
This supplement was supported by an educational grant to the AAFP from Abbott Diabetes Care.
Fam Pract Manag. 2024;31(1):17-18
Introduction
The American Diabetes Association’s (ADA’s) Standards of Care in Diabetes–2023 recommends consistent use of continuous glucose monitoring (CGM) for people who have type 1 or type 2 diabetes and take insulin.1 This includes any insulin regimen, whether basal insulin only, multiple daily administrations of insulin, or an insulin pump.
In April 2023, the Centers for Medicare & Medicaid Services (CMS) updated its Medicare coverage criteria for CGM, making them highly aligned with the ADA standards of care.2 In this supplement, we will discuss the potential utility of CGM in diabetes management, explore the updated Medicare coverage criteria, review CGM systems cleared by the U.S. Food and Drug Administration (FDA), and consider key steps involved in prescribing CGM and potential challenges.
How can CGM be helpful in diabetes management?
Using CGM in diabetes management has been shown to decrease A1C, even in the absence of other interventions.1 Patients describe the benefits of knowing their glucose level in real time and seeing how eating certain foods does or does not affect it. CGM can also provide much deeper insight into glucose patterns than a single value such as an A1C level. Having information about how much time a patient’s glucose level is within, above, and below the target glucose range makes it easier to identify and act upon patterns. Increased time in range is also associated with improved outcomes, including reduced risk of long-term complications.1,3
In light of how dangerous hypoglycemia can be and how often people experiencing it are asymptomatic, CGM can be especially helpful for identifying hypoglycemia.3 CGM systems can also alert patients and/or their caregivers to predicted low glucose levels so they can intervene early to prevent hypoglycemia altogether or minimize its severity and/or duration.
In addition, CGM data can be useful to calculate a patient’s glucose management indicator (GMI), an estimate of A1C based on their average CGM glucose level.4 CGM can also be used to determine the true average glucose level of patients for whom A1C is known to be inaccurate, such as patients who are pregnant and patients who have hemoglobinopathies such as thalassemia or conditions such as anemia or chronic kidney disease.
Updated Medicare Coverage Criteria for CGM
Updates to the coverage criteria for CGM allow many more Medicare beneficiaries to qualify. The patient’s medical record should show that they meet the following four eligibility requirements2:
The patient has diabetes mellitus.
The patient (or their caregiver) has been sufficiently trained on the CGM system’s use. The prescription for CGM serves as evidence that the patient meets this requirement.
CGM is prescribed in accordance with the FDA’s indications for use of the system.
CGM is prescribed to improve glycemia in a patient who is treated with insulin and/or has a documented history of “problematic hypoglycemia.”
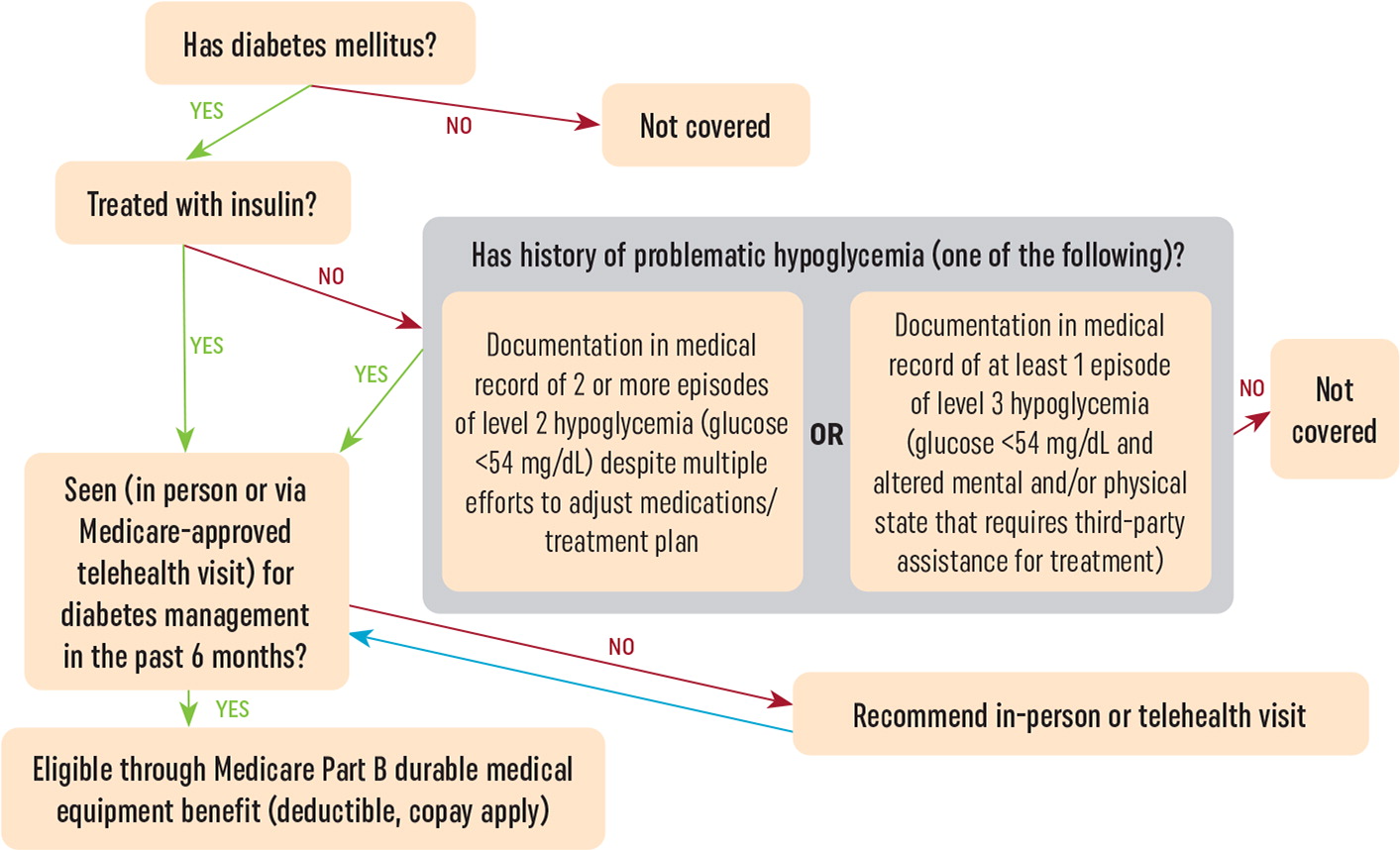
Figure 1 is an algorithm for determining a patient’s eligibility for Medicare coverage of CGM that shows how CMS defines problematic hypoglycemia.
