
Failure to use exclusion codes may result in patients being counted against you in quality metrics.
Fam Pract Manag. 2024;31(4):7-10
Tool: Exclusion codes for eight common metrics
Author disclosures: no relevant financial relationships.

Value-based care systems largely rely on quality metrics and benchmarks to measure physician performance and determine payment. Understanding how insurers or other entities calculate performance — including how they attribute your patients to quality metrics and what factors would exclude patients from certain metrics — is vital for your success within these payment models.
KEY POINTS
For quality metric scores to be accurate, ineligible patients must be excluded from the calculations.
Patients may qualify for exclusion from a particular metric due to relevant disease history, frailty, or advanced illness.
Exclusions must be communicated to payers using ICD-10 codes.
THREE PARTS TO EVERY METRIC SCORE
Quality metric calculations include the following:
Numerator (the subset of patients in the denominator for whom a particular service has been provided or a particular outcome has been achieved),
Denominator (the total eligible patient population),
Exclusions (patients with characteristics that remove them from the calculation).
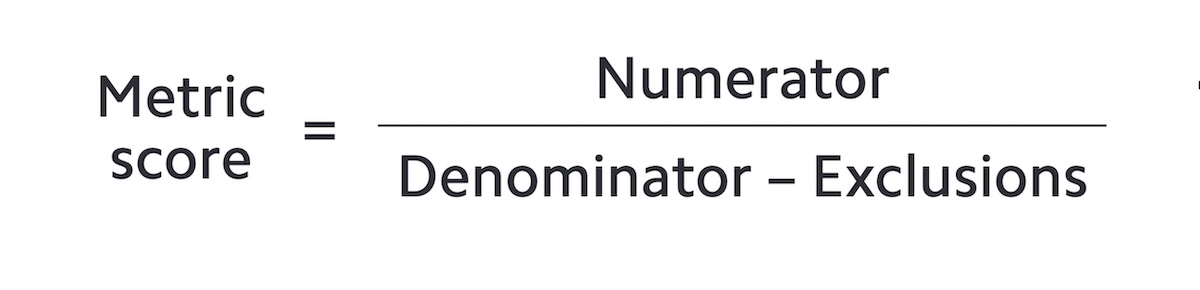
For example, a common quality metric is the percentage of women age 50–74 who had a mammogram to screen for breast cancer in the 27 months prior to the end of the measurement period. In this case, the numerator is the number of women age 50–74 who had a mammogram in the measurement period. The denominator is the total eligible population (women 50–74 years of age). The exclusions are patients who should be removed from the calculation (women who have had a bilateral mastectomy, use hospice services, etc.).
For each metric, every payer contract may specify different requirements regarding which patients are included in the denominator. Adding to this confusion, every electronic health record (EHR) system has different methods for counting and attributing patients to various metric lists. Some EHRs offer tools to assist practices in identifying patients who may require specific screenings, but a basic understanding of metric parameters is necessary in order to accurately run these reports.
UNDERSTANDING EXCLUSION CODES
To ensure that quality metrics accurately reflect a patient's need for a screening, or lack thereof, physicians need to understand how to accurately apply exclusion criteria. Exclusion codes remove patients from the denominator of certain metrics. It is essential to apply these codes accurately so the right patients are counted — and the wrong patients aren't.
