
A review of the broad market trends can help you evaluate the specifics of your contract.
Fam Pract Manag. 2016;23(4):28-32
Author disclosures: no relevant financial affiliations disclosed.

Family physicians are trained to employ both objective data and direct observation when diagnosing a patient, considering the general context of the patient's life circumstances as well as specific health metrics before making a treatment determination.
The process of evaluating a physician employment contract is somewhat similar. It begins with an understanding of the broad market trends shaping physician employment agreements and continues with an examination of contract specifics.
This article will explore both of these factors – market trends and contract specifics. It relies on statistics from one physician recruitment firm, Merritt Hawkins, our employer; however, the data echo trends reported elsewhere.1
Four market drivers
The salaries, signing bonuses, and other perquisites offered to family physicians in employment contracts today are shaped by four key market drivers.
1. The physician shortage. The Association of American Medical Colleges (AAMC) projects a national deficit of up to 90,400 physicians by 2025.2 Nowhere is this more evident than in family medicine. Family physicians remain at the top of the wish list for hospital and medical group administrators, and 2015 marks the tenth consecutive year that family physicians have been the most requested search assignment for our search firm. Rounding out the top 10 are psychiatrists, internists, hospitalists, nurse practitioners, obstetricians/gynecologists, neurologists, orthopedic surgeons, pediatricians, and dermatologists.
One factor exacerbating the physician shortage and accelerating demand for family physicians is the proliferation of alternative sites of service. In an age of “convenient care,” patients want to access physician services the same way they access other services or goods – quickly and easily. As a result, family physicians now have an enviable level of practice options and flexibility, from traditional practice settings to urgent care centers and more.
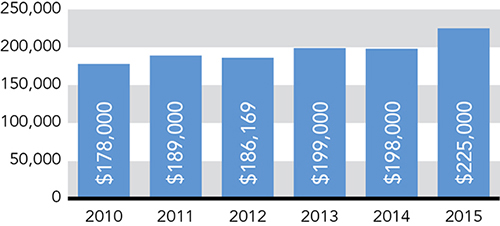
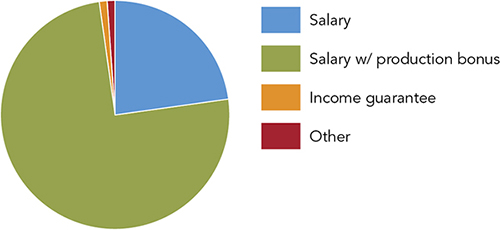
The physician shortage combined with the competition caused by emerging sites of service has created an upward trajectory for family physician starting salaries. In 2015, the national average rose to $225,000; it was $198,000 a year earlier. (See “Average starting salaries for family medicine.”) Base salaries with a production bonus are now the norm, while income guarantees are virtually a thing of the past. (See “Types of physician compensation structures.”)
2. Consolidation. A second market driver is facility consolidation. There were 100 hospital mergers in 2014, up 14 percent from 2013,3 and both hospitals and medical groups are becoming larger in order to achieve economies of scale and compete for managed care/population health contracts. Instead of recruiting three or four primary care physicians at a time, large integrated health systems or accountable care organizations may recruit (or buy the practices of) 30 or 40 primary care physicians. At that point, physician contracts must be reconsidered and aligned organization-wide, creating a growing amount of contractual volatility in the employment market.
3. Employment. The trend away from private practice and toward physician employment is a third key market driver. In 2004, only 11 percent of our firm's search assignments featured hospital employment of the physician. In the prevailing model at that time, hospitals would fund the recruitment of new physicians who would be established in private practice through an “income guarantee.” An income guarantee essentially is a loan that must be paid back, though any monies owed by the physician at the end of the contract period may be “forgiven” by the hospital in exchange for the physician's commitment to remain in the community for a stipulated length of time.
In 2014, by contrast, 64 percent of our firm's search assignments featured direct hospital employment of the physician. Additionally, approximately 90 percent of the 3,300-plus search assignments we conduct annually feature direct employment of the physician by one kind of facility or another, be it a hospital, medical group, or other entity. Less than 10 percent feature true independent practice settings, such as partnership arrangements or solo practice, compared with 22 percent less than a decade ago. These percentages do not take into account practices that recruit directly, and they do not suggest that independent practice is dead, but there has clearly been a strong shift toward direct hospital employment of physicians.1
4. Volume to value. The fourth, and most dynamic, market driver shaping physician employment contracts today is the ongoing effort to transform physician and other provider payments from volume-based models to value/quality-based models. This trend was accelerated in 2015 when the Centers for Medicare & Medicaid Services (CMS) announced a goal of tying 30 percent of Medicare payments to quality by the end of 2016, and 50 percent of Medicare payments to quality by 2018. According to a March 2016 announcement, CMS has already achieved the first goal.4
Currently, however, volume-based metrics such as relative value units (RVUs), present in 58 percent of contracts, continue to be the primary mechanisms by which physicians achieve bonuses. (See “Common bonus metrics.”) Quality metrics are growing, present in 32 percent of contracts, up from 7 percent in 2011, but many employers are struggling with how best to measure quality or value. Common quality metrics include the following:
Exceeding average patient satisfaction scores,
Correctly documenting charts,
Appropriate coding and billing,
Citizenship (peer review, community relations, etc.),
Participating in quality improvement,
Patient safety,
Clinical process effectiveness,
Efficient use of resources,
Population/public health participation.
