Fam Pract Manag. 2024;31(2):4-5
The publication of this supplement is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.

The Affordable Care Act established the Health Care Payment Learning and Action Network (HCPLAN), which consists of a collaborative group of public and private health care leaders representing physician groups, hospital systems, health plans, large health care purchasers (i.e., employers, union trusts), and patients.1 The group is dedicated to accelerating the adoption of alternative payment models (APM).
The American Academy of Family Physicians (AAFP) and other organizations engaged with the HCPLAN are aligned around the need to move primary care away from the undervalued and burdensome fee-for-service (FFS) reimbursement system and toward well-designed value-based payment systems. The HCPLAN serves several purposes, including1:
Facilitating APM adoption
Standardizing the APM framework
Tracking progress and measuring its impact
Identifying and advocating for impactful policies and practices
Addressing foundational health care issues such as health equity and primary care
Overall, the HCPLAN serves as a catalyst for transforming the U.S. health care system from its current state toward one that is more efficient, sustainable, and patient-centered. Their work benefits all stakeholders—from physicians and payers to patients and employers—by promoting improved quality and experience of care, as well as reducing the rate of growth in overall health care costs.
ARE WE MAKING PROGRESS?
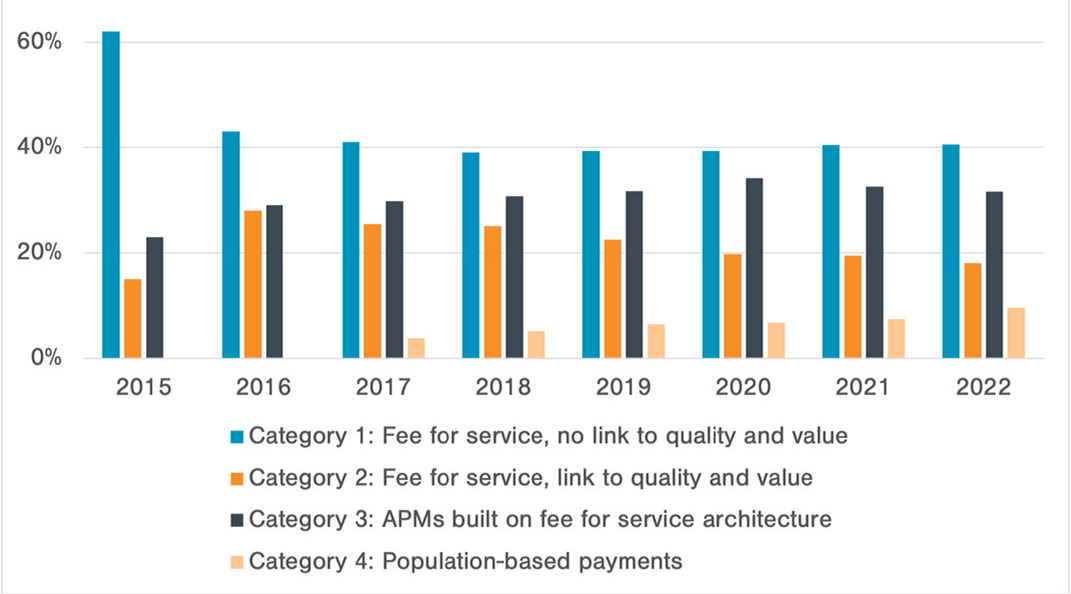
The HCPLAN released its most recent measurement report in October 2023. While it shows continued progress toward increasing APM adoption,2 progress remains slow and not at the pace and scale necessary to facilitate the changes needed in primary care. Analyzing the data reveals mixed results from 2015 to 2022 (Figure 1), with some encouraging trends observed during the period.
OVERALL MARKET MOVEMENT TO ADVANCED APMS2
There is a gradual shift toward more advanced forms of APMs, particularly those with shared savings and population-based payments.
Data shows a significant increase in payments flowing through Categories 3B and 4 compared to previous years.
In 2022, 16.5% of commercial, 30.2% of traditional Medicare, and 38.9% of Medicare Advantage dollars were in population-based payment APMs (Categories 3B-4), suggesting a growing willingness of physicians, clinicians, practices, organizations, and payers to share both rewards and risks for improved outcomes.
IMPLICATIONS FOR PRIMARY CARE
This trend presents both opportunities and challenges for primary care. Practices participating in shared savings and population-based payment APMs can potentially earn higher rewards based on improved outcomes, but in some instances, they may also face financial risk if performance falls short. Robust data infrastructure and strong care coordination are crucial to successfully transition to those payment systems.