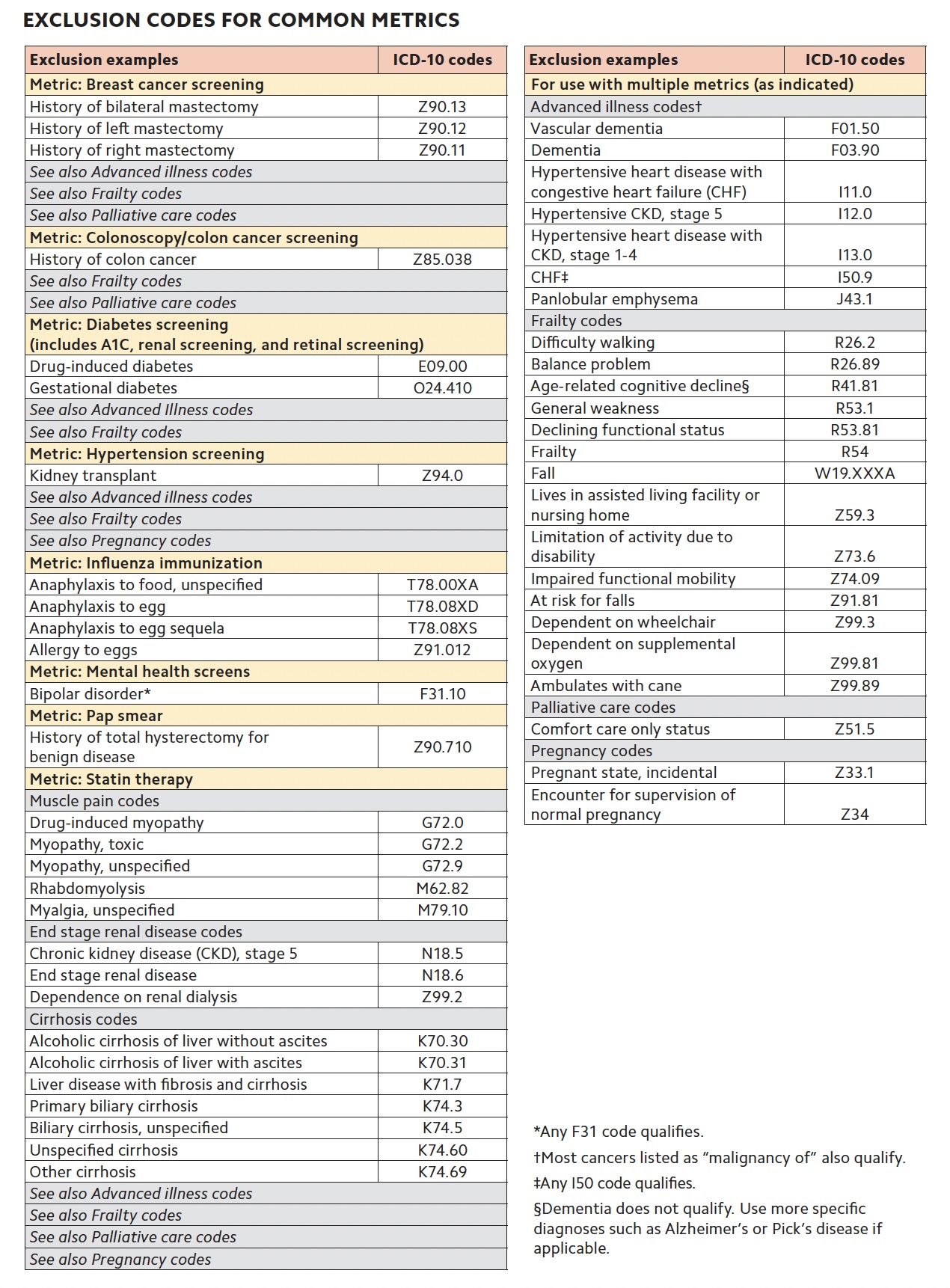
In clinical practice, physicians often encounter situations where a patient should be excluded from a metric, but the payer is unaware of this. This information can be conveyed to the payer using ICD-10 codes. The list of potential exclusion codes is extensive and includes rare conditions, such as Creutzfeldt-Jakob disease. In the chart below, we have compiled the most practical exclusion codes for eight common metrics that family physicians regularly encounter. (Because this list is not exhaustive, consult your quality manager, EHR vendor, or payers for more specific cases.) For instance, if a patient has had a hysterectomy, you can use the “history of hysterectomy” ICD-10 code to exclude them from the Pap smear metric. Failure to include this code may result in the patient remaining in your denominator and counting against you. The current requirement by the Centers for Medicare & Medicaid Services (CMS), which many other payers follow, is for physicians to enter these ICD-10 codes every year for each patient to remove them from the denominator. Streamlining this process to just once per patient would reduce physicians' administrative burden, but that change would require payer advocacy.
In addition to “history of” exclusion codes, there are also advanced illness and frailty codes that adjust your denominator. When advanced illness or frailty begins to affect a patient's functionality and overall quality of life, the importance of certain preventive screenings decreases. Family physicians frequently encounter patients with these conditions but may not always consider coding them due to their prevalence. However, applying these codes correctly can help ensure accurate metric data. Currently, advanced illness and frailty codes need to be assigned twice a year (e.g., two indications of frailty on different dates of service during the measurement year) for payers to exclude those patients from relevant metrics. Here again, payer advocacy could help streamline this process and reduce physicians' administrative burden.
Not all quality measures are affected by advanced illness and frailty codes. In the chart, we have listed some of the most commonly used advanced illness and frailty codes under the metrics to which they apply. One strategy to ensure compliance is to schedule these patients for two visits a year—one for their Medicare wellness visit and a second for a medication review — and then apply the advanced illness and frailty codes during each visit. These codes apply only to patients aged 66 and older. Another area for payer advocacy would be to allow some of these codes to apply to younger patients with disabilities or serious medical conditions.
