Adverse childhood experiences can have enduring effects on patients’ health, but these four steps can help promote healing.
Fam Pract Manag. 2019;26(2):5-10
Author disclosures: no relevant financial affiliations disclosed.

“I can’t lose weight! I barely eat, and I keep getting bigger,” says Patient M, a complaint you’ve heard from her for months now, causing both of you to grow frustrated. After being diagnosed with type 2 diabetes a year ago, she has made no progress with her weight loss, and her A1C continues to climb. At today’s visit, you intended to confront her on her poor choices, but when you reviewed her chart briefly before entering the exam room, you noticed her newly completed adverse childhood experiences (ACE) screening was positive for multiple items. So, you take a deep breath, turn away from the computer, look her in the eyes, and say, “That sounds so frustrating. What do you think is going on with your weight?”
ACES: THE HIDDEN ISSUE
ACEs are traumatic events viewed negatively by a child and beyond his or her control. They can have an indelible impact on individuals’ lifelong health, outlook on life, and how they respond to everyday occurrences.
Each year more than one billion children worldwide are exposed to direct or indirect violence.1 In the United States, at least one in four children has experienced child neglect or abuse (physical, emotional, or sexual) at some point in their lives, and one in seven children experienced abuse or neglect in the last year.2 Repeated and chronically negative events suffered by children can be damaging not only to the individuals who experience them but also to future generations and the surrounding community, impacting future violence perpetuation and perpetration, health, and opportunity.3
Fortunately, the experience of childhood trauma does not predestine a person to negative health. Growing evidence suggests that prevention strategies are effective and could improve the lives of those affected while reducing the costs associated with the consequences of childhood trauma.1 Family physicians can play a critical role in the lives of patients, families, and communities by taking the following steps to address childhood trauma.
KEY POINTS
Adverse childhood experiences (ACEs), such as abuse or neglect, can have an indelible impact on individuals’ lifelong health.
Because of the prevalence and impact of trauma, practices should consider adding a 10-question ACE screening tool to their workflow.
Simple shifts in practice can help physicians provide treatment, referral, or emotional support to trauma survivors in a safe, caring, and confidential environment.
1. UNDERSTAND ACES AND THEIR IMPACT ON HEALTH
