
Traditional scheduling can set physicians up for failure and frustration. Here’s a better way.
Fam Pract Manag. 2022;29(6):19-24
Author disclosures: no relevant financial relationships.

The way practices schedule patient visits can be a major factor in physician job satisfaction. A well-constructed schedule allows physicians more time for complex patients by reapportioning time left over from more straightforward patients. By scheduling appointments within each hour on a wave (i.e., front loading), practices can balance access and timeliness, improve continuity and financial stability, and reduce frustration and waste.
This article outlines seven steps, starting with wave scheduling, that can set up your practice for success.
KEY POINTS
Scheduling office visits in rigid blocks of time doesn’t account for differences in the complexity of each visit, making it hard for physicians to stay on schedule.
Scheduling “on a wave” (e.g., two patients on the hour and one on the half hour) allows more flexibility to shift time from patients who don’t need it to the ones who do.
Other strategies for staying on schedule include building in a buffer of unscheduled time on certain days, using team-based care, and scheduling follow-up appointments at the conclusion of the current visit.
STEP 1: SCHEDULE ON A WAVE
Scheduling on a wave rather than in a series of rigid time blocks allows practices the flexibility to adjust to patient needs on the fly. It isn’t always clear in advance which patients will require five minutes of a physician’s time and which will require 25 minutes. What is predictable is that some patients will take more time, and some less. It’s also predictable that, despite a practice’s best efforts (phone call reminders, text confirmations, etc.), some patients will fail to show up for their appointments entirely. This is predictable unpredictability, and we can adapt to it if our schedules are flexible.
The traditional method of scheduling patients in a rigid series of consecutive time blocks (i.e., non-overlapping 15-, 20-, or 30-minute appointments) often leaves physicians and staff stressed and frustrated. Practices with that system run behind whenever a patient arrives late or requires more time than allotted. They are also unable to repurpose any time that goes unused when a patient scheduled for, say, 30 minutes requires only 15, or when a patient no-shows.
A certain percentage of patient visits will always go shorter than average, and wave scheduling allows practices to take that time and repurpose it for the percentage of visits that inevitably go longer than average.
Here’s one way to do it: For many family physicians, scheduling two established patients on the hour and one on the half-hour works well. This builds in flexibility. The physician begins with whichever patient staff have ready first. If one of the first patients is late or a no-show, you can use that time on the others.
Even if two patients arrive at the exact same time, they’re unlikely to have to wait more than about 15 minutes. This is where setting patient expectations comes in. Let your patients know that, due to the way you schedule, they might have to wait a short time when they show up for a visit, but they will also have more face-to-face time with you when they really need it.
The specifics of wave scheduling can vary. Preventive care visits often also include evaluation and management of conditions or concerns, so some practices find that it works best to schedule only one or two preventive visits within each hour. The same may be done with new patient visits, which also generally take longer.
You may want to experiment to find what works best for your practice. It can be as simple as double-booking patients at the top of each hour and using the second half of the hour to catch up.1 The key is to break out of scheduling systems that assume each patient will be ready to be seen at precisely the scheduled time and all patients will need to be seen for the same amount of time. Give yourself more flexibility.
STEP 2: USE TWO OR THREE EXAM ROOMS
It is impossible to be efficient working out of a single exam room. Physicians should have at least two, and preferably three if they have a strong staff completing much of the pre-visit and post-visit work.
With two exam rooms, physicians can be seeing one patient while staff are rooming the next patient. With three, physicians can be seeing one patient while staff are rooming the next patient and performing post-visit tasks for the previous patient. Having three exam rooms works especially well for practices that do exercise oximetry and pulmonary function tests, or procedures such as immunizations, endometrial biopsy, suturing lacerations, and joint injections. It allows team members to keep the flow of patients moving, even when using one of the three rooms for these services.
STEP 3: BUILD IN A BUFFER TIME
When scheduling, it is helpful to create a buffer: an hour or so of additional time with no appointments that staff know they can schedule into to meet occasional surges in demand. This could mean starting an hour earlier the next day, seeing patients over the lunch hour, or seeing patients at the end of the schedule.
