
International medicine offers challenges and rewards while working in a setting far removed from home.
Fam Pract Manag. 2013;20(5):22-26
Author disclosure: no relevant financial affiliations disclosed.
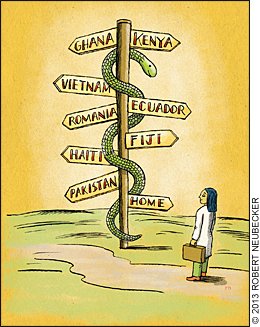
Physicians frequently volunteer to provide medical services in international settings because they want to assist those in need, break out of their daily routine, or expand their personal horizons. Before leaping into international medicine, however, physicians should carefully consider not only the benefits they can expect from such trips but also the professional challenges and personal costs involved.
Professional issues
For some, the best part of working in a developing country is the thrill of stepping outside one's professional comfort zone and treating unusual (at least to the physician) diseases and injuries. But there are special challenges to consider.
Expanded scope of practice. While surgeons, dentists, and anesthesiologists usually work within their own specialty areas when serving abroad, other physicians, such as family physicians, working with nongovernmental organizations are considered generalists and must often widen their scope of practice. That could involve dealing with obstetric and trauma patients, assisting in the operating room, and even administering anesthesia. In such situations, local nurses or physician extenders can provide valuable assistance, gently walking the visiting physician through clinical cases that may be unfamiliar to him or her.
International work may require reviewing how to diagnose and treat diseases and injuries that are uncommon in family medicine practice. Western practitioners have a reasonable concern that their knowledge base may not meet the needs of the developing world, especially with regard to common infectious diseases. Malaria, dengue, cholera, and schistosomiasis may be only a distant memory from medical school. In addition, visiting physicians may be unaccustomed to treating patients with severe malnutrition, more unusual parasitic diseases, snakebites and similar envenomations, and the extremely late presentations of tuberculosis, HIV, and other severe diseases, as well as ruptured ectopic pregnancies.
Pediatrics constitutes much of a physician's practice in the developing world, so it will help to become familiar with neonatal and pediatric resuscitation, including placing intraosseous lines. For those whose skills are rusty, a pediatric advanced life support course may help.
Having trusted medical references on hand will also be helpful. Web access may be unavailable or too expensive to use at the health care facility, so it helps to have some reference materials that do not rely on the Internet (although it may be available in the living quarters). For “portable brains” on a smartphone, an app like Medscape Mobile doesn't need web access, although it will lack embedded photos or videos. Also consider bringing some reference books or eBooks related to resource-poor medical practice. The types of books needed depend on the clinical setting. When leaving, it is a nice gesture to leave the print books behind for local health care providers to use.
Unfamiliar medications. In the developing world, visiting physicians will find the quantity, quality, and types of medications available different from what they're used to, but they must adjust and use medications that are most familiar to local providers and the population. Some commonly used medications abroad, such as chloramphenicol, chlorpromazine, intravenous quinine, and artemisinin-based antimalarials, are rarely used in the United States. In many countries, patients' families need to purchase medications (and sometimes intravenous solutions) before they can be administered. In addition, even if medications are listed on a facility's formulary, many will periodically be unavailable, including oxygen, antihypertensives, snake antivenin, analgesics, and antibiotics.
Equipment availability. Physicians will find that many locales lack much of what they think of as “normal” medical equipment. But unless specifically asked to bring alternative equipment or medications, they should focus on the basic practice essentials: a stethoscope, a penlight, an otoscope, pens, a few masks and sterile gloves for personal use, hand sanitizer to carry while working, and a headlamp to use for procedures or when the lights invariably go out. Making do with alternative equipment and medications is routine (see photo) and considered part of fitting into the local health care system.1

While radiographs may be hard or impossible to obtain in rural or remote areas of developing countries, ultrasound is becoming more common. If unfamiliar with that modality, spend time handling an ultrasound transducer and learn to manipulate the basic knobs on an ultrasound machine before the trip. Ultrasound can be used to diagnose long bone fractures (remarkably easy), pneumothoraces and bladder distention (also easy), or free intraperitoneal fluid (the focused assessment with sonography for trauma [FAST] exam is doable with a little practice).
Health care system limitations. On arrival, learn the local health care system's structure (e.g., whether there is a hospital or specialists nearby and the workplace hierarchy and culture) to accelerate adjustment to the new setting. One excellent way to start is to obtain a formal introduction or introduce oneself directly to the facility's head administrator. In most circumstances, this is the proper etiquette and will demonstrate a respect for the culture and the facility.
The health care facilities themselves may shock first-time international physicians. While major medical centers in the largest cities sometimes approximate Western standards, the majority of the developing world's health care facilities are rudimentary, with marginal cleanliness, sterility, and upkeep, and unreliable electricity, cooling, and lighting. Most advanced therapies will not be available at all. Visiting physicians must be ready to accept this reality; some patients may die who would not have died in a hospital in a more developed country.
Ancillary services and access to surgeons, dentists, anesthetists, testing laboratories, and ventilators may not be available or available only at distant locations or during specific hours. Consultations may also be difficult, although some specialist advice could be possible through the Internet from colleagues at one's home institution. Commonly, these will be in dermatology, ophthalmology, or orthopedic surgery when pictures can be sent via email.
Professional and patient communication. Language will invariably be a barrier. People in English-speaking countries don't necessarily speak the same type of English; the same is true of French, Spanish, and Arabic. In some countries, only the professionals and politicians speak the official language with ease. Most of the population speaks one or more native or regional language, so visiting physicians have to rely on translations, usually through the local health care workers with whom they work.
