
You can’t take care of others optimally unless you first take care of yourself. Start today.
Fam Pract Manag. 2020;27(1):27-32
Author disclosure: no relevant financial affiliations disclosed.

Chris is a family physician who provided the full spectrum of primary care for nearly 20 years. She delivered babies for young mothers she had taken care of since they were teens, covered hospital admissions, and took call in a small group practice. She was also a passionate teacher and leader to medical students, and she contributed to a community-based research collaborative focused on domestic violence prevention.
I worked with Chris for many years and watched her give her all to medicine. When she left her position, she felt angry, isolated, unsupported, anxious, distrusting, guilty, and worthless. These feelings didn’t develop after one bad day at work. They came after years of unrelenting chronic stress, which came like waves continuously crashing on the shore. From the outside, it may have seemed like Chris no longer cared. But she did care. She cared so much and aimed so high that it may have contributed to her fatigue and disengagement.
When Chris left in search of greener pastures, she shared that she had “nothing left to give.” She needed a fresh start. But three years into a new practice, she began having similar thoughts and feelings. The cycle was repeating. Her tank was once again near empty. We stayed in touch, and when one of her family members was diagnosed and soon died of cancer, Chris stopped working. She felt numb, absent from human functions and feelings, dehumanized. Depersonalization is what we often call it.
Chris had spent so many years taking care of so many people that she had no energy left to take care of herself. It had finally caught up with her.
KEY POINTS
Physicians must take care of themselves to have the physical and emotional energy to take care of others.
Saying “no” to perfection, saying “yes” to help from your team, and getting in touch with your emotions are all key to self-care.
To get started with self-care, complete the self SWOT and the Personal Health Improvement Plan.
PRIORITIZING OUR OWN HEALTH
Unfortunately, my colleague’s story isn’t uncommon in health care today. Diminished resources and expanded expectations have contributed to a growing epidemic of burnout among physicians and other health professionals, which has detrimental effects on our practices and our patients.1–4 Medicine, while very rewarding, is extremely demanding, and the culture and environment have been demonstrably toxic to the workforce beginning as early as the first year of medical school.5–7 Evidence-based strategies are emerging to address these factors and to support both personal and system wellness, but more research is needed.8,9
Drs. Sinsky and Bodenheimer have made the case that health care organizations need to pursue the “Quadruple Aim,” which adds the goal of improving the work life of physicians and staff to the “Triple Aim” goals of enhancing patient experience, improving population health, and reducing costs.10 They suggest organizational changes such as team documentation, better workflows, and better training to ease the burden on physicians and staff.
But physicians can’t wait for their organizations to change. In addition to organizational changes, personal changes must take place. Health professionals need to prioritize their own health.11 Individuals modeling wellness and self-care will help foster a culture of well-being in our practices, which will ultimately be better for our patients.
FIVE GUIDING PRINCIPLES
In my work with physicians on personal and system wellness, I have found it helpful to begin with five guiding principles, or “wellisms”:
Say “no” to perfection. Good is good, great is great, but perfect is unnatural and destructive. As physicians, we can struggle with this because we want to be competent and do everything well. We need to remind ourselves that we can do anything, but not everything.
Say “yes” to team. We must not only ask for help but also accept help when offered from our team members (nurses, medical assistants, other providers, students, residents, and even our IT staff). This requires letting go of control, allowing others to thrive, and learning to appreciate help, not resist it.
Embrace emotions. We as humans are designed to experience a full spectrum of feelings. We need to give ourselves permission to be vulnerable and to feel fatigue, sadness, frustration, disappointment, grief, and even joy. Our emotions don’t make us weak; they make us authentic and powerful.
Measure wellness. If we claim to measure what matters, we must add “well-being” to our organizational and individual performance dashboards. Our wellness is critical to our effectiveness not only as physicians but also as teachers, researchers, spouses, parents, etc.
Celebrate self-care. Instead of shaming ourselves or our colleagues for self-care, we should affirm it. Caring for ourselves is not a sign of selfishness, lack of commitment, weakness, or laziness but a means of maximizing our ability to care for others.
TWO TOOLS
So how do we get started on this journey of self-care? Here are two quick but helpful exercises.
1. A self SWOT. A traditional SWOT analysis, often used for organizational planning, involves assessing strengths, weaknesses, opportunities, and threats. A self SWOT can be used to understand our own strengths, weaknesses, opportunities, and threats related to personal well-being. This self-assessment can then guide the creation of a personal wellness plan.
The quadrants of a self SWOT are as follows (see the template):
My strengths — things related to wellness that I have mastered or do very well (e.g., time management),
My weaknesses — things related to wellness that I don’t do well (e.g., regular exercise),
My opportunities — things that could positively affect my wellness if I pursued them (e.g., social support),
My threats — things that could negatively affect my wellness if I don’t attend to them (e.g., a sick family member).
