of paper end up – in the physician’s hand, the patient’s hand, or the shredder? In Reedy’s group, many of the physicians ended up sending the reports home with their patients. “We found patients enjoy seeing their health data in one place, and it encourages them to be more proactive about their own health,” she said.
Population management & quality of care
Although the point-of-care report helps identify the unmet needs of the patient in front of you, it doesn’t address the unmet needs of all the unseen patients in your practice. This is where the power of the overdue report and the registry report come into play.
Overdue reports: As described above, these reports identify patients who are overdue for a needed test, screening, procedure, or follow-up appointment. (See below.) Some systems even allow you to notify patients who are overdue for services with minimal additional work, but you will still need to develop a plan for handling these patients and getting them seen. If a patient receives an automatically generated letter that says she is overdue for a bone density test and calls your office to ask about this, you want the front desk to be prepared to handle the call. One strategy might be to post a short script that front-desk staff can follow to answer common clinical questions the overdue reports may spark.
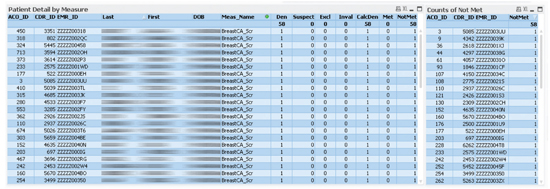
Registry reports: How many of your patients with diabetes have A1C levels under control? How many of your patients age 65 or older received a flu shot this year? Retrospective reports can answer these types of questions and enable you to track quality of care. (See below.) The reports don’t happen by magic; you will need to spend time with the vendor and determine your variables of interest and how you want the data presented. However, the time saved in the long run and the wealth of data you will have at your fingertips can make the exercise worth it.
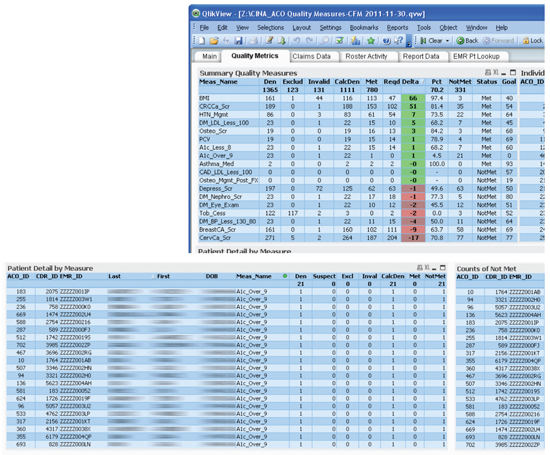
Eventually, use of these reports should result in an increase in the rate of screenings and immunizations in your practice. “The rate of mammograms in eligible patients in my practice now tops 90 percent,” said Webster. “Typically it’s closer to 40 percent in some of the practices in the area.”
Likewise, Reedy’s practice saw marked improvement in 10 out of 13 quality measures in a year-long diabetes QI project.
Financial payback
Implementing a clinical decision support system is a capital investment, with costs varying depending on your ownership structure, group size, type of system, and so forth. On average, high-quality systems will cost between $2,000 and $4,000 for the initial installment and then a nominal monthly maintenance fee. There is also the time investment of researching vendors, training staff, etc. These time and monetary costs are minimal compared to the cost of an EHR.
A clinical decision support system can actually increase practice revenues, as it has done for one of the authors (RE) through a combination of the following: The overdue reports help to increase visits and services – all evidence-based and billable. The point-of-care reports facilitate smoother and faster work-flow, increasing the practice’s capacity to offer expanded services in the same amount of time. The registry reports help increase profitable participation in pay-for-performance programs. Screen shots of these reports can serve as documentation to help obtain patient-centered medical home recognition from the National Committee for Quality Assurance, for example, which brings increased reimbursement from some payers.
CLINICAL DECISION SUPPORT SYSTEM PRODUCTS
Many EHR systems provide clinical decision support functions; however, stand-alone products are also available.
CDS Plus from Anvita Health
CINA’s Point-of-Care Clinical Decision Support Tool
Clinical Xchange from Shared Health
smartConsult from DiagnosisOne
Chipping away at the iceberg
No system is perfect, but a clinical decision support system can help you chip away at the iceberg of patient needs. The next time you see Mrs. Jones, she will already have completed part of her history with the medical assistant, and all preventive services will be covered. You can quickly note whether her chronic care needs are up-to-date and then use any newly found time to have a conversation about lifestyle change and community resources that can support her efforts. When her visit is over, you will have enough time to consider all the other Mrs. Joneses that are not on your schedule that day and how you can better help them.
Rather than being another EHR distraction, a clinical decision support system allows you to focus more on the relationship piece that likely drew you to family medicine in the first place.
DARTNET COLLABORATIVE

DARTNet is a federated research and quality improvement (QI) collaborative that links electronic health record data so that researchers and member practices can work together to answer research questions and provide feedback for QI projects and shared learning. DARTNet is a private-public partnership through the AAFP National Research Network, the University of Colorado, and other academic and health care organizations. See http://www.dartnet.info.
IMPROVING PRACTICE THROUGH RESEARCH

This article is part of a series from the AAFP National Research Network and its affiliates, a national collaboration of primary care practice-based research networks. This series is designed to help family physicians put research results to use in their practices.