The Centers for Disease Control and Prevention (CDC)-Kaiser Permanente Adverse Childhood Experiences (ACE) Study, the foundational study about the association between childhood abuse and neglect and later-life health and well-being, was conducted from 1995 to 1997 in southern California.4 It showed that ACEs not only are common but often occur in multitude. More than half of study participants had experienced at least one ACE, one-fourth had experienced two or more ACEs, and 13 percent had suffered three or more. In this initial study, ACEs included child abuse (physical, sexual, or emotional), child neglect (physical or emotional), and household dysfunction (intimate partner violence, substance abuse within the household, mental illness of a household member, criminal activity at home, parental separation, divorce, or incarceration of a household member). More recent ACE scoring systems have taken into account issues such as neighborhood safety, bullying, witnessing violence, racism, and foster care.5
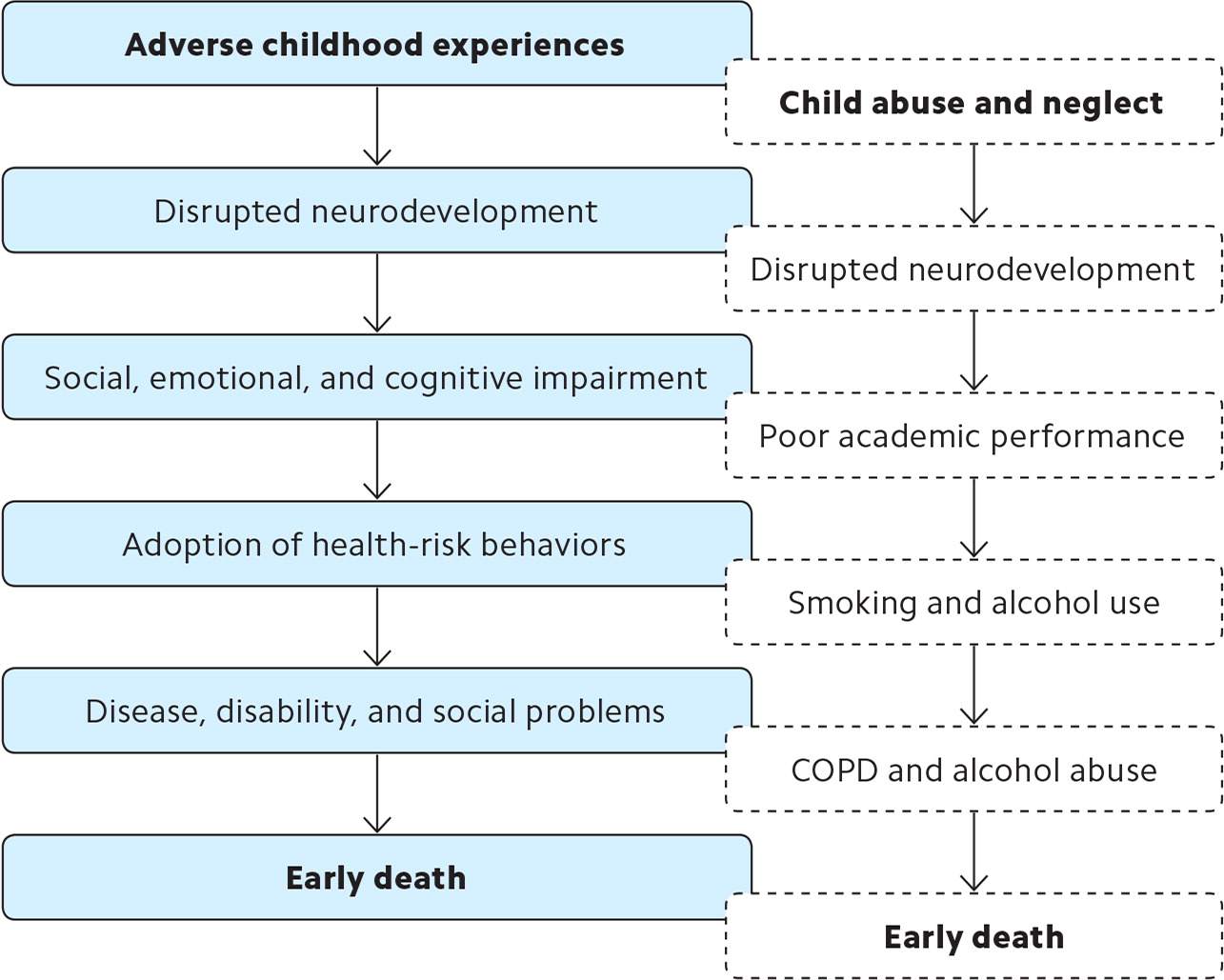
The ACE study demonstrated that as the number of adverse experiences increased during an individual’s childhood, the number of health risk factors for leading causes of death increased as well. Similarly, the study showed that the more ACEs an individual experienced, the higher the likelihood of having certain diseases such as diabetes, ischemic heart disease, chronic obstructive pulmonary disease (COPD), cancer, skeletal fractures, and liver disease. (See “Outcomes associated with adverse childhood experiences.”) Felitti et al proposed a mechanism for how ACEs lead to early death.4 (See “Adverse childhood experiences mechanism with example.”)
| • Alcoholism and alcohol abuse | • Suicide attempts |
| • Depression | • Cancer |
| • Drug use | • COPD |
| • Multiple sexual partners | • Diabetes |
| • Physical inactivity | • Ischemic heart disease |
| • Severe obesity | • Liver disease |
| • Sexually transmitted diseases | • Poor self-rated health |
| • Smoking | • Skeletal fractures |
2. SCREEN FOR ACES
Given the prevalence of ACEs in the general population, it is safe to assume that family physicians commonly care for survivors of trauma. However, we may not always recognize the signs and symptoms of trauma, and our social histories may be inadequate at identifying this integral piece of a patient’s history. With the significant impact ACEs have on health, it seems appropriate to include ACE screening in our workflows. Challenges arise, of course, as this represents yet another screen and yet another task for the already taxed physician in the context of an office visit. However, researchers have found that a 10-question ACE screening tool used with adult patients at routine office visits not only provided physicians with new information about their patients but also did not significantly lengthen visits.6 The key is to develop a team-based strategy so that ACE screenings and associated follow up are not the sole responsibility of the physician.
