
Burnout is everywhere, but you can't fight an enemy unless you recognize it.
Fam Pract Manag. 2015;22(5):42-47
Author disclosure: Dr. Drummond is an author, speaker, and consultant on the subject of physician burnout.
© 2015 Dike Drummond, MD, CEO, TheHappyMD.com

There is an epidemic of physician burnout in the United States, and it has a pervasive negative effect on all aspects of medical care, including your career satisfaction. According to one researcher, “Numerous global studies involving nearly every medical and surgical specialty indicate that one in every three physicians is experiencing burnout at any given time.”1 The 2015 Medscape Physician Lifestyle Survey reported an even higher burnout rate – 46 percent of physicians, up from 39.8 percent in the 2013 survey.2
At your next physician staff meeting, take note of your colleagues sitting on either side of you. At least one of you is likely experiencing burnout.
Lower patient satisfaction and care quality,
Higher medical error rates and malpractice risk,
Higher physician and staff turnover,
Physician alcohol and drug abuse and addiction,
Physician suicide.
Yes, burnout can be a fatal disorder. Suicide rates for both men and women are higher in physicians than the general population and widely underreported.9
So, before we go on, let's agree that physician burnout is bad on multiple levels – bad for doctors and their families, bad for staff and patients, and bad for organizations. And burnout is everywhere, all the time.
Unfortunately, although physician burnout is incredibly common and damaging, it remains a taboo subject in the workplace. Stress management and burnout prevention are not covered in detail in medical school or residency training.
In this article, we will fill this hole in your medical education by exploring burnout's origin, cardinal symptoms, and five main causes. In future articles, we will explore multiple, field-tested burnout prevention tools to help you lower your stress level and build more life balance and a more ideal practice.
IN THE AUTHOR'S OWN WORDS
Dr. Drummond explains the concept of an energy account and its role in physician burnout.
The origin of physician burnout
Burnout originates from a disorder of energy metabolism. This is not the Kreb's cycle. It is more like “the force” in Star Wars. A common metaphor for burnout is the battery. Physicians often discuss exhaustion and burnout as a state where, “My batteries are just run down.” This battery metaphor is at odds with reality for the following reasons.
When a toy's battery runs out, what does the toy do? It stops working. When did you ever stop working – ever? The answer is likely “never” because if you had stopped working at any time during medical school, residency, or practice, it would have had a negative effect on your career.
A much more accurate and useful metaphor for burn-out is the energy account. Like a bank account, it can have a positive or negative balance. You withdraw energy from this account for the activities of your life and medical practice. You deposit energy into this account during times of rest and rebalance. When you dip into a negative balance, the account does not get closed. You keep spending (or working) despite the fact that your energy account is depleted. (See “Your energy account: full or empty?”)
YOUR ENERGY ACCOUNT: FULL OR EMPTY?
We withdraw energy from this account for the activities of our life and work. We deposit energy to this account during times of rest and rebalance. Burnout occurs when there is a negative balance over time.
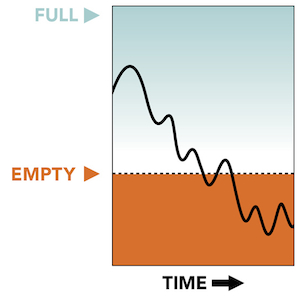
Burnout is the constellation of symptoms that occur when your energy account has a negative balance over time. You can continue to function in this depleted state; however, you are a shadow of the doctor you are when your account has a positive balance.
There are actually three types of energy accounts inside each of us:
Your physical energy account. You make energy deposits here by taking care of your physical body with rest, exercise, nutrition – all the things we learned not to do in our training.
Your emotional energy account. You make energy deposits here by maintaining healthy relationships with the people you love – your friends and immediate family. Recharge here is essential if you are to have the energy necessary to be emotionally available for your patients, staff, family, and friends.
Your spiritual energy account. You make deposits here by regularly connecting with your personal sense of purpose. In your practice, this occurs when you have an ideal patient interaction. This is the visit where you say to yourself afterwards, “Oh yeah, that is why I became a doctor.” You can connect with purpose outside of work as well. One example for me is when I coach my children's youth soccer teams. If you go long periods without connecting with purpose, this account is drained and you may have a lot of trouble seeing a reason to carry on.
As physicians, we each have a moral imperative to keep our energy accounts in a positive balance because of a physical reality I consider to be the first law of physician burnout: “You can't give what you ain't got.” If you remember nothing else from this article, please remember this law.
