This supplement is sponsored by the American Academy of Family Physicians.
Fam Pract Manag. 2023;30(4):17-22
A Guide to Relieving Administrative Burden is a series of supplements developed by the American Academy of Family Physicians (AAFP) to provide information about innovations proven to relieve administrative burden and optimize your family medicine experience. It is based on AAFP Innovation Labs conducted with physicians like you, as well as a comprehensive literature review. Whether you have a solo practice or are an employee of a large health system, the guide will help you consider and adopt proven innovations.
This is the first supplement in the series. Subsequent supplements will focus on other critical administrative burdens family physicians face, including prior authorization, quality measurement and reporting, and chart review.
Fighting to Relieve Administrative Burden
A burden is a responsibility that is hard to bear. But when administrative tasks take up approximately 50% of your time1 and 57% of your colleagues in family medicine are reporting burnout (up from 47% in 2018),2 administrative burden is more than just hard to bear—it has become impossible. Our collective goal must be to relieve or eliminate the burdens, not merely reduce them. Although this goal may not be achieved quickly or easily, the AAFP is committed to helping family physicians achieve it and is fighting administrative burden on multiple fronts.
The primary battlegrounds of administrative simplification are advocacy and innovation.
Advocacy involves driving policy to relieve administrative burden, develop and promote better payment models, and protect your scope of practice. The AAFP advocates with the federal government, larger payers, employers, and health information technology (IT) vendors.3 You can find examples of the AAFP's advocacy efforts and wins on administrative simplification at aafp.org/simplification.
Innovation is focused on helping you relieve your daily burdens with necessary changes that you can implement as soon as you are ready.
Why Innovation Is Essential
Family medicine is based on an ongoing, deep physician-patient relationship that requires support from technology and appropriately funded payment models that are not burdensome and work for you, not against you. In combination, fee-for-service (FFS) payment and electronic health records (EHRs) that are not oriented to the needs of primary care have created an administrative burden that has dramatically eroded the experience of caring for patients rather than enhancing it. However, innovations to help relieve this burden and optimize the family medicine experience are available. Most family physicians do not have the time and energy to assess every solution, so this supplement provides information about innovations that are proven to relieve specific burdens and have been implemented by family physicians in a wide variety of practice settings.
The Three T's of Innovation
The innovations described in this supplement fall into three categories (“The Three T's”):
Techniques can incrementally reduce the time and effort family physicians spend on burdensome tasks. Any family physician can use these tips and tricks right away in any setting. Multiple techniques can be combined to provide moderate relief from administrative burden.
Technologies are products and services that can be purchased and integrated into practice to significantly relieve specific administrative burdens. However, adopting a particular EHR may require organizational support.
Transformations are substantial, organization-wide efforts to change how a practice operates and/or receives payment. Transformations require significant commitment, but they promise ultimate relief from specific burdens.
Innovation Road Map
Family physicians tell the AAFP that their top administrative burdens are tasks related to documentation, prior authorization, and quality measurement. The literature shows that a significant percentage of the time family physicians spend on administrative and EHR tasks is devoted to chart review (32.1%), billing and coding (3.9%), and other clerical tasks (e.g., order entry) (16.6%), in addition to visit documentation (23.7%).1 Throw in the burden of managing the EHR inbox, which accounts for 23.7% of physicians' time in the EHR, and you have a core set of common administrative challenges (Table 1). This list constitutes the AAFP's current road map for seeking innovations to reduce administrative burden, but the Academy is also continually seeking input from AAFP members to ensure it stays focused on the critical challenges for family physicians.