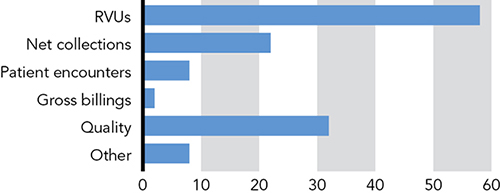
Our firm's 2016 Review of Physician and Advanced Practitioner Recruiting Incentives found that of contracts featuring a production bonus, quality metrics accounted for an average of 29 percent of the overall bonus amount. Consider the case of a family physician earning a base salary of $200,000 who has achieved all of a possible $50,000 bonus. If 29 percent of that bonus is based on quality/value metrics (a total of $14,500), then quality metrics will determine only about 6 percent of the physician's overall compensation of $250,000. That may not be enough to influence physicians to embrace the behaviors that quality metrics are intended to encourage.
For now, in the “real world,” quality based physician compensation remains more smoke than fire. As an article in the March 2016 edition of Health Affairs demonstrates, approximately 95 percent of physician encounters resulted in fee-for-service payments in 2013, while only about 5 percent resulted in capitated payments, which typically feature a quality component.5
That said, major changes are on the horizon. In April 2015, the Medicare Access and CHIP Reauthorization Act (MACRA) repealed the sustainable growth rate mechanism of Medicare payments to physicians. The legislation makes the fee-for-service model less attractive in an attempt to move physicians to a fee-for-value model. By 2021, quality/value scores could impact physician Medicare payments plus or minus 9 percent (with larger increases possible). (For more on MACRA, see “Medicare Payment Reform: Making Sense of MACRA,” FPM, March/April 2016.)
It is important now, and will be even more important in the future, for family physicians and other doctors to understand to what extent and in what way their compensation will be driven by quality/value metrics. Though volume-based payments will remain a significant component of physician compensation, upside potential will be increasingly determined by how well physicians perform in quality and value-based compensation models. Physicians often do not react favorably to the compensation formula changes that are increasingly prevalent in today's market, but these changes frequently are a result of larger, integrated entities struggling to align incentives and reach organizational goals built around quality and cost containment that they have not attempted before. For good or ill, contractual changes after and even during the stipulated contract period are becoming a fact of life.
Beyond the salary: signing bonuses, CME, and more
As noted earlier, market forces have led to an increase in starting salaries for family physicians, which now average $225,000 per year. In addition, family physicians are being offered attractive benefits such as signing bonuses, continuing medical education (CME) allowances, and relocation allowances.
Signing bonuses. Over the last 12 months, signing bonuses were featured in 77 percent of physician employment contracts that our firm tracked. Signing bonus amounts averaged $26,889, but ranged from a low of $1,000 to a high of $275,000.
Signing bonuses, which are offered in addition to base salaries, were once relatively rare in physician contracts but have become common as competition for physicians has increased. They act as an additional motivation for physicians to commit to an opportunity and may make it more practical for physicians to disengage from their current practice and home.
CME. CME allowances were offered in 97 percent of search assignments in the previous 12 months. They averaged $3,649, but ranged from a low of $500 to a high of $35,000.
Relocation. Relocation allowances, another standard perk in physician contracts, were offered in 84 percent of search assignments in 2015. They averaged $8,649, but ranged from a low of $2,500 to a high of $25,000.
Other benefits. Physician employment contracts also typically feature a range of other benefits, including health insurance (99 percent of contracts), malpractice insurance (99 percent), disability insurance (97 percent), and retirement benefits (96 percent). Educational loan forgiveness is not as common (26 percent). In addition, some employment agreements offer on-call compensation, with an average rate of $400 to $500 a day for primary care.
What about the style of practice?
