
With a little training, nurses can wrap up the patient visit, reducing errors, improving patient satisfaction, and freeing up time for providers.
Fam Pract Manag. 2019;26(4):13-17
Author disclosures: no relevant financial affiliations disclosed.

Traditional office-based processes are broken. While other industries have embraced working in teams, medicine continues to largely encourage clinicians to function as individuals. Individual efforts, lacking standardization, are prone to variable results. Meanwhile, dated medical office workflows do not leverage newly available skillsets and technology. This can diminish efficiency.
Our practice developed the “nurse closer” model as a response. This model systematically drives quality by combining team-based care with technological advances and encourages all team members to work to the top of their licenses. The goal is to achieve higher value care without increasing practice expense or provider burnout. In the time since we implemented this change, we have reached that goal and even increased revenue.
KEY POINTS
Unempowered staff and outdated office practices contribute to inefficiency and provider burnout.
Having a trained nurse or other staff member handle documentation and order entry at the end of patient visits can increase patient satisfaction and save the physician or other provider time.
A “nurse closer” can also help improve care quality, which can lead to higher revenue from payers.
WHAT THE NURSE CLOSER MODEL LOOKS LIKE IN PRACTICE
Our clinic is a Federally Qualified Health Center (FQHC) that serves approximately 7,000 patients per year through 16,500 visits in a rural setting. One physician and four advanced practice registered nurses serve as clinic providers. Support staff includes four nurses (one registered nurse and three licensed practical nurses), a nursing supervisor, and five full-time certified nursing assistants. Our previous, traditional office-based process included a provider-led office visit followed by patient checkout with front-office staff.
Beginning in October 2017, we implemented the nurse closer model. Each morning begins with a team huddle of the provider, a nurse, and a nursing assistant. The team uses a data filtering system in the electronic health record (EHR) to identify the preventive care needs of that day's patients and create a checklist to be used during their visits. As patients arrive, they check in at the front desk and provide any necessary payment. The team's nursing assistant then rooms each patient and completes the clinical intake process by entering patient data into the EHR. The nursing assistant leaves the exam room, gives a brief synopsis of the patient to the provider, and then rooms the next patient. The provider enters the exam room and performs a normal patient visit.
The nurse closer model then begins as follows: The provider, typically toward the end of the patient visit, contacts the team's nurse to come to the exam room. For more complex patients, the provider may ask the nurse to join earlier, during the initial provider-patient discussion. The provider then introduces the patient to the nurse and recaps the visit to both of them, highlighting clinical concerns and offering recommendations. The nurse, using a laptop and established protocols, acts as a scribe by entering into the EHR the provider's clinical instructions, including new medications or changes to existing medications, laboratory or testing instructions, and any necessary referrals. The provider summarizes the patient's diagnoses and tells the nurse what tests to order, which he or she documents in the EHR using drop-down menus that list diagnostic tests. This portion of the process addresses the patient's acute needs.
The nurse and provider then review the checklist generated during the morning huddle, which includes clinical reminders according to diagnoses, age, and gender, such as vaccinations, cancer screening, or health behaviors. They encourage the patient-specific preventive care recommendations at the end of the visit.
The provider then leaves the exam room, allowing the patient and nurse to build rapport. The nurse enrolls the patient in the patient portal (if he or she isn't already enrolled), refills medications, answers patient questions, provides education, schedules tests, gives immunizations, and schedules the patient for a follow-up visit, completing the checkout process in the exam room. The nurses have protocols for each activity. To enhance patient understanding and address future questions that may arise about their care, the nurse sends any instructions to the patient portal. For patients without portal access, the nurse prints the instructions and hands them to the patient as the visit concludes. Meanwhile, the provider has seen the next patient and is ready for the nurse to close the next visit.
RESULTS OF THE NURSE CLOSER MODEL
As an FQHC, we regularly track and report on 11 quality measures based on the Uniform Data System. Comparing our data from the fiscal quarter prior to implementation (July–September 2017) versus one year later (July–September 2018), we found that 8 of the 11 measures showed improvement, one measure showed no change, and two measures showed a decline between the two periods. (See “Quality measures before and after nurse closer implementation.”)