| Administrative Burdens | Chief Complaints |
|---|---|
|
|
EHR Documentation Burden
A seminal 2017 article in Annals of Family Medicine found that family physicians spent over 50% of the workday in their EHR, averaging 4.5 hours per day in clinic and 1.4 hours per day after clinic hours.1 Nearly a quarter of that time was spent on EHR documentation tasks. Faced with this burden, physicians must modify their workflow to shift their focus and effort during the visit from care delivery to clerical work. They may also be required to do extensive after-hours charting.5
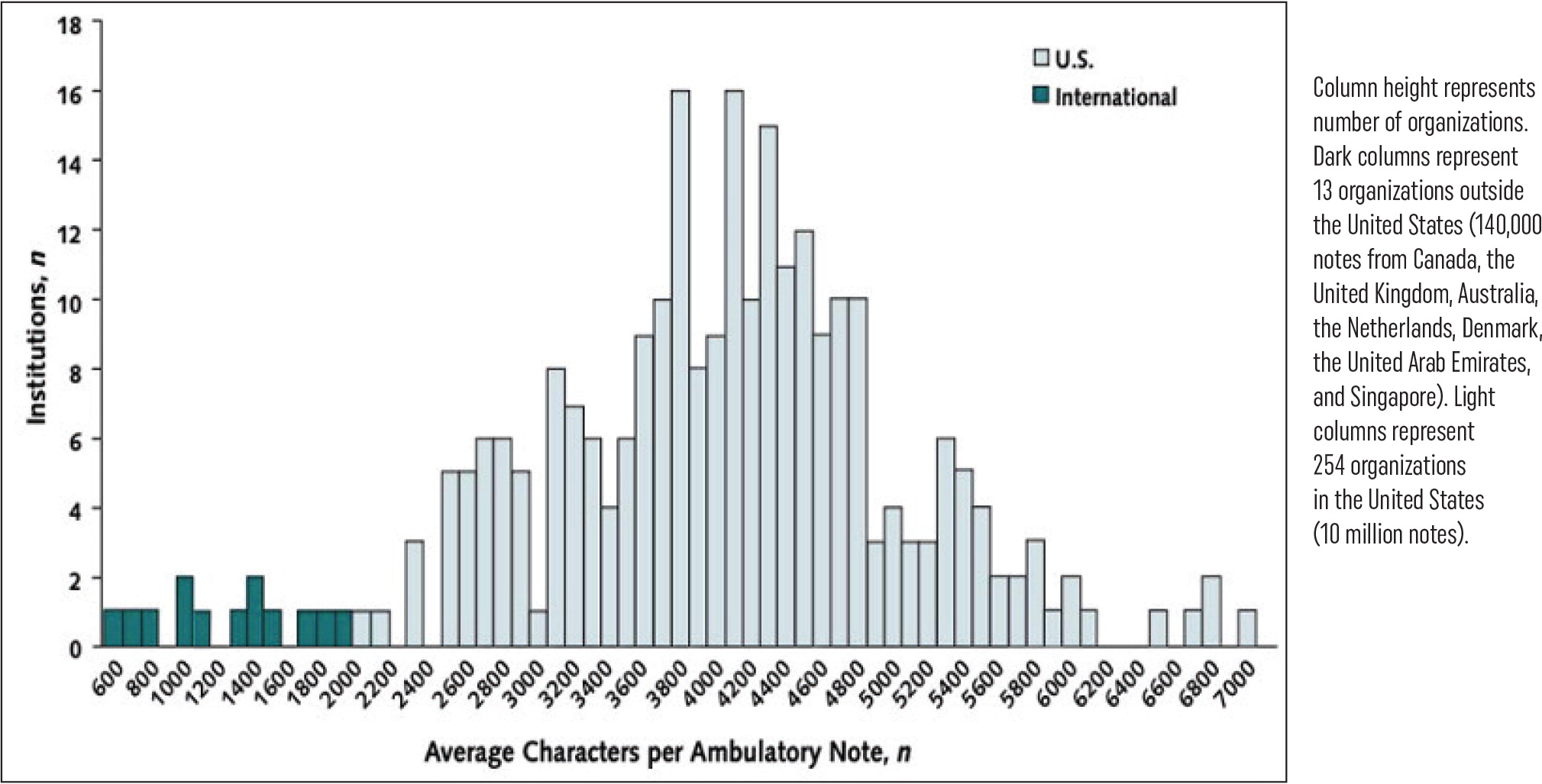
Instead of helping, traditional EHRs have only made the problem worse. Since EHRs were developed to support the insurance-driven FFS care model, they have encoded administrative tasks—and thus burden—into the physician workflow. The EHR user experience for visit documentation is outdated, using templates and forms that require excessive clicks, chart navigation, cursor placements, and typing to edit and complete. For example, Figure 1 shows the average number of characters in an EHR clinical note.
Physicians are forced to focus their eyes, hands, and minds on the EHR interface instead of on their patients. Rather than just documenting their findings and medical decision-making, they must jump through hoops to enter data, squeezing in documentation in the exam room, between visits, over lunch, and after hours every night and on weekends. In the words of one family physician, “Something has to give, and it's time with my patients and my family.”
