On-screen alerts can help a spread-out staff work together to keep patient care moving smoothly.
Fam Pract Manag. 2016;23(5):28-30
Author disclosure: no relevant financial affiliations disclosed.
In this modern age of technology and the instant gratification it brings, people have become accustomed to a certain level of expediency. For many of our patients, the old adage “Patience is a virtue” no longer applies. In fact, the largest source of patient dissatisfaction is the time spent waiting for an appointment.1,2 One study found that 75 percent of patients who waited less than 10 minutes gave an excellent or good rating compared with 3 percent of patients who waited longer than 20 minutes.3 Another study, using surveys from 44 ambulatory clinics over the course of one year, found that every aspect of the patient experience, including the patient's confidence in the care provider and perceived quality of care, correlated negatively with longer wait times.1
At our site, patients used to wait between 10 minutes and 20 minutes before being shown to an exam room, even longer if a medical assistant (MA) was busy performing an electrocardiogram, lab test, or other duties and was not immediately available to take the patient to a room. To address this, we had to find a way to communicate better and work as a team.
Looking for a solution
To find ways to improve wait times in our clinic, we examined the workflow of the patient experience from the time the patient enters the clinic to the time he or she enters the exam room. We looked for factors we could control and then tried multiple potential solutions. For example, new patients must fill out extensive paperwork, and we spend a lot of time verifying their insurance, which can cause delays in rooming. We tried asking patients to arrive 15 minutes earlier than their scheduled appointment to allow time for these tasks, but they often still arrived at their actual appointment time or later. We also tried using alerts in our electronic health record (EHR) that inform us of a patient's status, such as showing us that a patient is ready to be roomed. However, this alert doesn't help if the MA or physician the alert is meant for misses it or is not looking at the patient schedule screen.
Like many practices, ours had logistical problems with communication. The front and back offices are separated, and our MAs are scattered throughout the clinic. Because of this, our MAs were less likely to know when a patient's chart was ready and rooming could begin. In addition, each MA was used to working as a “silo” with a specific provider, rooming that provider's patients, working them up, and taking care of them only. Meanwhile, if the front-office staff needed to speak with a physician or MA because a patient was late or there was a problem with the patient's paperwork or insurance verification, the staff member had to call or even leave his or her area to track down the physician or MA. This introduced another layer of delay, especially if there were many patients waiting in line to be checked-in.
We realized we needed a solution that would address our communication problem and help us work better as a team. Our solution was to use instant messaging.
How it works
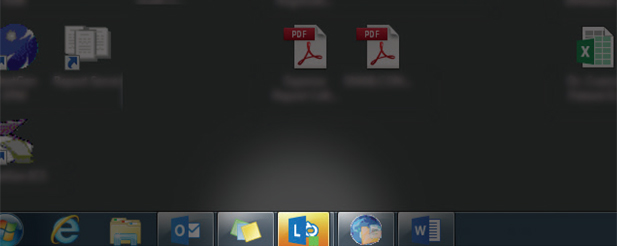
A number of instant messaging applications are available for offices. We use Microsoft Lync, a computer application that is included in the 2013 Microsoft Office Suite our organization uses. We created a group in Lync that includes all staff and physicians so that we would be able to communicate with each other in real time.
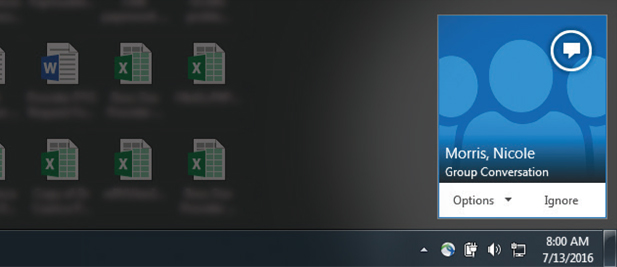
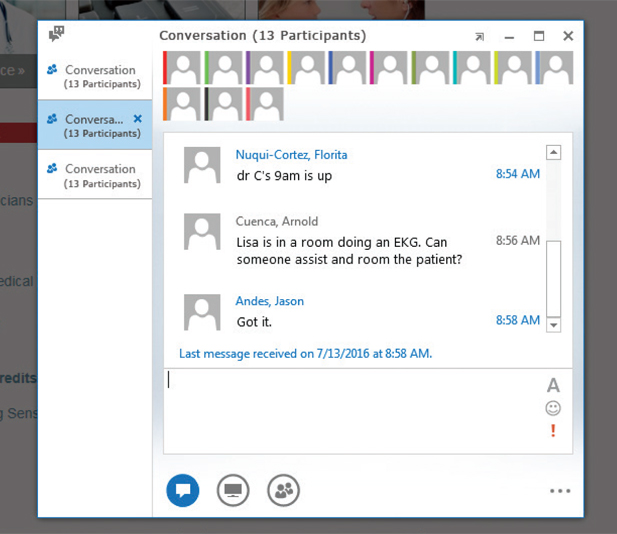
This is how it works: When a patient's chart is available and the patient is ready to be roomed, the front-office staff sends an instant message (IM) to the group. Everyone – all MAs, physician assistants (PAs), and physicians in our four-provider office – is included in the group message because we believe it is important for the entire team to be able to provide backup. The IM generates both a visual cue on our computers and an audio sound, decreasing the chance that staff will miss the message that a patient is ready. (See Figure 1.) These cues activate on the computer screen even if the recipient is working in a different section of the EHR and not looking at the schedule screen showing that the patient has arrived. (See Figure 2 and Figure 3.)