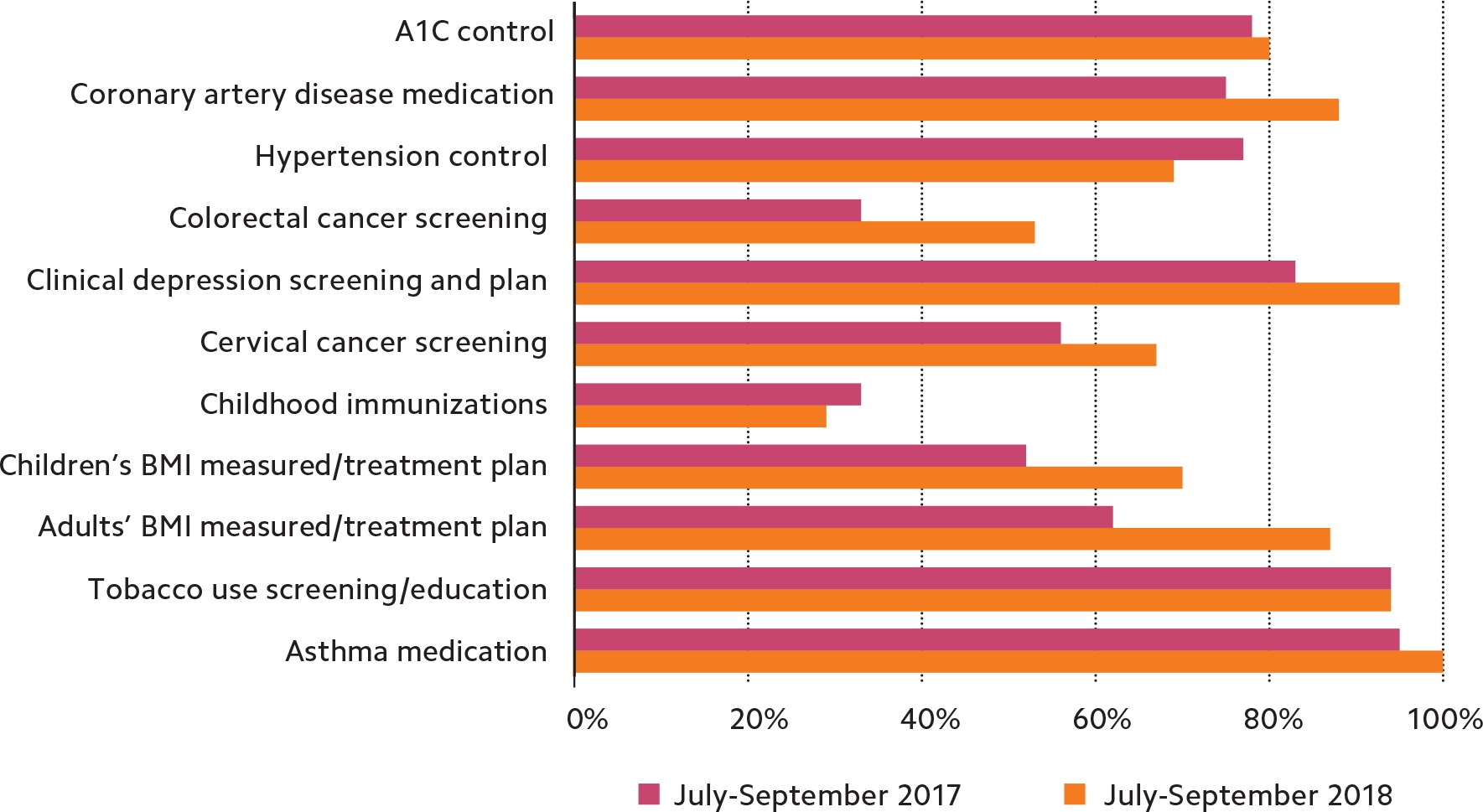
The nurse closer model was originally designed to improve preventive care, specifically colorectal and cervical cancer screening rates, so we were not surprised that these rates showed significant improvement. For hypertension control, which declined, we established new clinical follow-up parameters to address the problem more aggressively. During the subsequent quarter, the hypertension control rate rose from 69 percent to 77 percent. We did not make any immediate changes in childhood immunizations, another area of decline, partly because local pediatricians see the majority of young children in the area and our measure represented a sample size of just seven patients. However, we are working with our state's vaccine database to improve this measure. Quality measurements overall remained steady in the subsequent quarter.