Your best work and your best life depend on your ability to manage these energy levels. Your leadership skills, quality patient care, empathy, your skills as a spouse and parent – all of these rely on a positive energy balance. And yet we are not trained to notice or care for our energy levels. Instead, we are conditioned to ignore our physical, emotional, and spiritual energy levels and carry on despite complete exhaustion of our energy reserves, placing us at very high risk for burnout.
Burnout's three cardinal symptoms
The accepted standard for burnout diagnosis is the Maslach Burnout Inventory, developed by Christina Maslach and her colleagues at the University of San Francisco in the 1970s. She later described burnout as “an erosion of the soul caused by a deterioration of one's values, dignity, spirit, and will.”10 Here are the three main symptoms (which correspond with the three energy accounts we just discussed):
Exhaustion. The physician's physical and emotional energy levels are extremely low and in a downward spiral. A common thought process at this point is, “I'm not sure how much longer I can keep going like this.”
Depersonalization. This is signaled by cynicism, sarcasm, and the need to vent about your patients or your job. This is also known as “compassion fatigue.” At this stage, you are not emotionally available for your patients, or anyone else for that matter. Your emotional energy is tapped dry.
Lack of efficacy. You begin to doubt the meaning and quality of your work and think, “What's the use? My work doesn't really serve a purpose anyway.” You may worry that you will make a mistake if things don't get better soon.
Recent research shows that men and women suffer from exhaustion and compassion fatigue equally. However, symptom three, “lack of efficacy,” is much less common in men. Male physicians are far less likely than female physicians to doubt the meaning and quality of their work, no matter how burned out they are.11
Burnout can happen slowly over time in a chronic grinding fashion – the classic “death by 1,000 paper cuts.” It can also crash down on you in a matter of minutes when it is triggered by a traumatic outcome, lawsuit, devastating medical error, or equally tragic circumstance in your personal life.
The five main causes of burnout
In more than 1,500 hours of one-on-one coaching experience with burned out physicians, here are the five causes of burnout I see most often.
1. The practice of clinical medicine. Being a physician has been and always will be a stressful job. This is a fundamental feature of our profession for a simple reason. We are dealing with hurt, sick, scared, dying people, and their families. Our work takes energy even on the best of days. Our practice is the classic high-stress combination of great responsibility and little control. This stress is inescapable as long as you are seeing patients, no matter what your specialty. As you read on, note that this is the only one of the five causes of burnout we actually learn to cope with in our training.
2. Your specific job. On top of the generic stress of caring for patients, noted above, your specific job has a set of unique stresses. They include the hassles of your personal call rotation, your compensation formula, the local health care politics associated with the hospital(s) and provider group(s), the personality clashes in your department or clinic, your leadership, your personal work team, and many, many more.
You could change jobs to escape your current stress matrix, but your next position would have all the same stressors at different levels of intensity. It is tempting to believe a different practice model would be less stressful. However, moving from an insurance-based practice model to concierge or direct pay, or from an independent setting to an employed setting, simply switches one set of stressors for another.
3. Having a life. In an ideal world, your personal life is the place where you recharge from the energy drain at work. Two major factors can prevent this vital activity:
We are not taught life balance skills in our medical education. In fact, our residency training teaches us just the opposite. We learn and practice ignoring our physical, emotional, and spiritual needs to unhealthy levels and then carry these negative habits into our career. You work until you can't go any longer, and then you keep going. To do otherwise could be seen as a sign of weakness. (See cause No. 4 below.)
Multiple situations could arise at home that eliminate the opportunity to recharge your energy account. Your life outside your practice then switches from a place of recharge and recuperation to an additional source of stress. The causes range widely from simple conflicts with your spouse to illness in a child, spouse, or parent to financial pressures and many more. You may have seen this in a colleague who suffered the downward spiral of burnout at work in the absence of any new work stress. If you reach out to a colleague who appears to be burned out, you must ask, “How are things at home?” to reveal this burnout cause.12
4. The conditioning of our medical education. Several important character traits essential to graduating from medical school and residency emerge during the premed years. Over the seven-plus years of our medical education, they become hard wired into our day-to-day physician persona, creating a double-edged sword. The same traits responsible for our success as physicians simultaneously set us up for burnout down the road. Here are the top four character traits I see in my physician coaching practice and how to identify this programming when you are in its grip:
Workaholic – Your only response to challenges or problems is to work harder,
Superhero – You feel like every challenge or problem sits on your shoulders and you must be the one with all the answers,
Perfectionist – You can't stand the thought of making a mistake – ever – and hold everyone around you to the same standard,
Lone ranger – You must do everything yourself and end up micromanaging everyone around you.