The Three T's for Addressing Documentation Burden
In Tables 2, 3, and 4, you will find a list of techniques, technologies, and transformations for addressing documentation burden that have been identified in the literature and by family physicians working with the AAFP Innovation Lab. A relative estimate of potential burden reduction and probable cost range for each innovation is also shown. Actual impact will vary based on the practice environment and the baseline level of documentation burden. More information about these innovations and others is available at aafp.org/simplification.
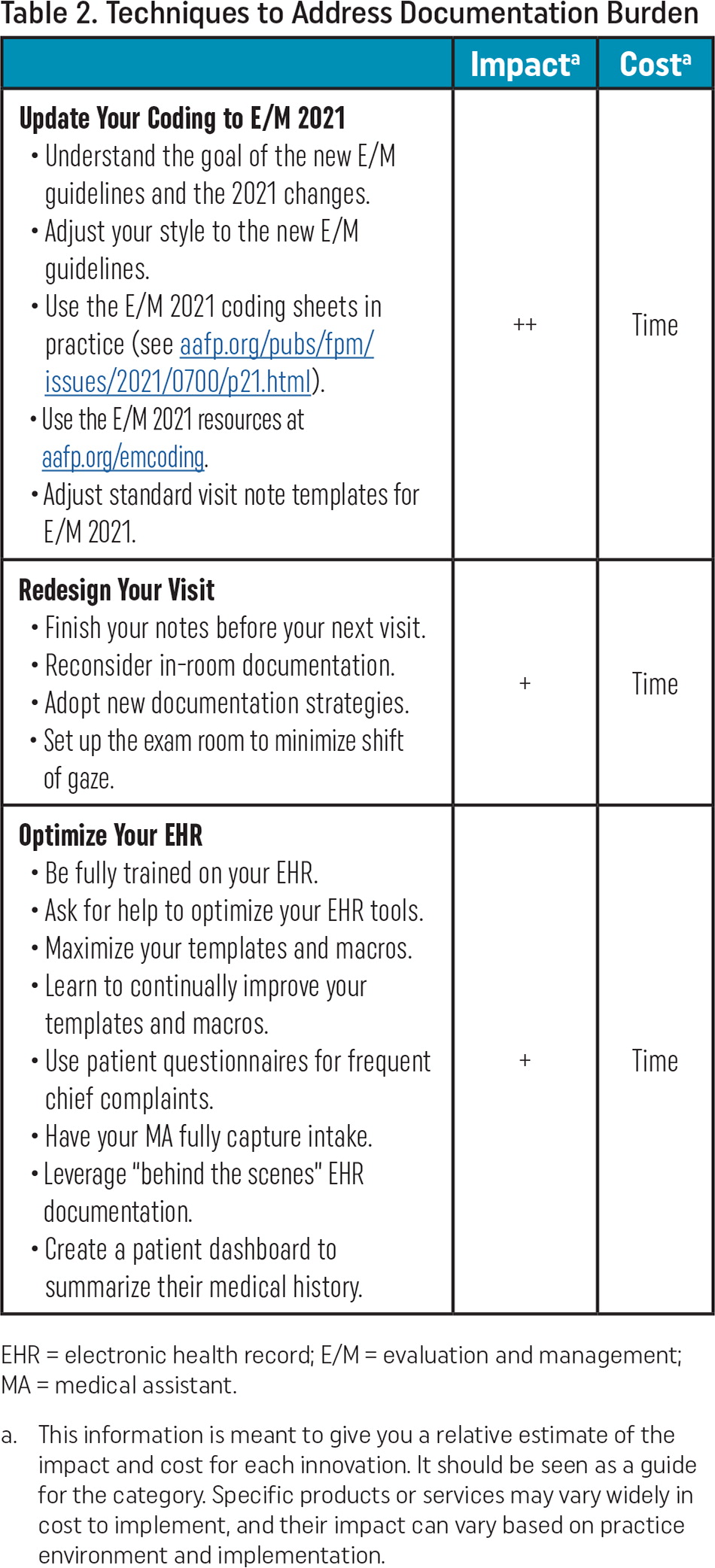
Techniques
In the techniques category, family physicians report that taking advantage of the new office visit evaluation and management (E/M) documentation guidelines can significantly reduce documentation burden (Table 2). These new guidelines—for which the AAFP strongly advocated—eliminate the need to capture bullet points in the history and physical exam sections of a clinical note. They allow physicians to focus on their assessment of the patient and care plan, with required documentation for payment based on total time or medical decision-making. This approach to E/M documentation is more clinically relevant and avoids excessive typing, data entry, and clicks.