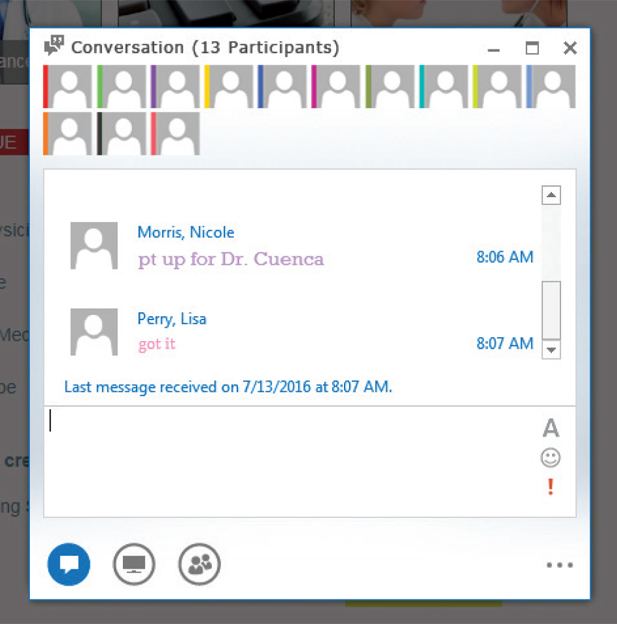
If the MA who is responsible for rooming that patient does not respond to the IM within five minutes, then we have set a requirement that another MA who is available must respond to the IM and room the patient. There must be a response from the back office to the front desk to ensure the communication loop is closed. (See Figure 4.)
Having everyone connected helps us make adjustments quickly and easily. If a patient is late, there is a scheduling problem, or a staff member has a question about a patient's insurance verification or paperwork, the front-office staff can send an IM to the back-office staff and providers asking for help without having to track them down. If a physician is running behind, the back-office staff can quickly send an IM to the front-office staff, who can then inform patients about the delay. This allows staff to focus on the patient experience. In addition, our practice manager can use the IMs to monitor patient flow and redirect staff to address problems if necessary.
The IM system allows us to room patients in less than five minutes. MAs have moved outside of their silos to work together as a team, assisting each other not only with rooming patients but also with performing in-office procedures. This has resulted in an increased sense of camaraderie in the office.
Things to keep in mind
If you choose to use an IM system to assist with your office workflow, make sure you comply with HIPAA (Health Insurance Portability and Accountability Act). For instance, we don't use patient names in our IMs (we say, “Dr. C's 9 a.m. is ready” instead of “John Smith is ready for Dr. C”), and our program operates on encrypted HIPAA-compliant servers configured with security parameters.
Also make sure IMs fit in with your office culture. Although the Lync application is compatible with mobile devices, such as cell phones or tablets, we only use it with our desktop computers. We are concerned that if patients were to see staff trading messages on their cell phones, that could be a distraction. Also, we do not permit staff to use their mobile devices during work hours to avoid reducing office productivity and patient care delivery.
The frequent posting and pinging of IMs could also become a distraction in larger practices. In our four-provider practice, the distraction is manageable, but larger practices might consider sending their IMs to smaller groups of staff based on care teams of two or three physicians and a few PAs or MAs rather than one group including everyone. This limits IMs to the people who truly need to see them.
By improving team communication with the use of a real-time messaging system, we were able to take a significant amount of control over patient delays. With this system in place, we continue to move forward in other areas of practice management to deliver efficient and high-quality care. We hope that other practices consider integrating an IM system into their practices.