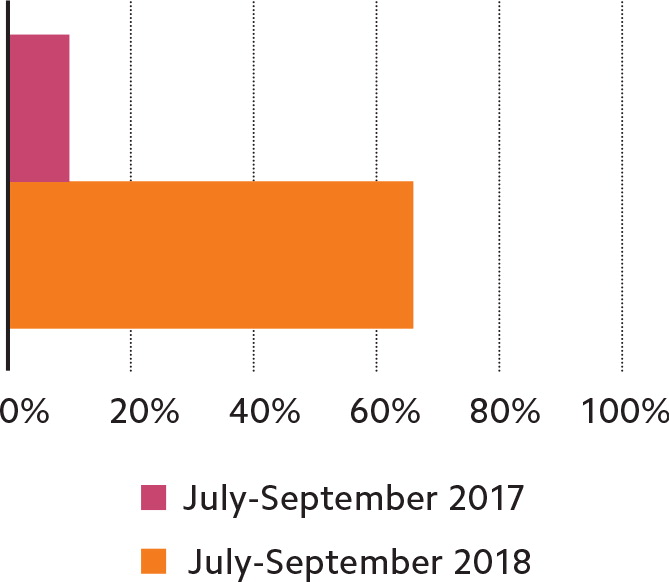
The nurse closer model also increased patient use of the online portal. (See “Patient portal usage.”) Only 10 percent of patients used the portal before we implemented the new process. Afterward, two-thirds of patients used it.
In addition, our nurses reported markedly improved morale under the new process, which led to a lack of turnover in the practice. The nurses, some of whom likened their role under the traditional process to a “glorified receptionist,” said they enjoyed being part of the care team, being able to independently answer patient questions, and having face-to-face contact with patients.
One final result of switching to the nurse closer model was that the clinic's charges increased 31 percent year over year as the clinic moved from a “walk-in” mentality to one where we were more able to address ongoing adult wellness issues, such as cancer prevention, smoking cessation, or weight loss. The nurse closers helped us structure visits so we could address the patients' acute, chronic, and preventive needs more effectively and efficiently. As patients received more education about their health, they were more engaged and willing to schedule future visits to address these issues. The improved quality also led to increased reimbursement from the largest commercial insurer in the state, which adds a certain percentage of reimbursement to the base payments if practices achieve certain levels of quality.
Implementing the nurse closer model didn't require us to change provider schedules or appointment times or hire additional staff. It also improved patient satisfaction. In fact, because of positive word of mouth and a steady influx of new patients, our clinic is now planning to add an additional nurse practitioner and nurse closer to the existing team of providers.
KEYS TO MAKING IT WORK
Our use of the nurse closer model demonstrates that ambulatory care offices can retool their processes to achieve higher quality care that is financially feasible and beneficial to providers. But can this model, developed by an FQHC, work in other practice settings? The answer is yes. Staffing models may need to vary – for example, you could use a certified medical assistant instead of a nurse for the closer – but as long as you provide the necessary training and put protocols in place to ensure safety and consistency you can achieve the same goals. The type of individual you select to staff the closer position is important, but what's more important is the culture of quality you are creating as medicine transitions to value-based care.
