
Fam Pract Manag. 2025;32(3):8-10
The publication of this content is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.
WHOLE HEALTH TAKES CENTER STAGE

There's a lot of buzz these days about whole health. With life expectancy in the United States dropping in recent years,1 an emphasis on overall health and well-being is a welcome conversation. The National Academies of Science, Engineering, and Medicine recently convened experts to examine and report on whole health with its committee, Transforming Health Care to Create Whole Health: Strategies to Assess, Scale and Spread the Whole Person Approach to Health.2
The committee examined whole health and its role in improving health outcomes and recommended a future direction with priorities for health systems to scale a whole health system of care. The committee's 2023 report, Achieving Whole Health: A New Approach for Veterans and the Nation, defined whole health and described how the Veterans Health Administration used its already strong primary care infrastructure to implement a whole health approach to care.
Whole health is physical, behavioral, spiritual and socioeconomic well-being as defined by individuals, families and communities…whole health care is an interprofessional, team-based approach anchored in trusted longitudinal relationships to promote resilience, prevent disease and restore health.”3
In the 2021 report, Implementing High-Quality Primary Care: Rebuilding the Foundation, the NASEM defined primary care and described primary care's important role in whole person health.
“Primary care is the provision of whole person, integrated, accessible and equitable health care by interprofessional teams who are accountable for addressing the majority of an individual's health and wellness needs across settings and through sustained relationships with patients, families and communities.”4
Whole person health focuses on well-being rather than the absence of disease and “account for the mental, physical, emotional and spiritual health and the social determinants of health” of a person.
WHILE NOT NEW TO FAMILY PHYSICIANS, DELIVERING WHOLE HEALTH CARE REMAINS A CHALLENGE
Family physicians have been practicing whole health for as long as the specialty of family medicine has existed.5 While lifestyle medicine, integrative medicine and functional medicine are newer concepts considered whole health disciplines, they are not the only approaches family physicians provide to treat the whole person. The goals and features of these disciplines are part of, and interwoven into, family medicine's approach to care, such as encouraging better nutrition, regular movement, improved sleep habits, better stress management and connection to community resources, to name a few. Collectively, these approaches, along with many others, constitute whole health care and are at the crux of the integral role family physicians play in the health care system.
At the American Academy of Family Physicians, we are privileged to witness the amazing work of family physicians every day, and we believe that family medicine is whole health. We also see the challenges family physicians and other clinicians face in delivering whole health in a system that rewards the treatment of disease over the achievement of health. Whether you call it whole health, lifestyle medicine, integrative medicine or something else, the concepts represent comprehensive, person-centered care that contributes the most to achieving and maintaining health.6