In the AAFP's 2022 Practice Profile Survey, 51% of respondents reported a reduction in their documentation burden after implementing the new E/M guidelines. Of these respondents, 68% said it was easier to select a code, and 73% reported reduced documentation time. By contrast, 49% of survey respondents said they had not seen a reduction in their documentation burden because they were still unclear on interpretation, were unable to capture total time, had trouble using the new codes due to their workflow or EHR, or were using an EHR still coded for the old E/M codes.
If you are not using the new E/M guidelines yet, you can get helpful information and resources at aafp.org/emcoding.
| Impacta | Costa | |
|---|---|---|
Update Your Coding to E/M 2021
| ++ | Time |
Redesign Your Visit
| + | Time |
Optimize Your EHR
| + | Time |
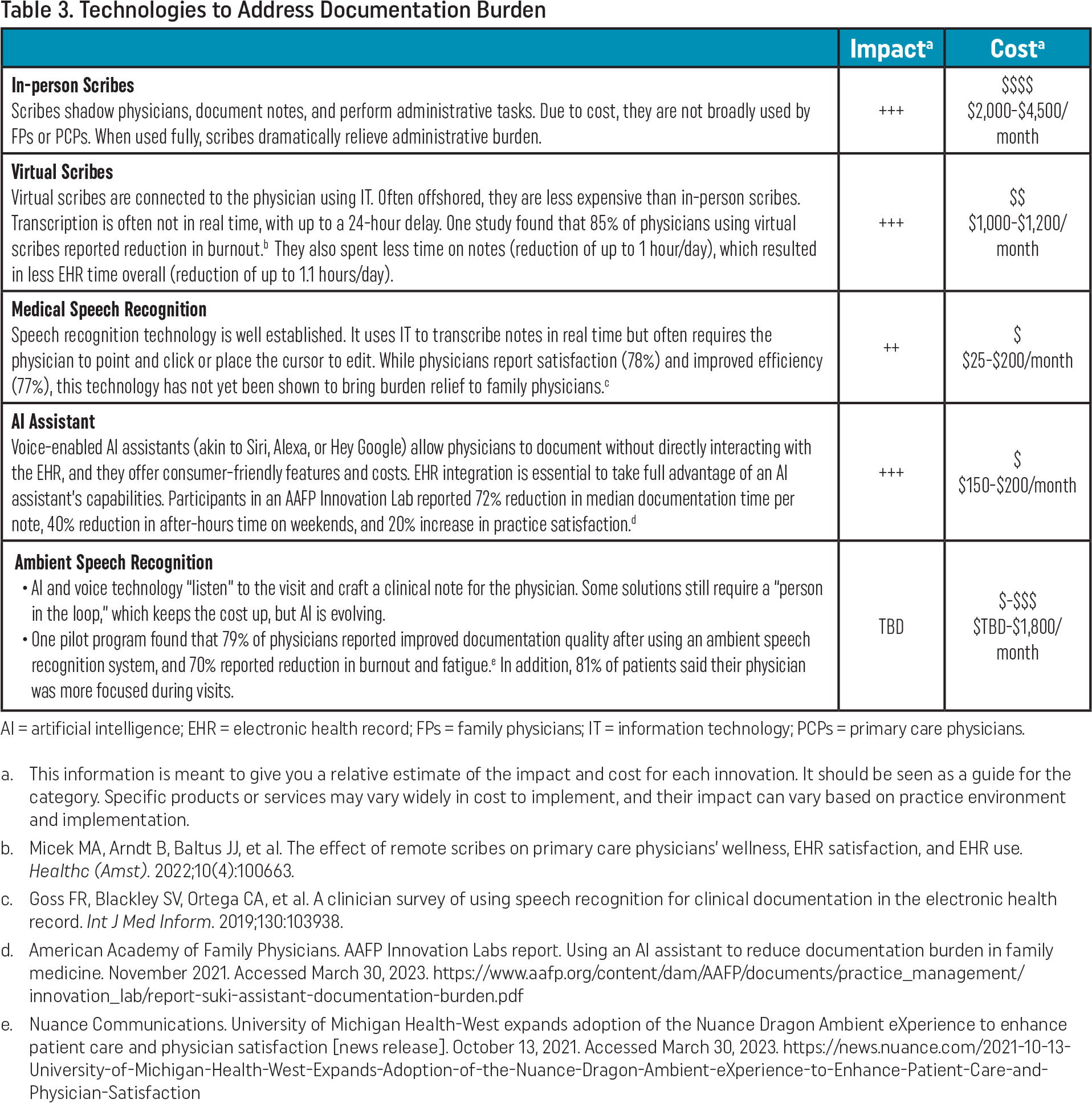
Technologies
In the technology category, scribes can dramatically reduce or eliminate documentation burden (Table 3). If the cost of employing in-person scribes to serve this function is a barrier, virtual scribes can be an impactful but less expensive alternative.6 Another technology solution to consider is an artificial intelligence (AI) assistant for documentation. These products allow you to use your voice to dictate a note and give the assistant commands (e.g., “Add my physical exam from the last visit but change the heart and lung to irregular.”). An AAFP Innovation Lab found that using an AI assistant reduced median documentation time by 72% per note.7 Members participating in the lab called the AI technology “a breakthrough.” An AI assistant can perform some of the functions of a human scribe; however, because it is software, the price point for this technology is more reasonable for family physicians.
