
Assembling a dedicated QI team is only half the challenge. Here's how to build and sustain their momentum.
Fam Pract Manag. 2018;25(5):23-26
Author disclosures: no relevant financial affiliations disclosed.

Primary care practices have been tasked with reporting an increasing amount of quality data to satisfy requirements for insurance companies, accountable care organizations (ACOs), patient-centered medical home (PCMH) recognition, and various pay-for-performance programs. As a result, it is common for practices to have ongoing quality improvement (QI) mechanisms in place, with QI teams regularly creating new clinical or operational processes to meet the ever-changing requirements.
Having an established QI process can be a huge advantage to practices. However, sustaining the effort is a challenge. Given that the requirements of practice change and metrics reporting are unlikely to decrease in the foreseeable future, motivating QI teams for continued success is the next hurdle. We have learned some important lessons that we hope will help others keep their QI teams motivated.
1. STRENGTHEN RELATIONSHIPS
Like many practices with competing priorities, we realized we needed to affirm our relationships with one another. Our practice of 35 faculty physicians, 15 residents, and 20 staff had split into clusters of people who knew very little about each other. To build camaraderie, leadership devoted five to 10 minutes of each QI meeting inviting team members to share a small fact about themselves. These “icebreakers” helped build a sense of connection between us and an appreciation of each other's talents and ideas.
In smaller practices, where clinicians and staff know each other better, this exercise may be unnecessary. Still, there is value in finding new ways of relating to one another. It is helpful in maintaining interest and committing to a collaborative, long-term, and systematic QI effort.
KEY POINTS
Sustaining a practice's quality improvement (QI) effort is challenging. Motivating team members to stay engaged is critical for continued success.
Include representatives from every area of the practice on the QI team, and proactively manage their schedules to allow time for QI team work.
To combat skepticism within the team, provide concrete examples of how the team's work will contribute to the overall vision and improve patient care.
Knowing when to seek input from others and when to take independent action is essential for QI team productivity.
2. ENSURE THE RIGHT PEOPLE ARE ON THE TEAM
Our team's composition contributes to its longevity. Although our practice has participated in numerous QI initiatives over the past decade, we have struggled to maintain a consistent, committed QI team from one project to the next. Our current team, which is now almost two years old, is made up of representatives from every area of the practice, including clinicians, nurses, medical assistants, front-desk staff, and management. Broad participation has always been our goal because it helps to keep the QI work grounded in the realities of every office role, but achieving it took creating work schedules that provide coverage for QI team members. While attending to these scheduling needs requires ongoing effort and communication with supervisors, it has been well worth the trouble. Our team meets weekly for one hour in a conference room on another floor, which provides separation from the demands of a busy practice.
Attention to team composition and scheduling paid off in one recent QI team meeting as the team was discussing when to administer a form to patients. When the front-desk representative arrived, one team leader exclaimed, “Here comes our expert!” and the front-desk representative quickly offered a simple, practical suggestion with none of the disadvantages of the other proposed ideas.
3. MANAGE SKEPTICISM
Some skepticism should be expected from individuals who have seen QI initiatives fall short of the transformative visions that were promised. We have found it best to address this head on. Early in our current QI initiative, one team member asked, “Are we doing this to jump through hoops for the funder, or are we actually thinking this will change something?” Since a question like this often goes unspoken, we praised the team for its honesty. Then we explained why the project was valuable, using specific examples.
We described the impact the project could have on improving patient care. For example, we illustrated the benefits of easily identifying patients whose blood pressure is out of control and systematically tracking follow-up appointments. We also emphasized the organizational benefits of the project, reminding the team (and ourselves) that we are developing and refining the structure that allows us to implement innumerable changes of our own choosing in the future. Remembering the larger vision reduces skepticism and contributes to team members' enthusiasm for the work we are doing.
4. ADDRESS PASSIVITY
In addition to skepticism, passivity has the potential to threaten a team's effectiveness. This came to our attention when a sub-group was updating the larger QI team on its progress on a workflow change. After outlining alternative proposals, one of the group members said, “I guess ‘the powers that be’ will decide which one they want us to implement.” This reminded us that our staff has been conditioned to defer to physicians in a historically hierarchical medical culture. Despite our efforts to empower QI team members, their belief that they were powerless persisted. We have found that continued encouragement makes a difference. Participating in the change process and seeing the results also demonstrates the power of the QI team.