The practice’s scheduler can regularly check the upcoming week’s schedule to look for warning signs of a busy day, allowing the team to build in more buffer time if necessary. Some days, such as Mondays or the first day back after a vacation, will predictably have more same-day patient scheduling demand than others. It is wise to schedule these days more lightly or anticipate using the buffer times more frequently.
A close-knit team, with medical assistants or nurses routinely sharing their knowledge of patients with the scheduler, will often be able to book at least some same-day patients during normal clinic hours (often on the half-hour time in the wave scheduling template described above), thus conserving the buffer time. Team members can then use that time to respond to inbox messages, return patient phone calls, work on panel management, or other tasks. The physician can use it to focus on indirect care, such as inbox management, attend to team relationships and skill building, or go home a little earlier than usual if the buffer is at the end of the day.
If you find that you are consistently using up your buffer time with patient care, then you may be over-paneled for the resources available (more on that later).
STEP 4: INCORPORATE TEAM-BASED PRACTICE FUNDAMENTALS
Working without a fully staffed team is a significant driver of stress and burnout.2 Some members of the team will predictably be absent for vacation and sick days at any given time. That means that unless your overall staffing is slightly above 100% of daily need, you will be chronically understaffed.
You can plan for staff absences by hiring “float” team members who become familiar with the unit’s routines and can fill in on several roles as needed. When they aren’t needed for direct patient care, float staff can do other work, such as panel management and visit preparation.
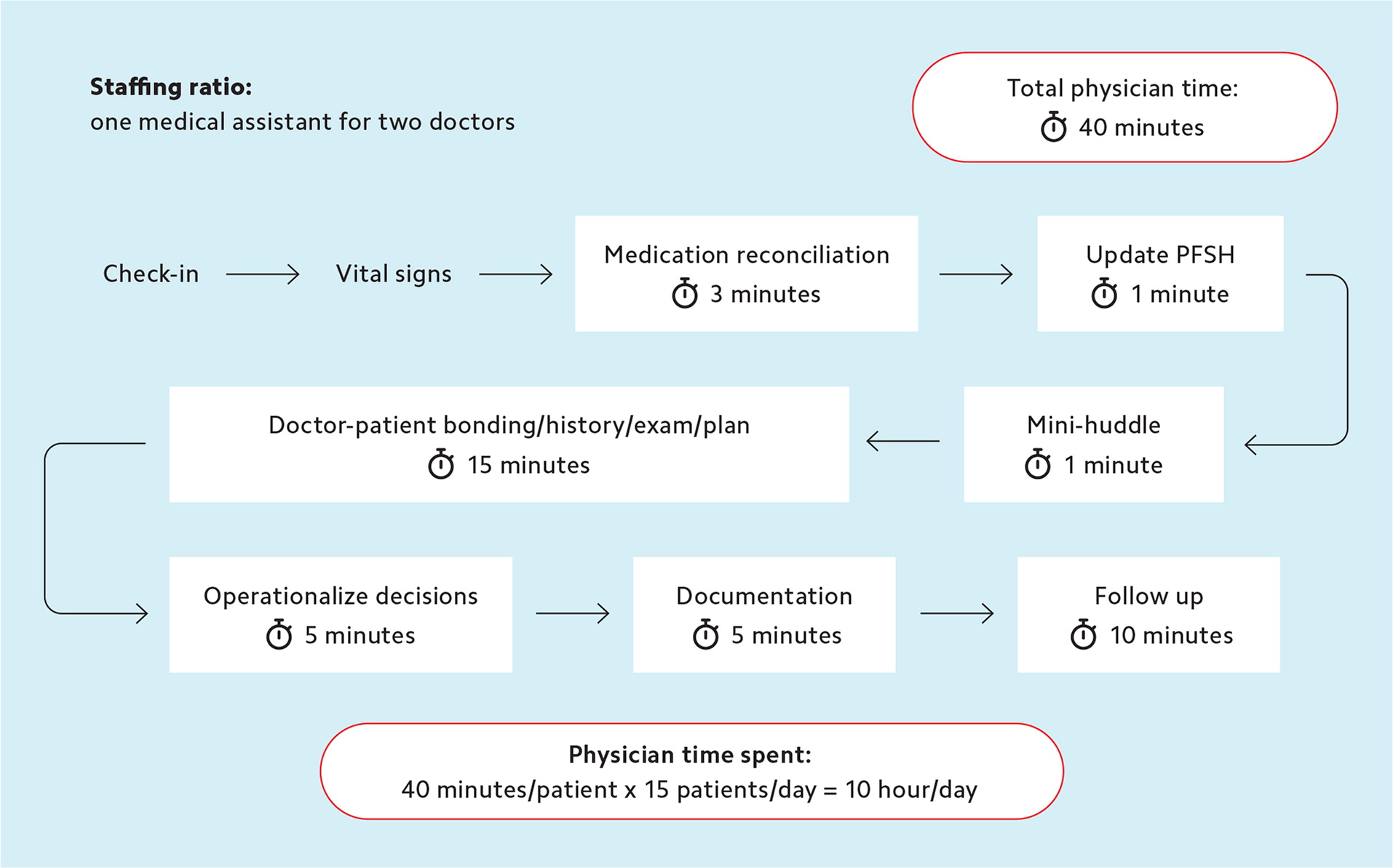