Understanding exclusion codes can also highlight inequities and biases in metric-based payment systems for which we can advocate for our patients. For example, patients with intellectual disabilities who are nonverbal and cannot read may not be able to complete depression and anxiety questionnaires, yet there is no exclusion for them. Similarly, patients who identify as different genders may be overlooked in the EHR regarding screenings for breast and cervical cancer, with no available exclusion code. Furthermore, patients may decline certain tests for valid reasons, yet there are no exclusion codes for patient autonomy. Advocating for our patients' autonomy empowers them to make decisions about their health, but their choices should not count against us in quality metrics.
| Exclusion examples | ICD-10 codes |
|---|---|
| Metric: Breast cancer screening | |
| History of bilateral mastectomy | Z90.13 |
| History of left mastectomy | Z90.12 |
| History of right mastectomy | Z90.11 |
| See also Advanced illness codes | |
| See also Frailty codes | |
| See also Palliative care codes | |
| Metric: Colonoscopy/colon cancer screening | |
| History of colon cancer | Z85.038 |
| See also Frailty codes | |
| See also Palliative care codes | |
| Metric: Diabetes screening (includes A1C, renal screening, and retinal screening) | |
| Drug-induced diabetes | E09.00 |
| Gestational diabetes | O24.410 |
| See also Advanced Illness codes | |
| See also Frailty codes | |
| Metric: Hypertension screening | |
| Kidney transplant | Z94.0 |
| See also Advanced illness codes | |
| See also Frailty codes | |
| See also Pregnancy codes | |
| Metric: Influenza immunization | |
| Anaphylaxis to food, unspecified | T78.00XA |
| Anaphylaxis to egg | T78.08XD |
| Anaphylaxis to egg sequela | T78.08XS |
| Allergy to eggs | Z91.012 |
| Metric: Mental health screens | |
| Bipolar disorder* | F31.10 |
| Metric: Pap smear | |
| History of total hysterectomy for benign disease | Z90.710 |
| Metric: Statin therapy | |
| Muscle pain codes | |
| Drug-induced myopathy | G72.0 |
| Myopathy, toxic | G72.2 |
| Myopathy, unspecified | G72.9 |
| Rhabdomyolysis | M62.82 |
| Myalgia, unspecified | M79.10 |
| End stage renal disease codes | |
| Chronic kidney disease (CKD), stage 5 | N18.5 |
| End stage renal disease | N18.6 |
| Dependence on renal dialysis | Z99.2 |
| Cirrhosis codes | |
| Alcoholic cirrhosis of liver without ascites | K70.30 |
| Alcoholic cirrhosis of liver with ascites | K70.31 |
| Liver disease with fibrosis and cirrhosis | K71.7 |
| Primary biliary cirrhosis | K74.3 |
| Biliary cirrhosis, unspecified | K74.5 |
| Unspecified cirrhosis | K74.60 |
| Other cirrhosis | K74.69 |
| See also Advanced illness codes | |
| See also Frailty codes | |
| See also Palliative care codes | |
| See also Pregnancy codes | |
| For use with multiple metrics (as indicated) | |
| Advanced illness codes† | |
| Vascular dementia | F01.50 |
| Dementia | F03.90 |
| Hypertensive heart disease with congestive heart failure (CHF) | I11.0 |
| Hypertensive CKD, stage 5 | I12.0 |
| Hypertensive heart disease with CKD, stage 1–4 | I13.0 |
| CHF‡ | I50.9 |
| Panlobular emphysema | J43.1 |
| Frailty codes | |
| Difficulty walking | R26.2 |
| Balance problem | R26.89 |
| Age-related cognitive decline§ | R41.81 |
| General weakness | R53.1 |
| Declining functional status | R53.81 |
| Frailty | R54 |
| Fall | W19.XXXA |
| Lives in assisted living facility or nursing home | Z59.3 |
| Limitation of activity due to disability | Z73.6 |
| Impaired functional mobility | Z74.09 |
| At risk for falls | Z91.81 |
| Dependent on wheelchair | Z99.3 |
| Dependent on supplemental oxygen | Z99.81 |
| Ambulates with cane | Z99.89 |
| Palliative care codes | |
| Comfort care only status | Z51.5 |
| Pregnancy codes | |
| Pregnant state, incidental | Z33.1 |
| Encounter for supervision of normal pregnancy | Z34 |
GETTING STARTED
To begin using exclusion codes in your practice, refer to the chart. For each metric (e.g., colon cancer screening), determine whether an exclusion, advanced illness, or frailty code is applicable to your patient. If so, apply that ICD-10 code at an office visit. Remember, exclusion codes must be applied once every year, per CMS, while frailty and advanced illness codes must be applied twice a year. (Individual payer policies may differ.) To reduce your administrative burden, investigate whether your staff or EHR can assist you in reporting these codes. A best practice may be to save these ICD-10 codes in the problem list, which can streamline the process for adding them quickly.
RELATED READING
Core Measure Sets: Accountable Care Organization / Patient-Centered Medical Home / Primary Care. Core Quality Measures Collaborative.