5. ENCOURAGE INITIATIVE AND VETTING
Balancing the need for independent action with the need for vetting has been a learning process for the team. Some lessons have come the hard way. For example, a sub-group of our team spent weeks perfecting workflow diagrams of a proposed change. When the group finally shared its meticulous products with the full QI team, it discovered an error in its assumptions and realized a particular solution was not possible. When the revised proposal was vetted, one of the team members expressed caution about moving forward without first ensuring everyone had had a chance to give input. Alternating sub-group working meetings with full QI team meetings is one way to balance the need for independent or small-group work with the need for discussion and buy-in from the larger group.
6. GIVE REAL RESPONSIBILITY
We were pleasantly surprised to find that the more responsibility we gave to team members, the more motivated they became. While it's important not to over-burden team members, they became more engaged and effective when we gave them responsibility for moving projects forward.
This was apparent during an office-wide meeting to share the QI team's work a few months into a new initiative. We had been developing three new workflows simultaneously. Sub-groups of three to four team members were each tasked with presenting their proposed workflow and fielding questions during the meeting. These groups, which included residents, staff, and faculty, developed visual materials and organized effective presentations. There was a palpable increase in enthusiasm after that meeting.
7. SEEK INPUT FROM NON-TEAM MEMBERS
In addition to vetting ideas within the QI team, we emphasized the need to seek input from those outside the team who would be most affected by proposed workflow changes. Team members have consistently followed this advice. For example, while brainstorming about a protocol for dementia screening, one team member mentioned that two doctors see the majority of the group's patients with dementia and suggested we ask them what would work best. “If it doesn't work for them, the whole thing is useless,” a team member said. The team selected a screening tool based on their feedback, but after consulting with the home visits team, learned it was too complex for many home-bound patients. With this input, the group reworked its proposal to include a simpler tool that better fit the workflow.
Because many changes affect everyone in the office in some way, we developed strategies to elicit feedback from the entire office. For example, in addition to gathering input about proposed workflow changes at an office-wide meeting, we created simple posters that outlined each proposed workflow. Each poster was displayed in the lunchroom next to a blank page and pen with a note soliciting input (anonymously, if desired). After two weeks, team members gathered all written and verbal input and considered it in subsequent team meetings.
8. COMMUNICATE, COMMUNICATE, COMMUNICATE
Keeping the entire practice informed and involved in the QI team's work is important for the well-being and productivity of the QI team. Individuals who are not sufficiently informed about the QI team's work may inadvertently and unknowingly become obstructionists to the QI process. For example, one of our supervisors didn't realize a team member had been asked to move a QI project forward and insisted on giving her additional assignments. Confusion and pressure grew to the point that the team member considered leaving the QI team even though she enjoyed participating. We were unaware of the issue until the team member reported the conflict. Keeping the QI process in the forefront of everyone's mind requires an ongoing effort. We continue finding new ways to improve communication, including a weekly review with office leadership and a monthly newsletter for staff, faculty, and project stakeholders. We distribute individual clinical quality metric reports to each faculty member, resident, and fellow, and we post overall quality metric scores in the lunchroom for the entire office.
In smaller practices, keeping everyone informed and at least peripherally involved in the improvement process is simpler. That does not, however, negate the importance of designating a formal, structured meeting time specifically for QI work. Asking for volunteers to record meeting minutes and keep time can help facilitate follow-up and communication with staff and patients.
9. MONITOR THE PACE OF PROJECTS
Teams can easily get bogged down in the development and implementation of a specific workflow, so it is important to consider whether efforts are proceeding at a reasonable pace. Moving too quickly can result in errors that require revisions and create confusion for the practice and patients. Moving too slowly can make it hard to stay focused on the big picture.