SELF SWOT
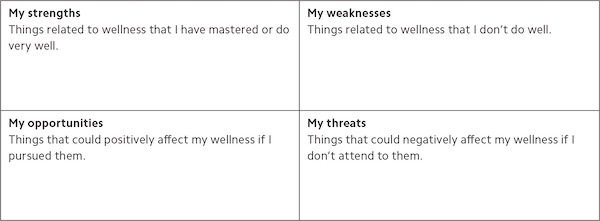
Complete the self SWOT by considering your personal circumstances and placing each of the following practices associated with personal wellness in one of the four quadrants:
Mindfulness — being present in this moment, not judging or multitasking, just observing,
Self-reflection — being a self-learner, silently listening, not speaking or knowing the answer, just asking myself questions,
Resilience — bouncing back after a difficult experience, turning challenges into opportunities, and growing from adversity,
Narrative writing — studying myself, interpreting my experiences by journaling and writing my story,
Exercise and diet — committing to my physical health and well-being, to filling my tank and nourishing my body,
Social relationships — relying on others’ support and mentoring, trusting my team, giving and getting feedback, and not approaching life solo,
Time management — purposefully allotting my time, making choices that replenish me, and not losing hours subconsciously to areas that deplete me,
Cultivating a healthy environment — modeling a culture of well-being, not buying into a status quo of shaming myself or others for self-care,
Embracing change — being adaptive to change, demonstrating emotional intelligence, and embracing my fears versus clinging to what is not working,
Prioritizing purpose — making healthy choices based on my own mission and vision, believing I can do anything, but not needing to do everything,
Cognitive reframing — being flexible in my thinking, rewriting my story, not limiting myself by my thoughts, and not believing everything I think,
Celebration/gratitude — appreciating what is going well in my life, practicing appreciative inquiry, and focusing on the positive people, places, and things that bring me joy versus dwelling on what is not working and expecting more.
(I’ll address each of these wellness practices in more detail in upcoming articles in this series.)
Next, answer the following question: What do you want your future to be like? This is your wellness vision. No need to wordsmith, overthink, or gather consensus. Just answer honestly. For example, “I want to be physically and emotionally healthy so that I have the energy to fully participate in life and enjoy my family, friends, and community.”
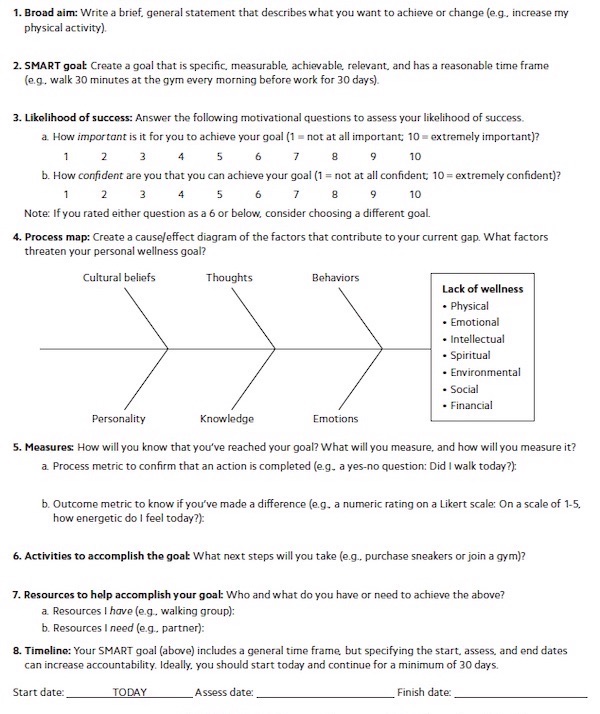
2. A Personal Health Improvement Plan. Analyze your self SWOT and pick one aspect you want to focus on for self-improvement. Make your choice consistent with your vision statement. For example, using the above vision statement, you might choose to focus on things that would increase your energy, such as physical exercise, healthier eating, social connections, or better time management.
Once you have selected an aspect to focus on, complete the Personal Health Improvement Plan worksheet or use the online version to get daily reminders. The worksheet leads you through setting a wellness goal, identifying factors that may threaten your progress, and identifying metrics and steps you will take. Ideally you will start your wellness plan today and continue for at least 30 days. Focusing on one change at a time increases your likelihood of success.
When you’re ready to focus on another aspect of well-being, you can use the SWOT and PHIP tools again. As with all improvement processes, there will be steps forward, backward, and even sideways. Expecting perfection will lead to disappointment, so the goal should not be to become superhuman but to continuously improve.
PERSONAL HEALTH IMPROVEMENT PLAN
THE REST OF THE STORY
After my colleague Chris lost her joy for practicing medicine, she did some self-reflection and realized her need for self-care. She reluctantly accepted an invitation from a persistent friend to go on vacation — an invitation she had previously turned down a dozen times. Chris went to Mexico, her first real vacation in 10 years. Leaving, she felt guilty; returning, she felt replenished. She learned that focusing on herself was good for those around her too. Her challenge now is to change old patterns and to learn to care for herself every day.
The challenge is the same for all of us. We must care for ourselves so that we can care for others, and that challenge starts now.
SERIES OVERVIEW

In this issue:
Creating your personal wellness plan.
In upcoming issues:
Self-care through mindfulness and strategies for promoting physical health.
Family well-being through social connectivity and time management.
Team well-being through conflict resolution and promotion of gratitude in the workplace.
Organizational well-being through prioritizing purpose and creating resilient leaders.
Community well-being through cognitive reframing and building emotional intelligence.