Some believe that as value-based care evolves providers will have to do more work and appointments will have to be longer for practices to achieve the desired results. Through our nurse closer process improvement, we have not found this to be the case. However, success does require increased efficiency, which means everyone in the practice must work to the maximum of their licenses. Nurses and nurse aides should not simply be phone attendants and lose the skills they learned in nursing school. They must be an active part of the care team. Providers must realize they alone cannot meet all of the patient's needs in one visit.
To allow nurses to be present as closers during patient visits, we had to reduce the volume of daily phone calls they were answering from patients. This required increasing patient use of the portal. Electronic messaging forces patients to be more concise, increases flexibility of when messages are answered, and ultimately improves practice efficiency. Initially, staff members at all levels were resistant to enrolling patients and encouraging them to use the portal. Staff members perceived that patients did not want to use it. To overcome this resistance (from staff, not patients), we made portal sign-up mandatory. After approximately six months, resistance finally waned as nurses experienced a lower call volume and portal enrollment became a routine part of the checkout process. To maintain the change, all staff members are regularly reminded to encourage patients to use the portal for communication. The nurse closer verifies that patients are enrolled in the portal and, if necessary, gives patients a brief tutorial. Visit instructions are immediately sent to the portal, and nurses prioritize portal communication over routine phone messages, further encouraging portal use. This has the dual purpose of improving communication efficiency while also engaging patients through regular communication with the care team.
We further improved efficiency by having the checkout process in the exam room. Given that billing and payment are already addressed at check-in, once the nurse closer has completed all checklist tasks at the end of the visit, the patient is free to leave. Having nurse closers rather than nonclinical checkout staff schedule tests, labs, and follow-up visits and send patient instructions directly to the portal avoids miscommunication, which decreases errors and patient frustration.
Checklists have become integral to the model, as studies show they improve efficiency and accuracy while reducing medical errors.1 Nurse closers use checklists to ensure they have addressed clinical care guidelines. Making sure this process is standardized among all clinic nurses has resulted in significant overall quality improvements and less variability in quality metrics between providers.
The model also takes aim at reducing the amount of time providers spend documenting and reviewing patient care in the EHR, which has been shown to exacerbate provider burnout.2 The nurse closers use the EHR to generate a checklist of care guidelines near the end of the visit and carry out tasks based on the provider's recommendations. This saves the provider time while ensuring the care guidelines are met. Patients also receive a high-quality visit that touches on wellness and prevention even on busy days.
The nurse closer model also alleviates provider fatigue from having to remember clinical details or check the EHR for details when answering patient questions after the visit. Instead, the nurse who was present during the visit can answer any questions patients later ask either over the phone or through the portal. This also avoids patients having to speak with nurses who were not involved in the visit, which generates frustration for both sides. Nurse closers also use prescription refill protocols, further saving provider time and fatigue while maximizing the nursing skillset.
Quality improvement isn't limited to the patient visits. Nurses and nurse assistants each week receive lists of patients who have yet to complete care items recommended during their visits, such as labs, imaging, or consults. They contact these patients directly to get these items done, which increases quality as well as production. Team members other than the providers frequently discuss other improvements, such as how to schedule patients for preventive care and follow-up appointments to fill all available schedule slots and maximize clinic time. Team members are empowered to care for patients. The nurse closer process has improved morale, which helps limit nurse turnover.3 Making non-provider staff an integral part of the team embodies the team care concept so often talked about but not often employed.
Although it is not part of the nurse closer model, we also implemented a bonus program that awards equal bonus payments to all clinical staff members if the clinic meets quarterly goals for care quality and charges. Provider compensation is typically based at least partly on quality and productivity, but this is not usually the case for nurses. An equal distribution model promotes teamwork and gives the entire medical team ownership in the process.
THE BENEFITS OF TEAMWORK
Consistent quality gains can be achieved through process changes, without additional overall expenses to the practice or providers. The nurse closer model uses EHR-generated checklists for thoroughness and engages patients through the patient portal. Nurses and nurse assistants become an integral part of the care team, driving staff empowerment and engagement and decreasing provider burden. Developing new processes that promote team-based, patient-centered care can improve quality and efficiency and have positive effects on providers and staff.