In addition, we physicians absorb two prime directives. One is conscious and quite visible: “The patient comes first.” This is a natural, healthy, and necessary truth when we are with patients. However, we are never shown the off switch. If you do not build the habit of putting yourself first when you are not with patients, burnout is inevitable.
The second prime directive is never stated, deeply unconscious, and much more powerful: “Never show weakness.” To understand this programming, try this thought experiment. Imagine you are back in your residency. A faculty member walks up to you and says, “You look really tired. Is everything OK?” How would you respond – and how quickly would that response come out of your mouth? Most of us would immediately answer that we are “fine.” This knee-jerk defense makes it difficult to help physician colleagues even when their burnout is clear to everyone on the team.
Put the five personality traits together with the two prime directives, and you have the complete conditioning of a well-trained physician. Combine this with a training process that is very much like a gladiator-style survival contest, and doctors become hard wired for self-denial and burnout.
5. The leadership skills of your immediate supervisors. Outside of health care, there is a management saying, “People don't quit companies; they quit their boss.” There is wide acceptance that your work satisfaction and stress levels are powerfully affected by the leadership skills of your immediate supervisor.
We know this is true for physicians too. A recent study shows a direct relationship between the quality of your boss and your burnout and job satisfaction levels.13 In this era in which physician groups are forming much more quickly than they can find trained doctors for their leadership positions, having either an unskilled or, worse, an absent boss to report to is common. This fifth cause of burnout has only recently joined the classic four above. It is a significant source of stress for many employed physicians.
How can you recognize when you are burning out?
When our energy accounts drop into negative balance, most physicians react by going into “survival mode” at work. Instead of finding adventure, challenge, and enjoyment in your practice, you find yourself putting your head down and simply churning through the patients and paperwork, focused on simply making it through the day and getting back home. A common thought at this point is, “I am not sure how much longer I can go on like this.” Survival mode and this voice in your head are signs that you are well into burnout's downward spiral. It is time to take different actions to lower stress and get some meaningful energy deposits ASAP.
How can we stop or prevent physician burnout?
There are two fundamental mechanisms to drive a positive balance in your energy accounts and avoid burnout:
Lower your stress levels and the drain they produce,
Improve your ability to recharge your energy accounts.
Most physicians will use a combination of both methods to treat and prevent burnout. We will discuss multiple tools in both categories in two upcoming articles. (See “Series overview.”)
SERIES OVERVIEW
In this three-part article series, we will explore the following:
Part 1: Burnout's symptoms and causes (this article),
Part 3: Proven methods to recharge and create more life balance.
But before we end this introductory article, let me remind you of two things that stop many physicians from preventing burnout:
The comprehension trap: The tendency to study a concept until you understand it, and then fail to put it into action. Because of our long history in the educational system, most physicians will study until we feel confident we could answer a multiple-choice question like the ones on our board exam. Then we often fail to translate this new knowledge into new actions. Do not let this happen to you. As you read the articles in this series, pick an action step that makes sense and take it. The only way to tell what will work for you is to take new actions and notice your results. Expecting a different result from new comprehension alone is insanity; see below.
Einstein's definition of insanity: “Doing the same things over and over and expecting a different result.”14 Free yourself from your workaholic conditioning. If you notice your own burnout and simply double down on the things you are already doing to get more done in the office or hospital, your workaholic conditioning has trapped you here in Einstein's insanity definition. Once again, the only way to get different results is to take action – different actions than you are taking right now. You don't necessarily need to take more actions, just different ones.
This is article one in a three-part series on preventing physician burnout. The first step in prevention is to recognize burnout as it arises. You now know burnout's causes, effects, prevalence, and pathophysiology. In future articles, I will show you multiple tools to lower stress and create life balance. Each of these techniques has been tested in the real world by physicians just like you.
You can see your programming now. You are awake and able to recognize the burnout all around you. Your best next step is to pick a new tool from this article series and try it out. Remember, you can't give what you ain't got. It is time to start managing your energy accounts intentionally and on purpose. Your patients, staff, and family are counting on you.
For more resources on improving physician well-being, visit the AAFP’s web portal Physician Health First.