Staffing is only one part of the equation for scheduling success, however. The stability and skill level of your clinical team also influences how much flexibility you can build into your schedule. Even in a “low staffing” model (e.g., one medical assistant for every two doctors), practices can achieve some efficiencies by staggering doctors’ schedules and having the medical assistant handle check-in and vitals. (See “Task distribution in a low staffing model.")
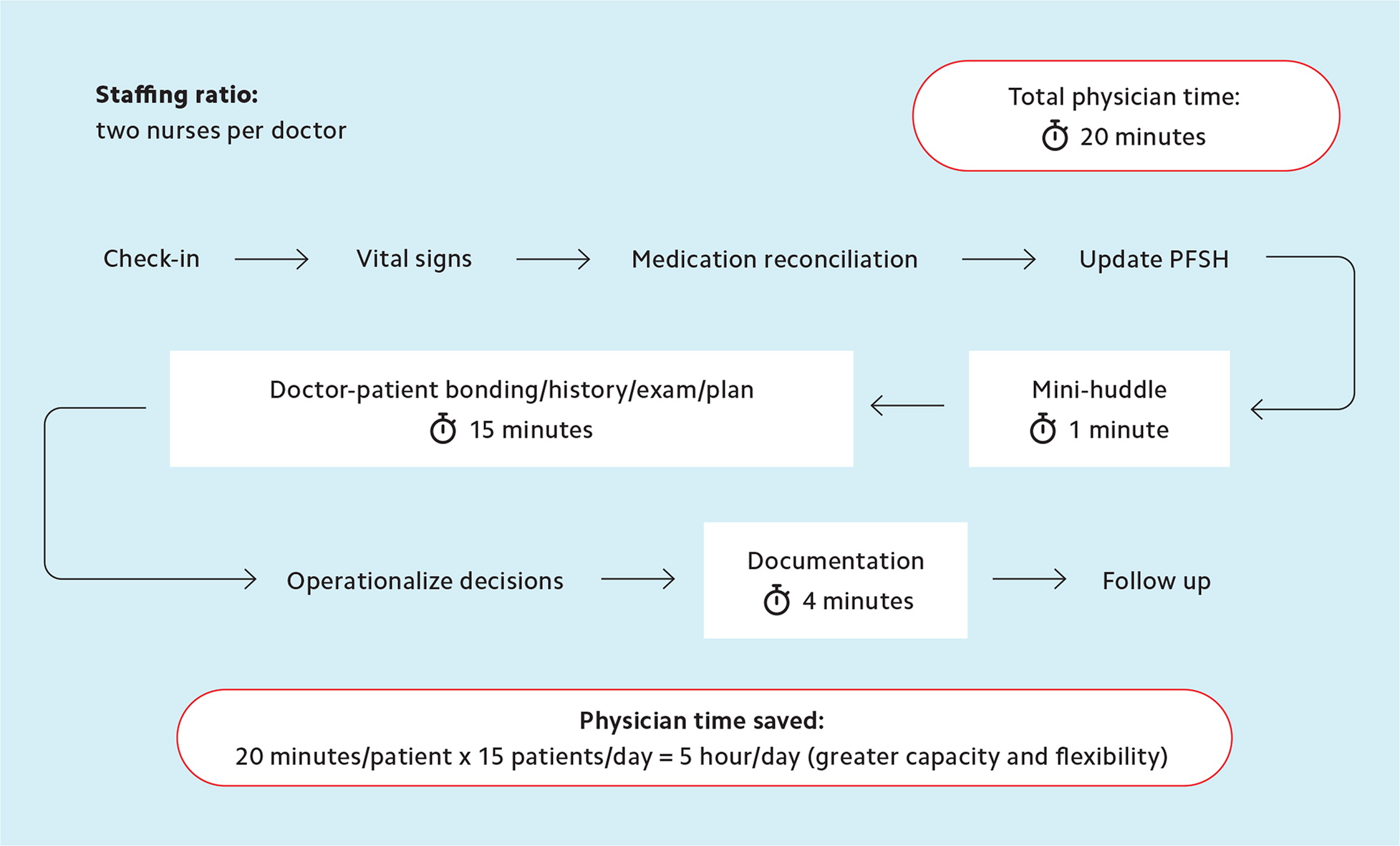
On the other hand, a robustly staffed practice (e.g., two nurses for each doctor) employing advanced team-based care techniques can save physicians even more time for seeing patients. In advanced team-based care,3 staff are empowered to do more of the standardized, predictable “production line” work, allowing physicians to focus only on the work they are uniquely trained to do. This means an appointment that would otherwise require 25 minutes of physician time may only require 10 minutes.4 That allows practices to schedule more patients in a day or provide more same-day appointments. (See “Task distribution in an advanced team-based care model.”)
STEP 5: SCHEDULE FOLLOW-UP VISITS AT THE CONCLUSION OF EACH VISIT
Having a staff member schedule the patient’s next visit at the conclusion of the current visit can also save significant time and keep the practice running smoothly. It’s better than all of the alternatives for scheduling follow ups.
Requiring patients to call to make their next appointment inevitably means some won’t remember to schedule it. When they do remember, there may not be any open appointments for several months, resulting in delayed care and dissatisfied patients.
Placing patients on lists to remind staff to call them to make another appointment isn’t a better option either. It essentially requires scheduling each patient twice: once when the practice puts them on the list (i.e., the “tickler file”) and once when the practice calls and confirms the next visit. Each touch point costs staff time. Scheduling the next appointment at the end of the current appointment eliminates one of these steps.
