
With opioid overdoses rising, practices should consider stocking this safe rescue drug alongside other emergency devices and medications.
Fam Pract Manag. 2021;28(1):17-22
Author disclosures: no relevant financial affiliations disclosed.
Imagine you are finishing up a busy clinic session when you hear a cry for help. Rushing out of the exam room, you see a patient collapsed in the hallway. He is lethargic, with slow and irregular breathing. Instinctively, you tell a staff member to call 911 and grab the automated external defibrillator (AED) and CPR bag valve mask. Then you notice a hypodermic needle lying on the floor.
“Get the naloxone in here, stat!” you say.
Would your staff know what to do next?
Opioid overdoses have surpassed motor vehicle crashes as the second-leading cause of preventable death (behind suicides) in the United States, according to the National Safety Council.1 Naloxone, an opioid antagonist, can rapidly reverse the symptoms of opioid overdose and save lives.2 The American Heart Association includes naloxone administration in its basic life support guidelines whenever opioid-associated respiratory or cardiac arrest is suspected.3 In 2018, U.S. Surgeon General Jerome Adams issued an advisory emphasizing the importance of health care professionals having naloxone on hand and being trained in how to use it.4
An overdose inside your medical clinic may not be a common occurrence, but it's still one to be prepared for. This article outlines the evidence for storing naloxone alongside other emergency medicines and devices in primary care clinics, and provides practical advice for practices looking to add it.
KEY POINTS
Given the increasing incidence of opioid overdoses, primary care clinics should stock naloxone alongside other emergency devices and medications.
Naloxone can be administered in several forms. Intramuscular injection with a common vial and syringe is the most affordable form, but nasal sprays and auto-injectors are easier to use, especially for non-medical staff.
Naloxone is a very safe medication but can send patients into immediate withdrawal with severe symptoms. Most patients should be transferred to an Emergency Department after it is administered.
FEW CLEAR GUIDELINES FOR CLINICS
In assessing our large academic primary care clinic (University of California – San Francisco) for overdose preparedness, we found that naloxone was not included in the emergency kit. When we looked for guidance about whether to add it, we were surprised to find few recommendations.
The Joint Commission has no mandates, and the American College of Physicians has not issued official guidelines. The American Academy of Family Physicians supports expanding access to naloxone for patients, medical professionals, and community members, but it does not have an official position on whether primary care clinics should stock it for emergencies. The only definitive recommendation we found came from the American Academy of Pediatrics, which formally recommends that naloxone be stored in pediatric clinics.5
Still, our informal survey of primary care physicians and practice managers revealed significant variation in preparedness for a drug overdose. Many clinics did not carry naloxone at all. Clinics attached to hospitals often relied on an in-house code team to respond to emergencies with “crash carts” stocked with naloxone. But this may cause a significant delay in naloxone administration depending on how large the hospital campus is and how far the code team is from the clinic.