Within six months prior to prescribing CGM, you must have seen the patient for an in-person or Medicare-approved telehealth visit for diabetes management. After a patient receives initial approval for CGM, ongoing approval requires them to have a face-to-face encounter with you — in person or via Medicare-approved telehealth — at least every six months. During these visits, you must document that the patient continues to meet the coverage criteria.
What has changed in the updated Medicare coverage criteria for CGM?
A requirement for fingerstick glucose checks is no longer included in Medicare coverage criteria for CGM, and there is no minimum requirement for frequency of insulin administration. Medicare will cover CGM for any patient treated with insulin as long as the other criteria are met. In addition, inclusion of problematic hypoglycemia in the coverage criteria means that some people who do not use insulin can now qualify for CGM.
Which FDA-cleared CGM systems does Medicare currently cover?
In order to cover CGM as a benefit, Medicare requires patients to use a CGM system with “a stand-alone receiver or insulin infusion pump classified as [durable medical equipment (DME)] to display glucose data.”2 CMS does allow patients to use a compatible smartphone, watch, or similar personal device in conjunction with a dedicated CGM receiver, but the receiver must be used at least some of the time in order for Medicare coverage to apply.
As of November 2023, four companies offer CGM systems that are cleared for use by the FDA: Abbott, Dexcom, Ascensia, and Medtronic. Currently, stand-alone CGM systems that use a durable CGM receiver are available from Abbott and Dexcom. Ascensia’s implanted CGM system provides on-body vibration, thereby meeting the Medicare criterion for a durable receiver, and it also transmits data to a smartphone app for more detailed display. The stand-alone CGM system from Medtronic solely displays data on a non-DME device (e.g., smartphone or similar personal device), so it cannot be approved for Medicare beneficiaries at this time. However, Medtronic makes an automated insulin delivery system that integrates CGM with an insulin pump. This is a CGM option for Medicare beneficiaries who would also benefit from and use this type of insulin delivery system.
Key steps for prescribing CGM
Ensure your chart notes reflect that the patient meets the Medicare coverage criteria. Document that they have a diagnosis of diabetes and are treated with insulin and/or have a history of problematic hypoglycemia.
Select a CGM system that is eligible for coverage through Medicare. As noted previously, Medicare requires patients to use a system that either has a stand-alone CGM receiver to communicate glucose data or integrates CGM with a compatible insulin pump.
Write a prescription for CGM. The prescription itself can serve as documentation that the patient or their caregiver received education on the CGM system’s use.
Send required forms and documentation to a participating DME supplier. Check companies’ websites to find resources to help you in this process, including lists of participating Medicare DME suppliers for their CGM systems. After you write and send a prescription for CGM, the supplier may ask you to submit the order on their form, complete a certificate of medical necessity, and/or attach your chart notes.
What potential challenges are involved in prescribing CGM?
The insurance authorization process is the most noted barrier to effective implementation of CGM.5 One potentially confusing aspect of this process is the fact that Medicare CGM prescriptions must be sent to a DME supplier rather than a pharmacy (unless the pharmacy is also a DME supplier). If Medicare does not approve a pharmacy’s claim, the pharmacy may communicate to you or your patient that CGM is “not covered.” However, in most cases, the claim would have been approved if it was processed through the DME benefit rather than the pharmacy benefit. If a pharmacy says CGM is not covered, try resending the prescription to a DME supplier instead.
Many patients who are prescribed CGM find it challenging to create an online user account and connect their CGM system to it. Your patients may reach out to your practice for help. If you are able to help, that is great. Manufacturers of CGM systems also offer patient education materials to assist with this process, including instruction sheets and brief online videos.
Closing thoughts
With the 2023 expansion of Medicare’s coverage criteria, many more patients stand to benefit from use of CGM and are likely to ask you about it. You can position yourself and your patients to enjoy the benefits of CGM by becoming familiar with the updated eligibility requirements, identifying which CGM systems can be approved for Medicare beneficiaries, understanding how to order and get approval for CGM, and anticipating potential challenges.
The American Academy of Family Physicians (AAFP) provides resources to help you navigate prescribing and ordering CGM for your patients at aafp.org/cgm.
This supplement was supported by an educational grant to the AAFP from Abbott Diabetes Care.