It also makes patients more likely to keep up with follow-up visits, which promotes continuity and increases adherence to disease prevention and chronic illness monitoring. This will increase your performance on patient satisfaction and quality metrics and reduce the amount of required staff outreach compared to relying solely on a registry to catch all of your patients’ care gaps. A small number of appointments will still require multiple staff “touches” because they will need to be rescheduled as the date of the appointment approaches. But even if 10% of patient visits need to be rescheduled, you have still reduced the staff time for scheduling appointments by almost half.
STEP 6: MAKE A PLAN TO INTEGRATE TELEMEDICINE VISITS
Integrating telemedicine into daily practice has become a necessity in primary care, and there are a couple different ways to do it.
Your practice can intersperse telemedicine visits among in-person visits or schedule them all into dedicated blocks of time on a specific day of the week. Both approaches have pros and cons. Some physicians and teams welcome the variety of a telemedicine visit mixed in between in-person visits, while others like the convenience of doing a series of telemedicine visits from an off-site location, such as at home.
Interspersing telemedicine visits with in-person visits on the same day allows easier integration of team-based principles in the televisit. Doing telemedicine off-site requires sophisticated planning to ensure that tasks support staff usually do — such as medication reconciliation, care gap closure, and orders — aren’t left undone, or left to the physician. Figure out what works best for your practice before making your schedule.
STEP 7: OPEN THE SCHEDULE 13–15 MONTHS IN ADVANCE
To successfully reappoint patients at the conclusion of the current visit, you will need to open your schedule for a little over a year. I recommend 13–15 months because that allows you to reappoint patients who only need a yearly appointment and may not be able to return exactly 12 months after the current visit.