Salary and benefit data offer one yardstick by which to measure physician employment agreements, but other key elements within a contract can reveal the overall character of the practice. It is important to review these elements to ensure the practice style is compatible with your personal preferences and needs. For example, some contracts are structured to be more entrepreneurial and incentive-laden while others reflect a more flexible approach characterized by controllable, lifestyle-friendly schedules.
It is not unusual for residents, in particular, to overlook some of these characteristics and select a practice based solely on its geographic location. When they subsequently realize that their work environment trumps location, they must decide whether to tough it out or move on to a new practice. This can happen to physicians of all experience levels who do not closely examine practice parameters outlined in the employment agreement.
To avoid a mismatch, physicians should carefully read the employment agreement, noting questions such as the following.
Call. Is emergency room call coverage required? If so, is it assigned or unassigned? Is there on-call compensation? Some contracts will say there is no call, but does that really mean no call, or are there exceptions?
Productivity. How is productivity measured? As noted earlier, the most common productivity bonus metric is still RVUs. If the practice uses RVUs, what is the formula?
Inpatient care. What is the inpatient census of the practice? Who is responsible for rounding on inpatients? Often, this work is being turned over to hospitalists, but not always.
Non-visit work. What is the payment policy on phone calls or prescription refills? This is most likely unreimbursed work, but it can consume a significant amount of time, so some practices are beginning to pay for it.
Work schedule. What are the expectations in terms of work hours? Some employment agreements stipulate that the physician be present during “normal hours of operation,” but what does that mean – e.g., eight half-days, four days a week? Is the practice open in the evenings or on weekends? An increasingly important consideration, particularly for younger physicians in their child-rearing years, is whether there is schedule flexibility. More practices today say they are open to part-time schedules or practice sharing, but it is important to ensure schedules are verified in writing to prevent “schedule creep.”
Paid time off (PTO). How much PTO is allowed? Four to five weeks per year is typical for family physicians, although this can be negotiated. How much PTO can be used for vacation versus sick days or other personal leave?
Concierge/direct pay options. This is an area of increasing interest. Do physicians have the opportunity to build their own concierge/direct pay patient base while continuing to accept third-party payments from the majority of patients? If so, is the concierge/direct pay reimbursement pooled together or paid separately to individual doctors?
Partnership. Is there a path to partnership? If so, how long is it? Typically the time frame to partnership is two years (62 percent of our contracts) or immediate to one year (36 percent of contracts). Prolonged paths to partnership are a thing of the past.
Potentially thorny issues: non-competes, privileging, termination, and tail
In today's market, most large physician employers do not seem to be particularly concerned about non-compete agreements, as few physicians are likely to leave the fold to set up practice on their own. If employers are concerned about this, the non-compete clauses featured in their employment agreements usually are iron clad. In those cases where non-competes are an issue, they may impact a physician's desire to moonlight. Physicians who do have such an interest should obtain permission in writing.
Similarly, some physicians may wish to pursue outside business interests, such as patents, clinical trials, devices, or speaking engagements. Such income should be considered separate from the physician's salary and production bonus and be stipulated as such in the agreement.
The employment agreement should also state at which facilities the physician is required to have admitting privileges. Physicians should not be prevented from obtaining privileges where they wish. In addition, there should be no language in the agreement, specific or implied, tying physician compensation to volume of patient referrals. This is a violation of federal fraud and abuse and tax laws, as are salaries or income guarantees that are beyond what is customary and reasonable in a given specialty. For family physicians, salaries of $400,000 or more may be likely to raise red flags.
The standard period for termination is 30 to 90 days without cause. Physicians should not have to stay at the facility or practice for several months or more if they are not satisfied or are uncomfortable. Termination for cause is usually for clear offenses. However, physicians should be cautious if the contract states they can be terminated “for cause in certain instances at the sole discretion of the corporation.” If this is the case, the definition of “certain instances” should be explained.
Larger employers today usually pick up tail insurance when a physician leaves the practice as a matter of course. However, if physicians leave without cause during the contract period, the obligation to obtain such insurance may be on them. This can be significant, as the cost of tail coverage is often between 1.5 and two times a physician's annual premium.
A strong but evolving market
The doctor shortage and other market factors have led to an employment market that is particularly favorable to family physicians, increasing compensation offers, practice setting choices, and practice flexibility.
Family physicians evaluating their practice options should consider that physician employment agreements are rapidly evolving, as is the health care system itself. Relatively straightforward agreements that reward family physicians for the volume of work they do are giving way to agreements that feature more nuanced and subjective quality/value-based metrics. Family physicians should pay particular attention not just to how much they are likely to earn but also to what measures their performance and compensation will be based on. In addition, they should closely examine the parameters of the practice as stipulated in the agreement to ensure the style of practice matches their professional wants and needs.