We did identify at least one exception to the overall lack of overdose preparedness: the Veterans Affairs (VA) health system. After an on-campus opioid overdose in the VA Boston Healthcare System, facilities in that region began storing naloxone in their AED cabinets — a policy the VA is evaluating for all its facilities nationwide.9
IS NALOXONE NECESSARY FOR AMBULATORY PRACTICES?
When we began exploring the possibility of storing naloxone in our clinic, we evaluated several questions and concerns:
How likely is a drug overdose to occur in the ambulatory setting? The number of drug overdoses in ambulatory practices in the United States is unknown. Previous articles have identified asthma attacks, anaphylaxis, shock, seizures, hypoglycemia, and cardiac arrest as more common emergencies in primary care clinics.6,7,8 But as overall overdose rates continue to rise, it is likely that overdoses in ambulatory clinics will also increase. Overdose and near-overdose prevalence may vary by clinic location and patient population, but we know that opioid use disorder is common and under-recognized, and it affects people of all ages, races, and socioeconomic groups.10 In addition to patients who use illicit opioids or misuse prescription opioids, patients who take opioids as prescribed are also at risk for overdose, especially if they use opioids with other sedating medications like benzodiazepines.11
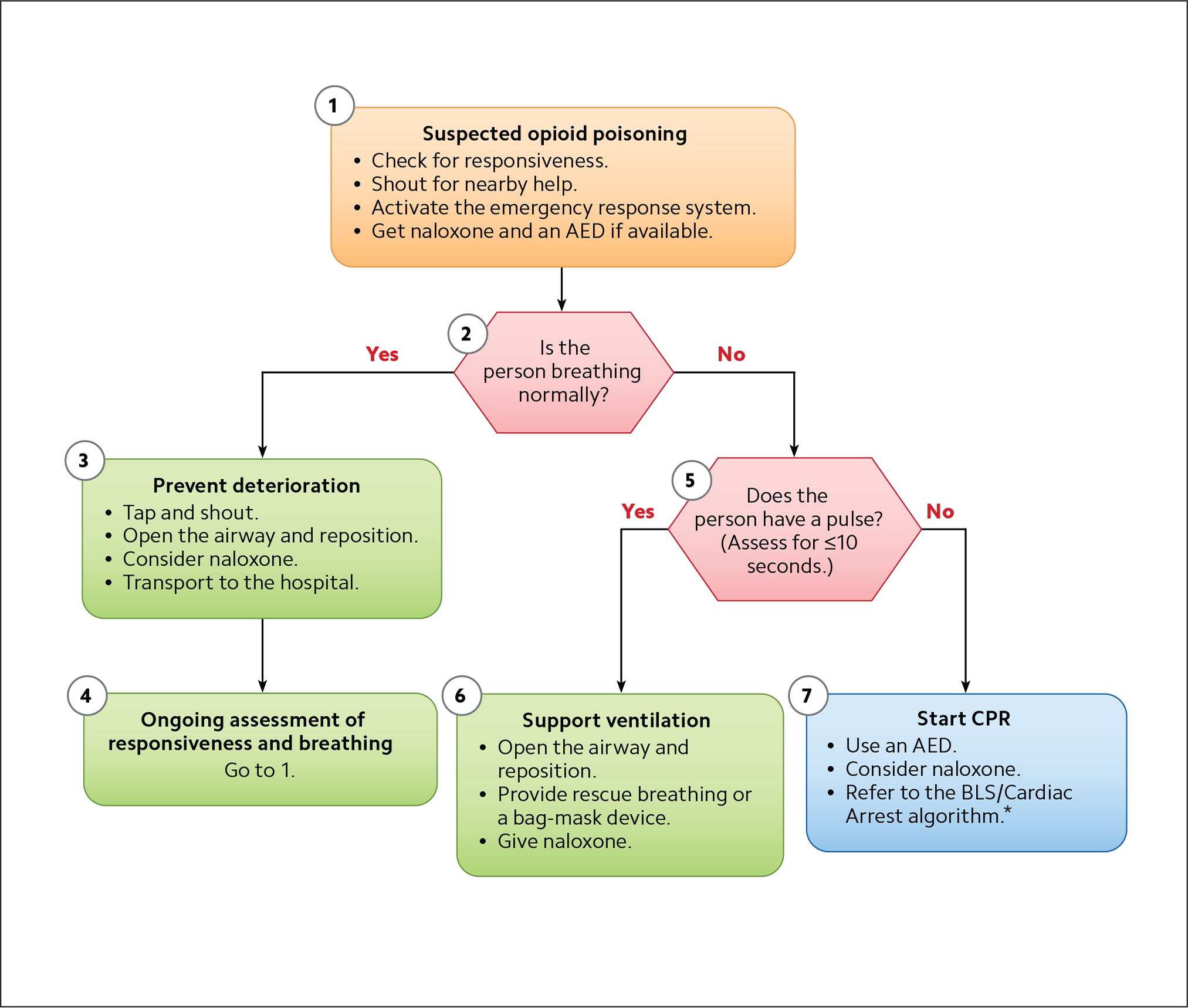
Can't we just provide bag-mask ventilation until emergency medical services arrive with naloxone? Per the American Heart Association, “Bag-mask ventilation is a challenging skill that requires considerable practice for competency.”12 In ambulatory settings where physicians and other providers do not frequently encounter emergency situations, skill levels may vary. Studies have found that a two-handed technique is more likely to achieve an effective seal on the bag-mask valve, but it requires a second rescuer to squeeze the bag.13 There may not be a second person available in an ambulatory care setting in which staff are limited and likely performing other tasks to resuscitate the patient and activate the emergency response system. Some clinics would be forced to use the one-handed technique to seal the mask around the airway, potentially making CPR less effective. Moreover, fentanyl, a potent synthetic opioid contributing to the exponential rise of drug overdoses, is associated with chest wall rigidity, which makes it more difficult to adequately ventilate a patient.14 Naloxone increases chest wall flexibility, potentially making CPR more effective. Lastly, without naloxone, clinics will not be able to provide the standard of care outlined in the American Heart Association's basic life support guidelines.3 (See “Opioid-associated emergency for health care workers algorithm.”) Much as AEDs are now considered crucial for the provision of basic life support, so too is naloxone.
HOW TO INCORPORATE NALOXONE INTO A PRACTICE
Once we addressed the questions about the necessity of naloxone, we set about resolving the details of bringing it into a practice.
What form of the medication should we stock? Naloxone can be delivered as an intramuscular injection via a common syringe, as an intranasal spray, or via auto-injector. Each method has pros and cons. (See “Forms of naloxone.”)