When speaking with local health care professionals in English, the vocabulary, including medication and laboratory test names, may vary considerably from that used in the United States. The table below shows the variations in common medical terms between Kintampo, Ghana, where English is the official language (although the country has about 81 different languages), and the United States.2
As in any system, the quality of local health care professionals will vary, although in most cases they will far exceed expectations. Visiting physicians who are ready to learn from their new colleagues, and teach them in return, will benefit the most from their international experience.
Kintampo, Ghana | United States |
|---|---|
| Zone | Ceftriaxone |
| Paracetamol* | Acetaminophen |
| Largactil* | Chlorpromazine |
| Pethedine* | Meperidine |
| ATS | Tetanus toxoid |
| ASV | Snake antivenin |
| Full Blood Count (FBC) | Complete Blood Count (CBC) |
| MPS | Thick smear-malaria |
| ICT | HIV test |
| Road Traffic Accident (RTA)* | Motor Vehicle Collision (MVC) |
Personal issues
Besides professional issues, there are also several personal factors that often determine whether a physician can choose to do international medicine.
Availability and costs. Family responsibilities and finances can dominate a decision to work internationally. Will the assignment be short or long term? Will family members be able to accompany the clinician? Some organizations pay part or all of a physician's actual expenses, and long-term assignments of a year or more may also include a salary. Depending on the organization and destination, it may be possible to bring family members along or meet them for a subsequent vacation, but that again depends on costs and lost wages. Organizations rarely pay for accompanying family unless the position involves an extended stay.
Living arrangements. Living conditions will be very different and, depending on the locale, rudimentary. For example, accommodations vary widely, from tents to ships to houses or apartments. Some offer private rooms, while others feature multi-person sleeping quarters. Likewise, amenities vary, with only some sites providing laundry, cooking, and cleaning services. As for eating, the gastronomically unadventurous will have to find out whether the locale has food that is personally appealing, available, and safe.
Traveling to remote areas often includes dealing with routine power outages, lack of running water, primitive toilet facilities, no hot water, the presence of dangerous animals, or a nightly ruckus from chickens, roosters, dogs, or snoring bunkmates. But this is also the basis for great tales when travelers return home.
Expect travel in a developing country, particularly airline and bus schedules, to be inconsistent and fluid, with trips often being cancelled without notice. If traveling by road, find safe drivers and always wear seatbelts as most American deaths overseas result from motor vehicle crashes, rather than crime, terrorism, the environment, or diseases.3
That said, personal security is still important. For all travelers, the best security is based on common sense and experience. The keys to staying safe are to remain alert, maintain a low profile, trust your instincts to tell you when something is amiss, and closely observe your environment.
Communication is essential for international travel and is getting better in developing countries. Learn whether and what types will be available and their costs. Cell phone service has become much more common in remote areas, although it is usually better in urban settings and “roaming” charges are often obscenely high. A mobile phone programmed to work with any cellular network is often the cheapest way to communicate locally with fellow health care providers or friends. If the Internet is available, stay in touch via email, Facebook, Twitter, or a video conferencing service like Skype.
Health risks. In most developing countries, infectious diseases pose a major threat, not only to the local populace but also to visiting physicians. The Centers for Disease Control and Prevention's travel website is the best source of current information on which immunizations are needed for each country. Begin this process early, since some immunizations may be difficult for physicians to obtain (use a university travel clinic for the fastest results). In addition, live virus vaccines provide the best protection if given at least 28 days apart (at least 30 days for yellow fever vaccination), and some must be given weeks in advance (e.g., rabies preimmunization) or months in advance (e.g., primary tetanus immunization). Track all immunizations on the International Certificate of Vaccination, often referred to as the “Yellow Card,” which should always be kept with the passport.
Despite immunizations, travelers in endemic areas still need to take malaria prophylaxis. Talk to the travel clinic provider to determine which one to use. However, since none of these medications is 100 percent effective and immunization against dengue is not yet available, the other vital precaution is to use a good (100 percent DEET) mosquito repellent day (against dengue) and night (against malaria). Also, use an insect-protective bed net and, where available, sleep in an air-conditioned room, which reduces mosquito activity.
Immunizations also do not protect against traveler's diarrhea. Carry loperamide, but recognize that diarrhea may also be infectious or a sign of other significant disease. Finally, have medical insurance, evacuation insurance, and an evacuation plan. Bad things happen at the worst times.
Benefits of international work
Physicians who practice international medicine, either in short spurts or for extended periods, will probably gain more from the experience than their patients. It's hard for a single physician or even a single nongovernmental organization to make a significant impact on the world's health care woes. In fact, except for missions with specific objectives, such as disaster relief, clinical education, research/publication instruction and supervision, or high-impact surgery (e.g., cataract removal, cleft lip/palate reconstruction, or vaginal fistula repair), the costs involved in doing international medicine work would arguably be better used to fund global medicine projects involving long-term services that improve public health.
That said, international experiences can make a difference. Above all, they allow physicians to grow personally and professionally by constantly working at the edge of their comfort zone. Most physicians return with a deeper empathy for other cultures, greater flexibility, improved language abilities that they can use in their practice (particularly Spanish), and even ideas for better organizational or clinical methods. These experiences also provide the satisfaction of helping patients who may not otherwise have had the benefit of expert medical care. U.S. physicians also may be able to assist local health care providers by providing education and collaborative research, which can be continued via email after returning home.
Finally, there is the adventure of working in an unfamiliar and remote area, the possibility of tourism during time off, and the opportunity for true cultural immersion while working alongside local health care professionals and their patients.
Editor's note: For more information on international health care opportunities, see the article “Working With International Populations - Abroad or in Your Own Backyard.”