It can be tricky to schedule that far in advance, for yourself and your patients, but it will ultimately save everyone time. You won’t know the exact days that you will take off in the next 15 months, but you probably know roughly how many total vacation, meeting, and personal days are available to you. Block off this number of days somewhere in your schedule where you anticipate potentially taking them. It is much less work to reschedule a few of these weeks when your schedule is known than to have to schedule them all twice because every patient was first “scheduled” onto a tickler file list.
Scheduling 13–15 months in advance is also respectful to patients because it gives them a reserved slot ahead of time that they can plan around. Automated texts, phone calls, or emails allow practices to remind patients of these appointments as they approach, reducing no-shows without requiring any extra work for staff. Another tip is to track which patients fail to show up for scheduled pre-visit labs. Practice staff can then reach out to those patients and ask if they are planning to keep their appointment.
SOME FINAL “PRACTICE PEARLS”
Here are some additional tips to make scheduling go more smoothly and efficiently.
Map out and optimize your current workflow. In most primary care practices, for every hour of patient-scheduled time, physicians spend at least an hour on other related tasks.5 It doesn’t have to be this way! Map out the steps of a visit, measure the time for each step, identify the person who performs it, and ask whether this is the right person to do this task. If not, restructure your workflow so the physician is doing fewer tasks that staff could do.
Link prescription renewal and testing to each patient’s annual wellness visit. Prescribing medications for patients with stable chronic illnesses for 90 days plus four refills removes much of the redundant work of interval prescription renewal, freeing up staff time for more valuable contributions. Similarly, linking yearly tests (e.g., mammograms for eligible women or urine microalbumin monitoring for patients with diabetes) to the annual wellness visit saves staff from having to call and remind patients to get it done.
Set realistic expectations. If you think each patient’s needs can fit into the same predictable time per appointment, you will be frustrated and often feel like you are failing. Likewise, if you think that a patient with a 10 a.m. appointment will be seen by the physician at precisely 10 a.m., you will always be behind and feel frustrated.
A more reasonable target is to try to see the majority of patients within 20 minutes of their scheduled time (especially if the visit begins, as it should, with staff doing rooming tasks). Otherwise, you will end up prioritizing being “on schedule” at the cost of other values, such as access, continuity, flexibility, and comprehensiveness. Even attempting to see 90% of patients within 10 minutes of their appointment time could compromise aspects of care more important to patients, such as the ability to see their personal physician or to be given more time when their needs require it.
Avoid over-paneling. Some physicians have more patients in their panel than they can reasonably manage. This may be because their scheduling system allows new patients to be booked into any opening, without leaving space for existing patients who will have unexpected needs for care. Or it may be because their leadership has prioritized seeing new patients (e.g., by granting new patient visits double work Relative Value Unit credits) over maintaining appropriate access for existing patients. It can also happen when there are reductions in clinical staff without corresponding reductions in panel size.
The optimal panel size for a practice varies according to patient mix and, more importantly, practice resources. A family physician using only two exam rooms and only one medical assistant (especially if it’s a different medical assistant each day) will have a smaller panel capacity than a physician working with two registered nurses using three exam rooms. (More information on right-sizing your panel is available elsewhere.6–8)
A mismatch between panel size and team capacity will contribute to a chaotic clinic environment. It will create pressure to provide care via the patient portal, which is sometimes insufficient to meet patients’ needs and still takes time, often adding to physicians’ uncompensated labor and work after clinic.
Updating your panel size data regularly and being prepared to push back on accepting new patients if your panel is full can vastly increase your odds of scheduling satisfaction.
VALUE WORKLIFE BALANCE
The more flexibility your practice can build into your schedule using the steps above, the better worklife balance will be for physicians and the care team as a whole. Retention and recruitment will improve if physicians and staff have the flexibility to attend key life events, such as their kids’ school programs. Wave scheduling, high levels of teamwork, built-in buffer times, and a degree of decision-making authority granted to physicians closest to the patients will make it easier for practices to accommodate these personal needs.