There are a number of ACE screening tools available. The “Family Health History” and the “Health Appraisal” questionnaires that were used in the original CDC-Kaiser ACE study are available for free on the CDC website. These questionnaires are quite extensive but include the 10 questions referenced earlier, which are shown in “Patient M’s ACE survey.” A systematic review developed by Academy Health identifies nine ACE screening tools worth consideration. It is important when selecting a tool to understand your patient population and its unique needs and experiences in addition to verifying that the tool has been validated.
Studies have demonstrated that patients with or without significant trauma generally find screening acceptable;7 however, it is critical to understand that no screening should take place unless the physician and his or her office is prepared to deliver the necessary aftercare, whether that means treatment, referral, or emotional support. In addition, family physicians can leverage their network of community partners to ensure patients have access to the support they need.
Back to Patient M: You listen closely as she tells you that she is trying her best. She had cut out fast food lunches, but due to cost and scheduling issues, she has now started skipping lunch. She started an exercise program but quickly fell back into old habits. Most nights she ends the evening feeling exhausted on her couch, and sometimes a snack like cookies or chips is all that makes her feel better. You thank her for sharing and ask her if it would be OK to talk more about her answers on her ACE screening survey. She agrees and reveals that she first started gaining weight as a teenager after being sexually assaulted by a family member. As her weight grew, he lost interest in her and the abuse stopped. Food was at times scarce in her childhood household, and she had limited experience preparing fresh foods since she grew up eating mostly processed foods. Food rewards were a common way of easing stress in her family, and when her mom was depressed she often baked cakes to boost her mood. You begin to understand the issues underlying Patient M’s struggle with her weight and uncontrolled diabetes.
| Abuse | ||
| While you were growing up, during your first 18 years of life, a parent or other adult often or very often: | ||
| Swore at you, insulted you, put you down, or humiliated you, OR acted in a way that made you afraid that you might be physically hurt. | ✖Yes | No |
| Pushed, grabbed, slapped, or threw something at you, OR ever hit you so hard that you had marks or were injured. | Yes | ✖No |
| Touched or fondled you or had you touch their body in a sexual way, OR attempted or actually had oral, anal, or vaginal intercourse with you. | ✖Yes | No |
| Neglect | ||
| While you were growing up, during your first 18 years of life, you often or very often felt that: | ||
| No one in your family loved you or thought you were important or special, OR your family didn’t look out for each other, feel close to each other, or support each other. | Yes | ✖No |
| You didn’t have enough to eat, had to wear dirty clothes, and had no one to protect you, OR your parents were too drunk or high to take care of you or take you to the doctor if you needed it. | ✖Yes | No |
| Household dysfunction | ||
| While you were growing up, during your first 18 years of life: | ||
| Your parents were ever separated or divorced. | Yes | ✖No |
| Your mother or stepmother often or very often was pushed, grabbed, slapped, or had something thrown at her, OR sometimes, often, or very often was kicked, bitten, hit with a fist, or hit with something hard, OR was very repeatedly hit for at least a few minutes or threatened with a gun or knife. | Yes | ✖No |
| You lived with someone who was a problem drinker or an alcoholic or who used street drugs. | Yes | ✖No |
| A household member was depressed or mentally ill, OR a household member attempted suicide. | ✖Yes | No |
| A household member went to prison. | Yes | ✖No |
| Total ACE score | 4 | |
3. BUILD A SUPPORTIVE PRACTICE ENVIRONMENT
While prevention combined with early detection and intervention can potentially lessen the lifelong impact of ACEs on health and wellness, practices need to be thoughtful as they partner with patients to do this work. Implementing a screening questionnaire that uncovers intimate and traumatic experiences can re-traumatize the patient if the interaction is mismanaged. Practices must be prepared to emotionally support the patient and family and provide access for those needing additional care. Because some patients may feel more comfortable sharing sensitive information with non-physician staff, it is essential to provide everyone in the office with the skills necessary to assist with these interactions.
