
Three overlapping burdens are making it difficult for practices to recover.
Fam Pract Manag. 2022;29(4):37
Author disclosure: no relevant financial relationships.
As a quality officer for a large medical group, I have been trying to understand why we have struggled to rebound from the quality metric decreases that occurred at the start of the COVID-19 pandemic. Our in-person visits have bounced back, but our quality metrics have not. As a primary care physician, I think I finally understand why.
1. The emotional burden. During the height of the pandemic, before vaccines were approved, our practices lost many patients to COVID. They would go to the emergency department, then to the intensive care unit (ICU), get intubated, and never leave. No one could visit them, not even their primary care physician, because of the strict hospital quarantines. I consider myself resilient, but hearing about these patients week after week definitely took a toll. I think one of the worst ways to die would be in the ICU on a ventilator with no outside contact.
Although many of us have tried to distance ourselves from the emotional effects of the pandemic, the burden is heavy — even heavier when we try to carry it alone. In April 2021, one in three primary care physicians said their level of burnout or mental exhaustion had reached all-time highs, according to a survey by the Larry A. Green Center (https://bit.ly/3Njg8Jl).
2. The workload burden. Many primary care practices have been stretched to the limit. In a September 2021 survey, also from the Larry A. Green Center (https://bit.ly/3KYRUST), 74% of primary care physicians said they have experienced turnover in staff, and 44% said they have experienced turnover in clinicians. At the same time, 56% said the health of their patients with previously well-managed chronic conditions had worsened. This is partly due to patients avoiding in-person visits during COVID and falling behind on needed care.
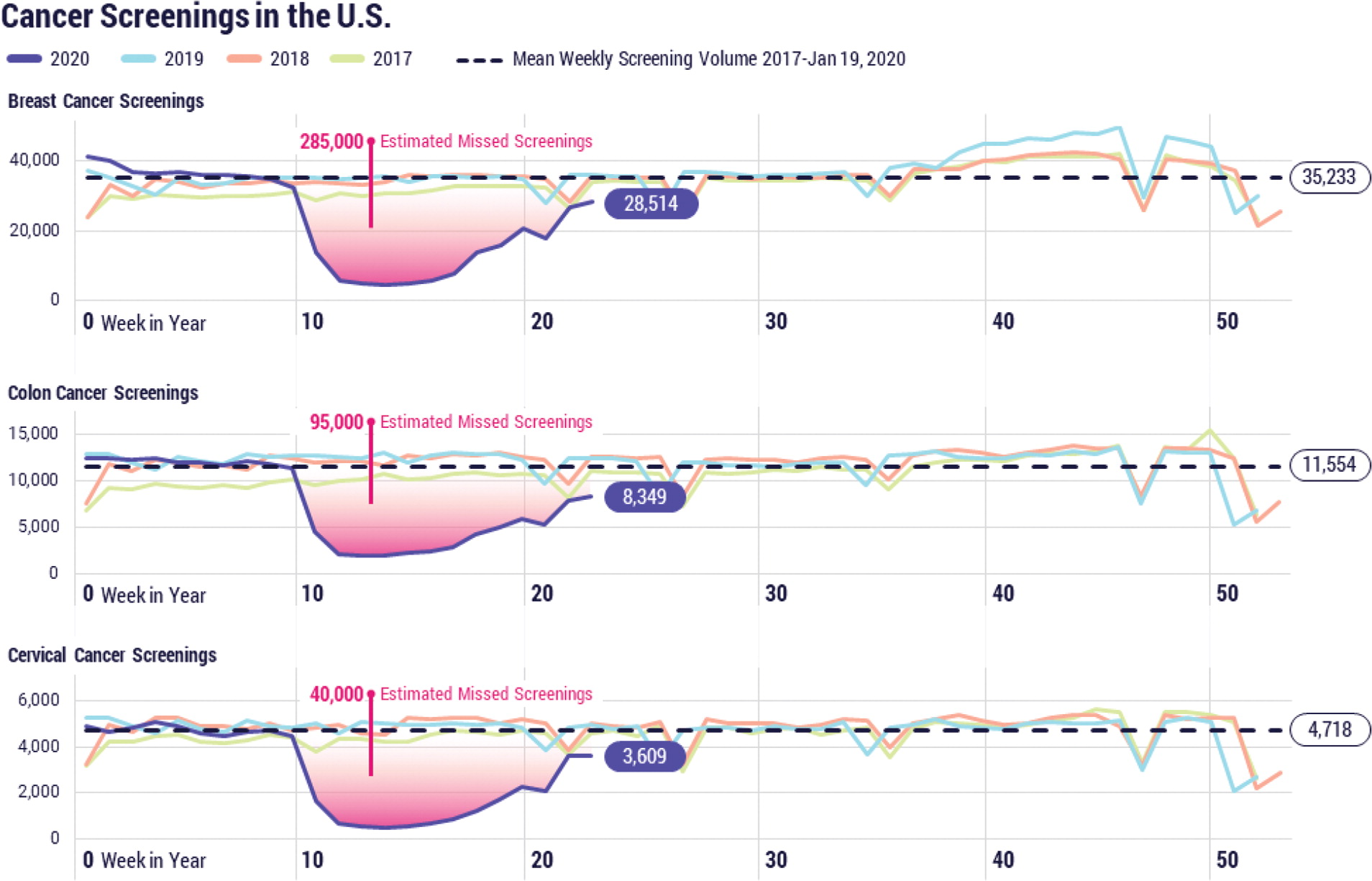
Although in-person visits have resumed, the pent-up demand for primary care has left many practices struggling to catch up. Consider the screenings missed during COVID. According to Cosmos, a dataset of more than 120 million patients in Epic EHR systems across the country, preventive cancer screenings in the U.S. dropped sharply following the declaration of the COVID-19 national health emergency — an 86% decrease for colon cancer screenings and a 94% decrease for breast and cervical cancer screenings.1 Though screening rates have rebounded since the early months of the pandemic, we can only make up for the screenings patients missed if the rate significantly exceeds the baseline. We are not seeing that happen. (See “Missed cancer screenings.”)
Attempts to close care gaps by improving physician efficiency may seem like a good idea, but often they just oil the hamster wheel and increase burnout. Physicians can only go so fast before being thrown out of the wheel — or voluntarily jumping out. No wonder we are seeing retirements increasing and happening at earlier ages than in the past.
3. The payment burden. Across the country, our fee-for-service payment system amplified the effects COVID had on clinicians and contributed to burnout. Many physicians lost income due to the precipitous drop in office visits. To make up for the losses, they have been working harder and adding more patients to the schedule. This faster pace leaves less time to focus on closing care gaps and providing preventive care, with a cascading negative effect on quality metrics.
If the primary payment model during the pandemic had been value-based rather than volume-based, practices could have weathered the storm much better. Up-front, risk-adjusted, per-member-per-month payments, along with quality incentive payments, would have given practices consistent income throughout the pandemic to effectively manage their patient populations. Some screenings would have still been missed during the lockdowns, of course, but value-based payments would have made it easier to provide care outside of office visits, for example, by using digital health tools and care coordinators to reach out to patients with chronic diseases.
COVID alone didn't cause our quality metrics to tank, our workloads to become unmanageable, or our burnout rates to rise. It just accelerated these issues. The underlying problem is that a good portion of our health system is still trapped in the fee-for-service hamster wheel. As we move beyond the pandemic, we have an opportunity to improve the health of our patients and our care teams by reimagining our care delivery model. I hope we take it.