Additionally, the recent growth in population-based payments is encouraging from a primary care perspective, as it increased from 7.4% in 2021 to 9.6% in 2022 (Figure 1)— the most significant increase reported for all categories. This is especially important to primary care because a significant revenue shift from FFS to population-based payments or “capitation” is essential to support practice transformations. A 2017 study used microsimulation to estimate that 63% of primary care practice revenue should come from capitation to provide the level of resources and flexibility to implement a more proactive and less “visit-centric” model of primary care.3
VARIATIONS BY MARKET SEGMENT2
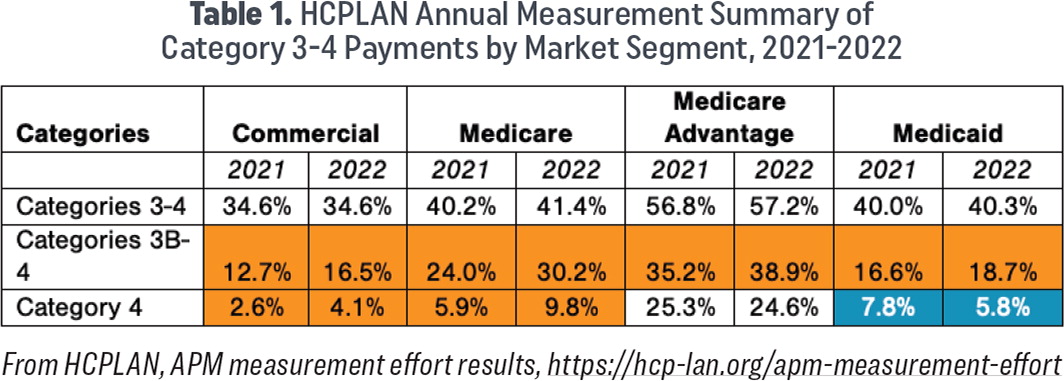
All lines of business are making progress year over year, increasing the percentage of dollars cumulatively flowing through Category 3B and 4, yet disparities in adoption exist across market segments (Table 1).
Lagging significantly behind Medicare and Medicare Advantage, both commercial payers and Medicaid fall below 6% of payments made through population-based payments.
However, commercial payers almost doubled this investment between 2021 and 2022, while Medicaid dollars decreased. Addressing these disparities through tailored strategies is crucial for ensuring equitable access to APM benefits for patients.
| Categories | Commercial | Medicare | Medicare Advantage | Medicaid | ||||
|---|---|---|---|---|---|---|---|---|
| 2021 | 2022 | 2021 | 2022 | 2021 | 2022 | 2021 | 2022 | |
| Categories 3–4 | 34.6% | 34.6% | 40.2% | 41.4% | 56.8% | 57.2% | 40.0% | 40.3% |
| Categories 3B-4 | 12.7% | 16.5% | 24.0% | 30.2% | 35.2% | 38.9% | 16.6% | 18.7% |
| Category 4 | 2.6% | 4.1% | 5.9% | 9.8% | 25.3% | 24.6% | 7.8% | 5.8% |
IMPLICATIONS FOR PRIMARY CARE
Commercial (private payers): Population-based payments in commercial lines of business pose specific challenges that make uptake slower than other market segments. The biggest hurdle is that it may require overhauling claims adjudication systems that have been in place for decades.4 While this is certainly not insurmountable, as some private payers are moving in this direction (as the data shows), it can be a daunting task. Some payers have successfully transitioned to population-based payments for primary care that other commercial plans can learn from. One way AAFP members can impact the availability of commercial plans offering population-based payments to primary care is to make their voice known to their employers or directly to their payers.
Medicaid: These results reinforce the need for the Centers for Medicare & Medicaid Services (CMS) to remain steadfast in its focus to advance health equity5 and recognize that primary care is an important evidence-based intervention to leverage in progressing their strategy to meet Medicaid patients' needs by increasing access to comprehensive, high-quality, whole-person primary care. However, primary care practices, particularly those serving as safety nets, are hampered by persistently low payments and limitations related to a volume-based payment system. New payment models that seek to increase investment are not readily available to all primary care physicians. In cases where they are, they experience significant burdens created by the unique requirements of each payer. Strategies to bridge the gap include simplifying regulations, providing technical and financial assistance to Medicaid and safety net physicians and clinicians, and developing APMs specifically tailored to the unique needs of Medicaid patients.
AAFP'S ACTIONS
Engaging with the HCPLAN is central to the AAFP's advocacy efforts, as it provides an opportunity to influence the most extensive cross-sector data collection and reporting mechanism available, which informs directional primary care payment policy decisions by multiple stakeholders.
In early 2023, the AAFP provided input to the HCPLAN's request for feedback about their 2030 goals for accountable care. In our comments, the AAFP urged the HCPLAN to consider expanding their measurement effort to include an explicit focus on primary care investment, as primary care is the foundation and cornerstone to advancing accountable care.
The AAFP's efforts are paying off. In 2023, the HCPLAN added a measure of accountable care, defined as the “total number of health plan members attributed/aligned/assigned/empaneled to a primary care provider (PCP)/primary care group (PCG) or non-PCP (i.e., specialist) participating in a total cost of care Category 3 or 4 accountable care APM in CY 2022 or most recent 12 months.”6
However, the AAFP believes the HCPLAN can do more as it conducts the nation's most comprehensive aggregation and analysis of APM data. The AAFP continues to encourage the HCPLAN to expand its measurement efforts by measuring the level of investment in primary care across the four APM categories and reporting the level of investment made in FFS or population-based value-based payment.
EMERGING ISSUE: EXPANDING APM EVALUATIONS
Measuring APM adoption over time is not enough. While the HCPLAN data is useful for informing progress, evaluations of APMs must also evolve to include not only an aggregate reduction in spending but also the ability to transform care delivery that truly improves outcomes, advances health equity, and stabilizes the primary care workforce by attracting the next generation of primary care physicians. Read more about strategies to show the benefit of value-based primary care in the Health Affairs article, ‘CMMI and Value-Based Care Play Important Roles in Advancing and Safeguarding Primary Care.’