The Substance Abuse and Mental Health Services Administration (SAMHSA) defines four critical aspects of providing trauma-informed care:8
Realize that trauma has a widespread impact on individuals, families, groups, organizations, and communities and understand the paths to recovery;
Recognize the signs and symptoms of trauma in clients, staff, and others in the system;
Integrate trauma knowledge into policies, programs, and practices;
Seek to avoid re-traumatization.
Practices should educate physicians and staff in each of these four areas, perhaps partnering with community organizations such as behavioral health centers, schools, or even law enforcement to assist with the training. Additionally, practices should pursue cultural proficiency, use trauma-sensitive, appropriate language both in conversation and in medical record documentation, and have a list of community resources where patients can receive additional services as needed.9
ACE training should also address the need to avoid stereotyping or making assumptions about patients. Take care to establish a safe environment without judging or demeaning patients and their experiences, and assure patients that any information shared will be kept confidential.
Some simple shifts in practice can signal to patients that your practice is a safe space for them. For example, warn patients prior to asking invasive or upsetting questions, and ask permission before initiating touch. While it is not uncommon for patients to feel discomfort during invasive questioning or intimate exams or procedures, clinicians should be aware when the reaction is heightened or more than expected and should respond with sensitivity and empathy.
One way to build awareness and empathy among staff and physicians is to have them complete an ACE screening questionnaire themselves to gauge their own risk and experiences. Be sure to have mental and social support available for your employees as well, because given the prevalence of ACEs in society, chances are high that someone in your practice will have experienced one or more ACEs.
Finally, remember that not all people who have experienced an ACE will go on to have the negative health outcomes shared in the studies, and not all patients with negative health outcomes necessarily have had an ACE. Continue to treat each patient and family member as individuals.
Back to Patient M: It turns out Patient M had never really considered that her childhood could be affecting her struggles with her weight today. As the two of you consider what goals she would like to tackle before her next visit, you offer her a few suggestions including referrals to a therapist who works with sexual abuse survivors and a peer coach who has a knack for teaching others how to prepare vegetables in healthy and tasty ways. Finally, you brainstorm together some non-food stress-relief options to consider at the end of her busy days to help her unwind.
At her follow-up appointment three months later, she hasn’t lost any weight but for the first time didn’t gain any either. She saw the therapist once, but the co-pays were a challenge. Luckily, she has found a supportive network in a peer group for women with prior history of sexual abuse at the local YWCA. Most importantly, for the first time in more than a year, she says she feels like she is on the right track.
4. HAVE A COMMUNITY AND PUBLIC HEALTH PERSPECTIVE
Although trauma is an individual experience, it can stem from community problems and have lasting effects on neighborhoods, families, and schools. As leaders in the community, family physicians can use their knowledge and skills to help address the root causes of trauma and promote healthier communities. Family physicians need not serve as the “local expert” on this topic, but they can challenge any community organizations they are involved with (school boards, local government, zoning commissions, etc.) to consider their role in addressing the issue of childhood trauma. This includes understanding not only the current realities of the community served but also its history and practices that may have placed trauma on the community, such as redlining and displacement from gentrification. This is critical in addressing current as well as avoiding further health inequities within populations.
Practices do not need to reinvent the wheel. Look for organizations whose efforts you can support.10 For example, in our North Philadelphia neighborhood, homicide is the leading cause of death among individuals ages 15 to 19. To help address this public health crisis, Temple School of Medicine has partnered with Philadelphia CeaseFire – CureViolence, which focuses on youth outreach, criminal justice participation, building community awareness about gun violence, and getting residents as well as community, business, and faith-based leaders to work together and get involved. Temple provides funding, technical support, and volunteers, and CeaseFire serves as a valuable resource for high-risk patients.
BREAKING THE CYCLE
Childhood trauma can have a lasting impact on health and well-being. Family physicians have a unique opportunity to affect individual and population health on a significant level by understanding ACEs, screening for them, and using empathy, support, and action to facilitate health and disrupt the cycles of trauma.