
Medical emergencies may not be common in the office setting, but that's precisely why you need to practice your response to them.
Fam Pract Manag. 2013;20(2):13-18
Author disclosure: no relevant financial affiliations disclosed.
Certain emergencies elicit an immediate, conditioned response. When someone yells “Fire!” for example, most people look for an emergency exit or a fire extinguisher. However, emergency situations in medical offices do not engender the same type of Pavlovian reaction. Although most medical training, including family medicine training, involves learning how to deal with emergency situations, that education has a tendency to wane after graduation. Once physicians are in private practice, with the demands of seeing patients, maintaining emergency certification becomes a lower priority than dealing with day-to-day issues. Many primary care physicians do not invest time in maintaining active certification in cardiopulmonary resuscitation (CPR), much less advanced life support. However, medical emergencies do occur in physicians' offices, including asthma exacerbations, chest pain, hypoglycemia, anaphylaxis, and impaired consciousness, among others.1 Outpatient facilities must be prepared to deal with these situations.
This article describes the emergency preparedness program that our practice, Community Volunteers in Medicine, designed and implemented. Our practice is a busy, mostly volunteer-staff clinic providing medical and dental care as well as ancillary services such as nutrition and diabetes education, and last year we conducted 26,000 visits. Given this patient volume, we felt that everyone on our staff needed to be prepared to deal with medical emergencies. In addition, because we have many volunteer staff who have retired from previous careers, are more than 60 years of age, and have medical issues, we felt it prudent to have measures in place to care for those who help us care for patients.
We recognize that our model may require adaptation for use in other offices depending on the number of staff (including physicians, other providers, and nursing staff), role assignment, proximity to an emergency department (ED), response times of local emergency medical services (EMS), the level of care providers are capable of administering (basic versus advanced life support), and state laws regarding who may provide emergency services. Still, we offer an emergency preparedness model befitting a family medicine office.
Condition C: An emergency preparedness program
We named our emergency preparedness program “Condition C” to avoid the popularized term “code blue,” which could alarm patients in the office and waiting room. The algorithm shown below summarizes the steps involved in our program, which has two major components.
Scavenger hunt. The program begins with a review of all available emergency equipment in the office utilizing an engaging scavenger hunt format. Both nursing and medical staff participate in finding and reviewing the medications and equipment that might be needed in an emergency situation (see the checklist of recommended emergency supplies). Because our office is staffed mostly by volunteers and not all items can be stored within a crash cart or emergency box, the scavenger hunt helps ensure that all staff members are able to access these items in an expedient manner and that the practice is fully equipped. Once staff identify the items, they inspect medications to make sure none have expired and review equipment use. It is imperative that staff know how to use oxygen tanks, injectable epinephrine, and other equipment correctly. Additionally, Condition C cards with common emergency situations and the appropriate interventions are located in each exam room and stored with the emergency equipment. The scavenger hunt confirms the presence of these cards.
Mock codes. The program also involves mock code situations followed by a debriefing to discuss staff members' roles and potential issues that arose during the exercise. We do not inform staff ahead of time that a Condition C is going to be simulated. To mimic the most likely scenario in an office setting, we plant a volunteer in the waiting room or exam room and ask him or her to simulate shortness of breath or acute chest pain. This tests whether our office staff is alert to patients' needs. The goal is to have someone call a Condition C in a timely manner, followed by a rapid response by staff with the appropriate emergency equipment. We try to perform these mock emergencies at least two times per year.
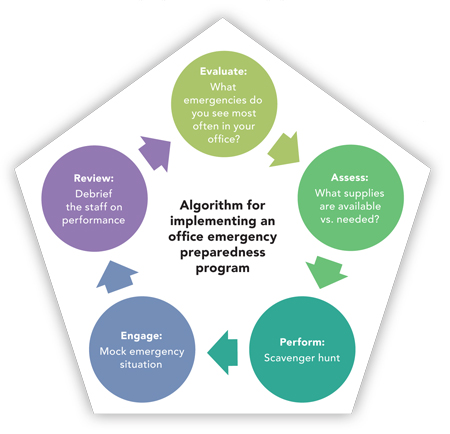
Our emergency preparedness program involves five key steps, depicted here. Additionally, we orient all new staff members to our emergency procedures upon hire, and we review staff members' CPR certification regularly. Although this may seem like an overwhelming task to introduce into a busy clinic schedule, we believe it is worth the time and effort. An alternative would be to incorporate all of these steps into a half-day session and to offer CPR certification
CHECKLIST: EMERGENCY SUPPLIES FOR FAMILY MEDICINE OFFICES
The following checklist of recommended emergency supplies includes many expected items, such as oxygen and nitroglycerin, as well as several items not commonly found in family medicine offices, such as an automated external defibrillator In deciding whether to include a particular item in your practice, consider your staff members' ability to use the item appropriately and your office's access and proximity to emergency services. we revised our system of monitoring medications used for emergencies and assigned a staff member to this task.