Injectable naloxone is the least expensive, but it requires the most skill to appropriately dose and administer. This is not as much of a barrier in a clinical setting where skilled health care professionals are accustomed to dosing and injecting medications, but the stress of an emergency situation adds an extra complication. Intranasal naloxone is more expensive but easier to use, and it requires very little training. The naloxone auto-injector is also easy to use but is the most expensive of the three forms, according to GoodRx. Some states have programs that offer free naloxone, but eligibility (and the forms of naloxone available) vary by program.15
The shelf life of naloxone also varies by form. The Food and Drug Administration recently extended the approved shelf life of the nasal spray to 36 months, while the other forms remain approved for 24 months.16 In one study, the medication in various forms showed little degradation long after its labeled shelf life, but clinics should still develop protocols for replacing naloxone after it has expired.17 All forms should be stored at room temperature (68 to 77 degrees Fahrenheit).
| Injectable naloxone | Intranasal naloxone | Naloxone autoinjector | |
|---|---|---|---|
| Potency | 0.4 mg/1 mL, 1 mg/1 mL, or 2 mg/0.4 mL | 2 mg/0.1 mL per device or 4 mg/0.1 mL per device | 2 mg/0.4 mL per device |
| Packaging | Single-use syringe system (needle not included); single- and multi-dose vials available | Two active devices per package | Two active devices and one demonstration device per package |
| Initial dosing | Adults: Administer 0.4 mg intramuscularly Children five or younger or who weigh less than 20 kg: Administer 0.1 mg/kg Children older than five or who weigh more than 20 kg: Administer 0.2 mg | Administer one spray into one nostril for all patients, adult or pediatric | Administer one dose to all patients intramuscularly or subcutaneously into the anterolateral thigh, through clothing if necessary, as directed by the voice-prompt system. Pinch thigh muscle while administering to patients under age one. |
| Repeat dosing | Additional doses may be given every 2–3 minutes if respiratory depression persists | Additional doses (alternate nostrils) may be given every 2–3 minutes if respiratory depression persists | Additional doses may be given every 2–3 minutes if respiratory depression persists |
| Cost | About $15–$30 per dose | About $75–$140 per pack (two doses per pack) | About $200–$400 per pack (two active doses per pack) |
| Pros | Lower cost | No assembly required No special disposal Moderate likelihood of proper administration without training | No assembly required Demonstration device included Automated voice prompts High likelihood of proper administration with or without training |
| Cons | Assembly required Fragile glass container Sharps disposal Potential for needlestick | Higher cost | Higher cost Sharps disposal Special disposal may be required by state law due to battery |
How much training is needed? The form of naloxone you choose will determine the amount of training required. An injection syringe requires the most training for lay-persons, but it's a method familiar to most medical professionals. An auto-injector manufacturer's study found that 90% of laypersons could properly administer naloxone via auto-injector with no training and 100% could do it after minimal training from a nurse.18 That outperformed the naloxone nasal spray, which the study found 0% of laypersons could operate successfully without training and only 57% could operate properly with training. But the nasal spray fared much better in a larger study that was not industry-funded (and did not include auto-injectors). In that study about two-thirds of laypersons used it properly even with no training.19 The same study found that about half of untrained people could properly administer naloxone with an intramuscular injection kit.
Given the rapid increase in drug overdose deaths, we recommend that all health care professionals and non-medical clinic staff be trained to recognize and respond to opioid overdoses. Training resources that are brief, affordable (some free), and accessible for a wide variety of learners are available online.20,21 Some basic life support courses also include naloxone administration.
Though everyone should be trained in case someone is away when an emergency happens, individual clinics can still decide who will usually administer naloxone. This decision should be part of an overarching emergency preparedness program that includes designated staff roles, reminders about where emergency supplies are stored, and mock emergency drills with debriefs.6
What are the liability issues? Naloxone is a very safe drug and, to our knowledge, there have been no legal actions against health care professionals for attempting to resuscitate a patient with it. If mistakenly used on a patient who has not used opioids, naloxone has virtually no effects (unless the patient has an allergy to naloxone or other ingredients in the various naloxone forms). If used on a patient who has overdosed, the patient will experience symptoms of opioid withdrawal. These symptoms — including body aches, stomach cramps, nausea, and vomiting — are uncomfortable and can be severe, but they are rarely life-threatening.22 The effect of naloxone is temporary, lasting approximately 30 to 90 minutes. Repeat dosing may be required depending on the potency of the opioids the patient has consumed and the patient's tolerance. Transfer to an Emergency Department for ongoing care should be done in most cases.2 Patients who overdose should also be evaluated for opioid use disorder and buprenorphine treatment.
All 50 states have passed laws increasing public access to naloxone. The laws vary by state but often permit prescribing to third parties, allow naloxone distribution by standing order, grant laypersons immunity from liability when they use naloxone in an emergency, and provide significant protection from civil and criminal liability for clinicians who prescribe naloxone.23 Furthermore, many states allow for behind-the-counter (without a prescription) purchase of the naloxone nasal spray and auto-injectors. Other states allow pharmacist-initiated prescriptions or collaborative practice agreements between pharmacists and prescribers in which the prescriber delegates patient care to the pharmacist.24
Given the widespread knowledge of the opioid epidemic and these efforts to expand the distribution of naloxone in every state, one could argue that not having naloxone on hand is a bigger liability for ambulatory clinics than having it.
We recommend assessing whether your clinic is prepared for an overdose and keeping naloxone in your emergency kit. This is especially important for clinics in rural areas where emergency response times are longer. If you already stock naloxone in your clinic, confirm that all clinicians and staff know how to recognize and respond to an opioid overdose. They are becoming increasingly common, and naloxone should be on hand in case one happens in your clinic.