| Impacta | Costa | |
|---|---|---|
| In-person Scribes Scribes shadow physicians, document notes, and perform administrative tasks. Due to cost, they are not broadly used by FPs or PCPs. When used fully, scribes dramatically relieve administrative burden. | +++ | $$$$ $2,000–$4,500/month |
| Virtual Scribes Virtual scribes are connected to the physician using IT. Often offshored, they are less expensive than in-person scribes. Transcription is often not in real time, with up to a 24-hour delay. One study found that 85% of physicians using virtual scribes reported reduction in burnout.b They also spent less time on notes (reduction of up to 1 hour/day), which resulted in less EHR time overall (reduction of up to 1.1 hours/day). | +++ | $$ $1,000–$1,200/month |
| Medical Speech Recognition Speech recognition technology is well established. It uses IT to transcribe notes in real time but often requires the physician to point and click or place the cursor to edit. While physicians report satisfaction (78%) and improved efficiency (77%), this technology has not yet been shown to bring burden relief to family physicians.c | ++ | $ $25–$200/month |
| AI Assistant Voice-enabled AI assistants (akin to Siri, Alexa, or Hey Google) allow physicians to document without directly interacting with the EHR, and they offer consumer-friendly features and costs. EHR integration is essential to take full advantage of an AI assistant's capabilities. Participants in an AAFP Innovation Lab reported 72% reduction in median documentation time per note, 40% reduction in after-hours time on weekends, and 20% increase in practice satisfaction.d | +++ | $ $150–$200/month |
| Ambient Speech Recognition | ||
| TBD | $-$$$ $TBD-$1,800/month |
Transformations
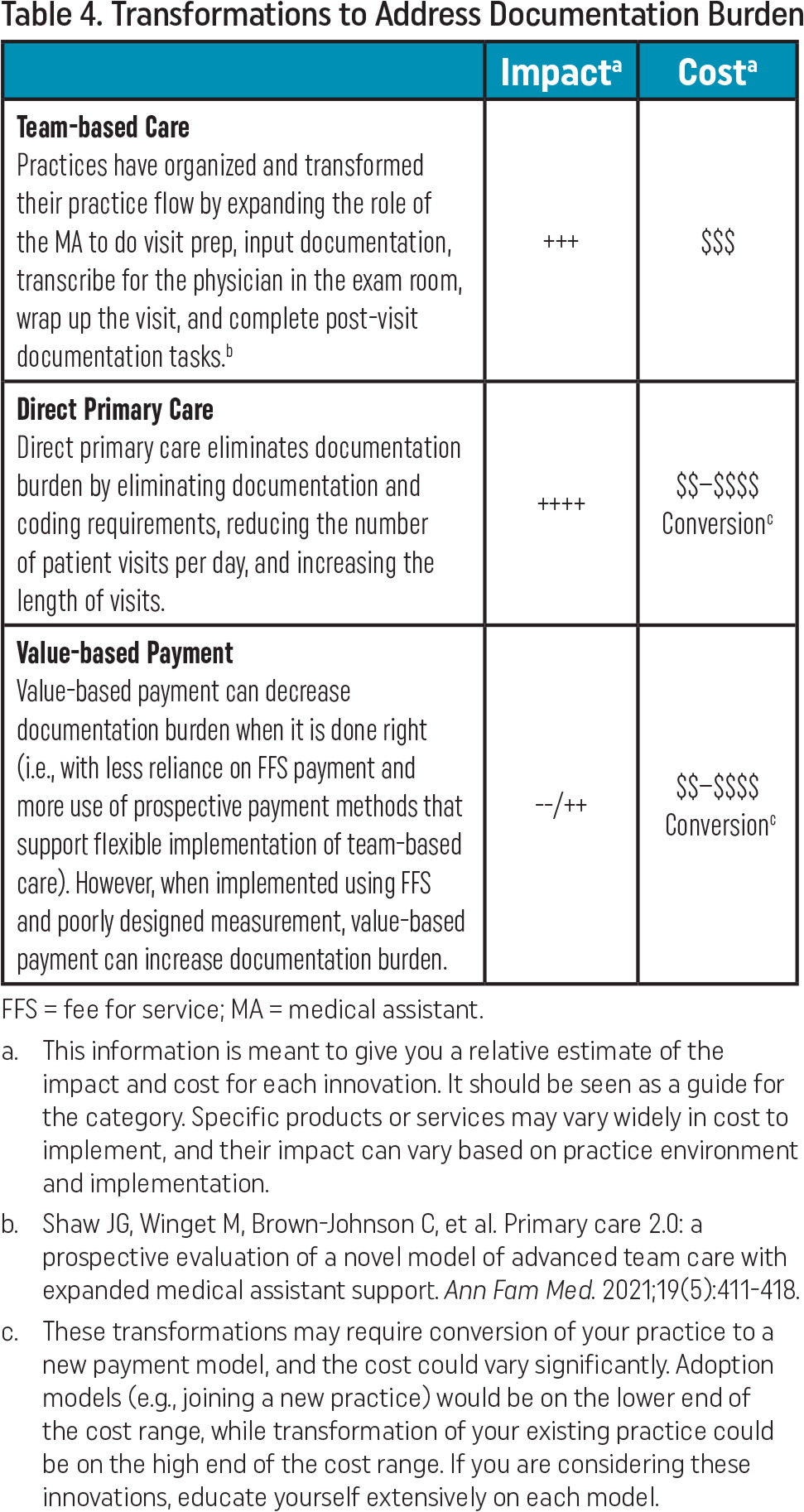
Transformations can take many forms in a family medicine practice. Two that can affect documentation burden are value-based payment (VBP) and direct primary care (DPC) (Table 4). When done right, VBP can reduce administrative burden and improve payment. Ensuring that there are more readily accessible value-based payment models that work well for primary care is a top advocacy priority for the AAFP.8