10. FOCUS ON RESULTS
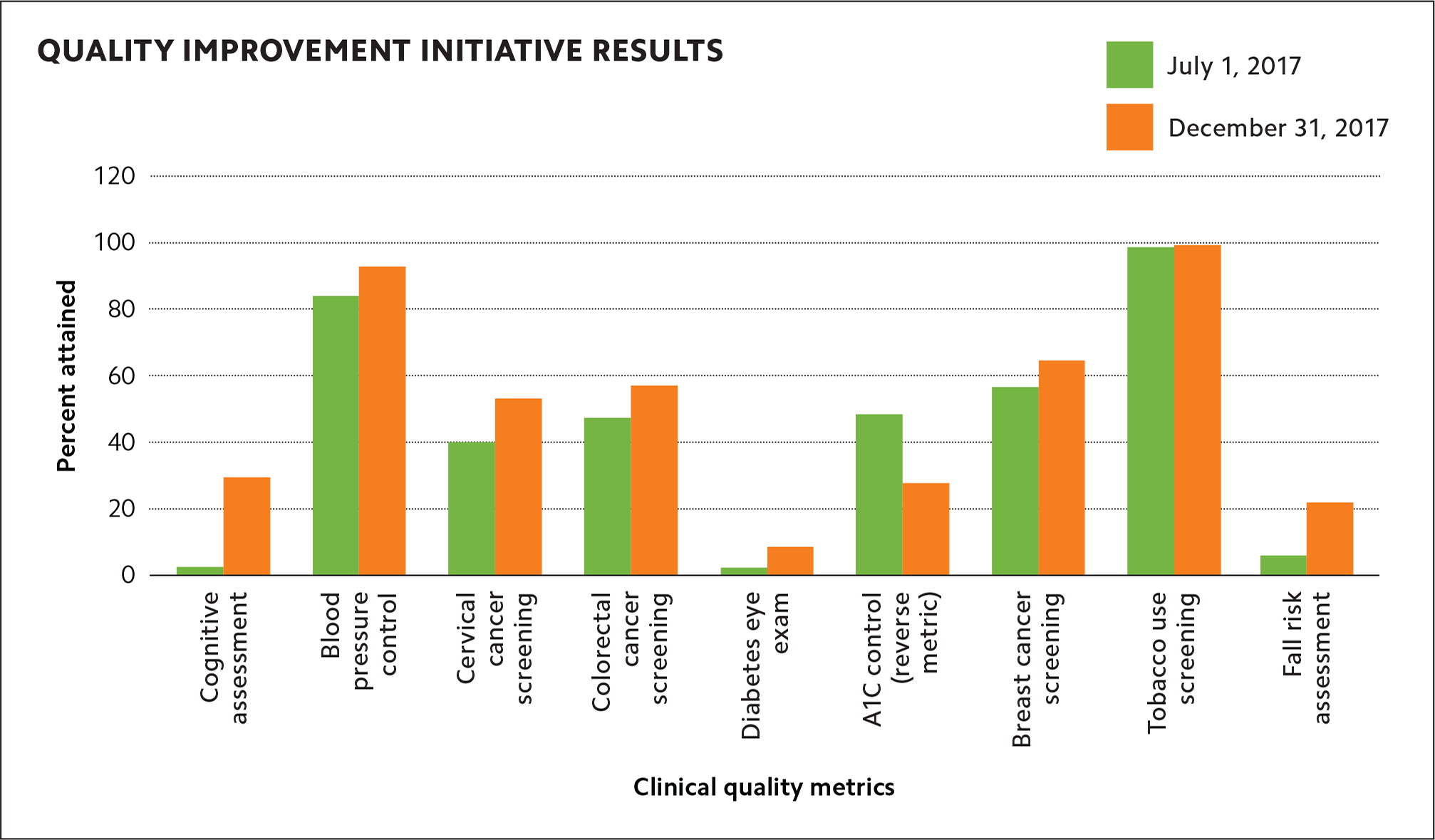
Data-supported feedback can boost morale. After struggling for the first year of our current quality initiative to get accurate and complete data for our areas of focus, the QI team was excited to receive reports that reinforced our successes and reinvigorated our focus on areas where further improvement was needed (see “Quality improvement initiative results”).
A TEST OF ENDURANCE
Several years ago, we were learning to establish QI teams focused on electronic health record adoption, PCMH recognition, ACO participation, and many other factors that influence how we work and get paid. While the demands for change are still extensive, we are much more seasoned today. We are, however, on a new learning curve — maintaining the stamina and motivation necessary for our QI team to continue this marathon. There is no guidebook for this phase yet. We're all writing it together, day by day.