| Equipment | Cost |
| □ Automated external defibrillator (AED) | $2,300 |
| □ Bag mask ventilator (two bag sizes and three mask sizes for adult, pediatric, and infant) | $19–$22 per mask and bag |
| □ Blood pressure cuff (all sizes) | $55–$236 |
| □ Glucometer | $10–$40 |
| □ Intravenous catheter/butterfly needles (18 to 24 gauge) | $40 |
| □ Intravenous extension tubing and T-connectors | $1–$2 |
| □ Nasal airways (one set) | $7–$15 |
| □ Nasogastric tubes | $9–$25 |
| □ Nasal cannula for oxygen | $28 |
| □ Nebulizer or metered dose inhaler with spacer and face mask | $30–$80 |
| □ Non-rebreather mask (three sizes) | $2.49 per mask |
| □ Oxygen mask (three sizes) | $1–$2 |
| □ Oxygen tank and flow meter | Tank: $65 (empty) Flow meter: $50–$150 |
| □ Portable suction device and catheters, or bulb syringe | $3 |
| □ Pulse oximeter for child and adult usage | $179 |
| □ Resuscitation tape (color-coded) | $120 for a package of |
| □ Universal precautions (latex-free gloves, masks, and eye protection) | $12 per kit |
| □ CPR barrier device | $9 |
| □ Blood spill cleanup kit | $6 |
| □ Eye wash | $2 |
| □ Cardiac board | $68 |
| Medications | |
| □ Acetaminophen (rectal suppositories) | |
| □ Albuterol | |
| □ Aspirin, chewable | |
| □ Ceftriaxone (Rocephin) | |
| □ Corticosteroids, parenteral | |
| □ Dextrose 25% and 50% | |
| □ Diazepam, parenteral (Valium) | |
| □ Diphenhydramine, oral and parenteral | |
| (Benadryl) | |
| □ Epinephrine injection (EpiPen and EpiPen Jr.) | |
| □ Flumazenil (Romazicon) | |
| □ Lorazepam, sublingual (Ativan) | |
| □ Morphine (MS Contin) | |
| □ Naloxone (Narcan) | |
| □ Nitroglycerin spray | |
| □ Saline, normal | |
| □ Glucagon | |
| □ Atropine | |
| □ Lidocaine | |
| Other | |
| □ ECGmachine | |
| □ Condition C cards | |
| □ Fire extinguisher | |
| □ Panic button | |
Obstacles addressed
One of the main obstacles to effective emergency care that we identified through our mock code situations was a lack of awareness by front office staff of patients in the waiting area. This was because of the layout of our physical space. To combat this issue, we installed surveillance cameras throughout the area, allowing the front office staff to see patients who are not directly visible from their desk.
Additional issues identified through our mock code exercises included slow response times among staff, difficultly finding necessary items, poor documentation of the episode, and slow-downs in patient flow in other parts of the practice. We created the scavenger hunt to improve the ability to find needed items. To improve documentation, we introduced an “Emergency Nursing Record.” This flow sheet includes patient information, emergency type, vital signs, review of systems, necessary interventions, and medications. In the event a patient requires transfer to the ED, we send a copy of this sheet with the patient. In general, this sharing of information helps streamline and improve patient care.
EMERGENCY NURSING RECORD
Immediately following mock emergencies, staff members meet to debrief and discuss problems in how the team responded. This allows all those involved to voice concerns and suggest improvements. Utilizing a debriefing form (see the “Mock Trial Evaluation Form”), we analyze each situation individually. These debriefing sessions help us troubleshoot the program. During a recent mock emergency, we discovered that multiple medications in our emergency box were expired. As a result, we revised our system of monitoring medications used for emergencies and assigned a staff member to this task.
An additional obstacle to running mock emergencies in a busy practice is pushback from staff who say it interrupts patient flow and disrupts those working in the clinic. This was the case at our practice, and getting buy-in was difficult at first. Attitudes changed, however, after a true medical emergency transpired, and our staff witnessed that things went smoothly. In this instance, a patient presented with chest pain and was having an acute myocardial infarction. Condition C was called. The patient was given aspirin, nitroglycerin, and oxygen. The electrocardiogram and flow sheet were copied and sent with the patient to the ED. The emergency physician subsequently called to compliment our clinic for the pre-hospital care. By the time the patient reached the ED, the ST elevations were already resolving.
MOCK EMERGENCY EVALUATION FORM
Date of mock emergency:____________________
| Yes | No | Comments and other information | |
| Placed mock call to EMS immediately | |||
| Airway assessed | |||
| Breathing assessed | Respiratory rate: Description of respiration: | ||
| Oxygen started for respiratory distressed | |||
| Circulation assessed | BP: Pulse: | ||
| Any other initial interventions used | |||
| Patient reassured frequently until mock EMS arrived | At 5 min: At 10 min: | ||
| Head to toe examination | |||
| All supplies required for management of the patient were available | |||
| Supplies requested were found quickly | |||
| Emergency nursing record form was available and/or used | |||
| Personnel knew how to use equipment properly | |||
| Condition C cards were available and/or used | |||
| Leader communicated effectively and roles were assigned | |||
| Events were recorded accurately | |||
| Other: |
Worth the effort
Although implementing an emergency preparedness program is challenging, we believe it is a worthwhile and necessary addition to all family medicine offices. While infrequent, emergency situations do occur in office settings, and this program equips us to provide the best possible care for our patients. Implementing an office emergency preparedness program removes the anxiety of dealing with unusual issues, keeps necessary medications and equipment current and in working condition, and identifies problems prior to an actual emergency so that they can be resolved. It also reduces the risk of malpractice suits arising from poor emergency care in an office setting.
The old adage “practice makes perfect” seems applicable. Though perfection is impossible, all clinicians and staff members must practice their response to medical emergencies in the outpatient setting so they are prepared should an actual emergency arise. Your patient's life may someday depend on it.