Family physicians working in practices transformed by increased financial support derived from non-FFS value-based payments report overall improvements. For example, in a recent series of conversations with family physicians in high-performing VBP practices, many reported that their investment in transformation was paying off, stating that VBP is still work, but it is “better work” that focuses more on the patient and the care team and less on administrative tasks.9 Unfortunately, results are mixed because many practices striving to deliver VBP still have to handle a high volume of FFS care.10 With team-based care and less reliance on FFS payment, VBP can decrease documentation burden.
Direct primary care reduces documentation burden by eliminating excessive insurance documentation and coding requirements. DPC practices receive their prospective revenue from individual patient subscriptions or through an employer subscription model, completely eliminating the “FFS hamster wheel.” While DPC is not a model that works for every family physician, it is a transformation that can alleviate documentation burden, and family physicians in DPC practices report high levels of satisfaction.11,12,13
| Impacta | Costa | |
|---|---|---|
| Team-based Care Practices have organized and transformed their practice flow by expanding the role of the MA to do visit prep, input documentation, transcribe for the physician in the exam room, wrap up the visit, and complete post-visit documentation tasks.b | +++ | $$$ |
| Direct Primary Care Direct primary care eliminates documentation burden by eliminating documentation and coding requirements, reducing the number of patient visits per day, and increasing the length of visits. | ++++ | $$–$$$$ Conversionc |
| Value-based Payment Value-based payment can decrease documentation burden when it is done right (i.e., with less reliance on FFS payment and more use of prospective payment methods that support flexible implementation of team-based care). However, when implemented using FFS and poorly designed measurement, value-based payment can increase documentation burden. | --/++ | $$–$$$$ Conversionc |
Leveraging The Three T's of innovation—techniques, technologies, and transformations—can help you address documentation burden. Practices interviewed by the AAFP's Center for Practice Experience & Innovation have described how these innovations are working for them. Know that you are not alone in dealing with administrative challenges. The AAFP is actively advocating for continued improvements to reduce administrative burden, improve payment, and protect the scope of family medicine.