We admire the passion of family physicians in helping patients realize their best, healthiest selves using whole health approaches. However, prevailing health care payment systems (i.e., insurance plans) scarcely consider many whole health interventions to be “health care services,” making it all the more challenging to incorporate them into everyday practice at scale. Inadequate payment means many of these services are not covered at all and/or are not paid at a rate that accurately reflects the time and efforts of physicians and their teams.3,4 Making the health care system more challenging is the fact that, to some degree, physician training remains more heavily focused on traditional medical interventions than on broader lifestyle/behavioral interventions, the latter of which often have the greatest positive impact on patient health.6,7
ADDRESSING SYSTEMIC BARRIERS IS ESSENTIAL TO ACHIEVING WHOLE HEALTH
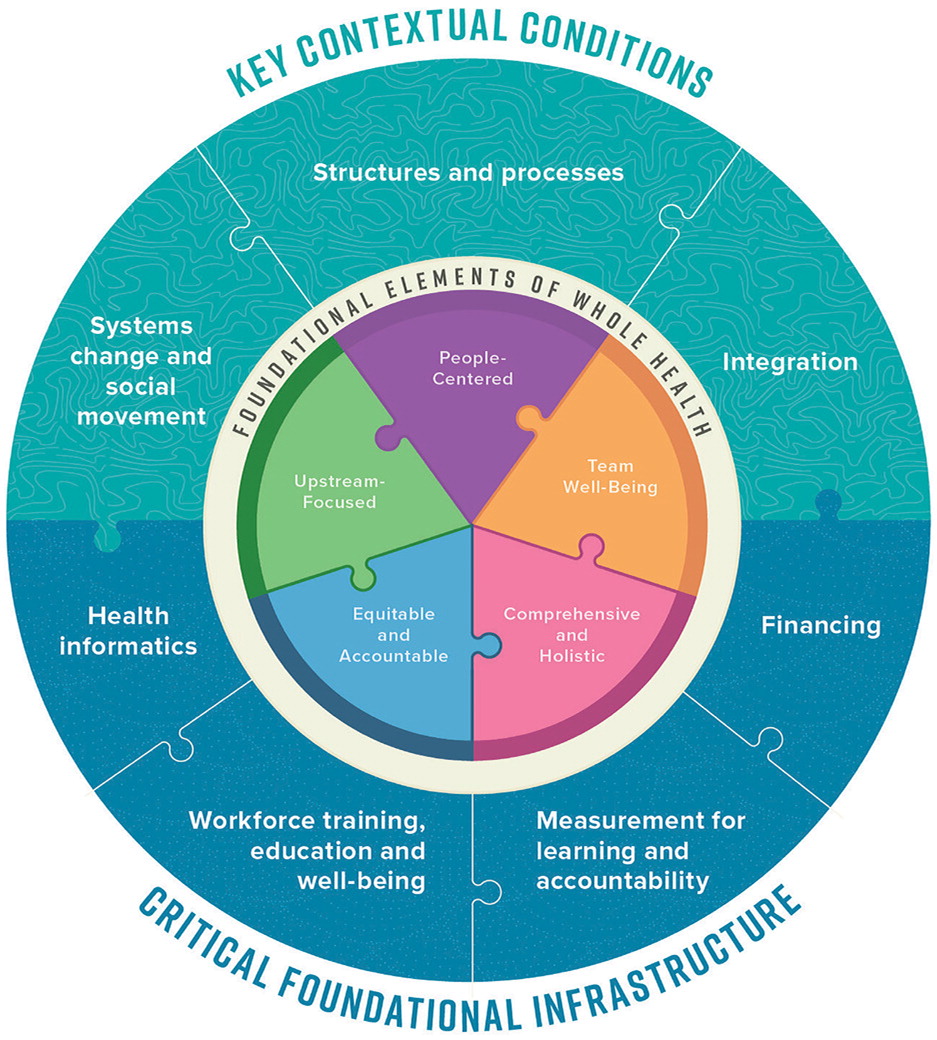
The NASEM whole health report provides a helpful framing of the foundational elements, contextual conditions and critical infrastructure needed for a health care system oriented toward achieving whole health.3 The priorities of family physicians and the work of the AAFP to address the challenges you face can be found throughout this framework.
In this Beyond the Beltway feature, we highlight the AAFP's efforts related to financing and payment, as well as training and education, aimed at incorporating whole health. We also share our plans to further engage the AAFP's physician leaders to shape the national conversation on whole health with a gathering in late fall 2025.
Financing and Payment
Improving primary care payment systems and reducing administrative burdens are two of the highest priorities expressed by AAFP members.8 Achieving these goals is central to the AAFP advocacy efforts in the public and private sectors.
The AAFP's payment advocacy (https://www.aafp.org/advocacy/advocacy-topics/physician-payment.html) focuses on increasing payment allocated to primary care and removing the burdensome documentation of payment systems. AAFP Board Chair Dr. Steven Furr made this clear in his Senate Finance Committee testimony (https://www.aafp.org/news/government-medicine/bolstering-medicare-testimony.html) telling senators that fee-for-service medicine “doesn't just underinvest in primary care, it also makes it extremely complex to get paid.”9 He emphasized the unreasonable burdens by describing FFS payment in primary care as “trying to cut a roll of paper with a hole punch rather than a pair of scissors.”
Our advocacy efforts reflect the AAFP's commitment to improving the primary care infrastructure and practice environment, addressing systemic barriers to accessing health care and properly investing in primary care to ensure family physicians can provide high-quality, whole person patient care. These efforts help all practice settings – from physician-owned and physician-led independent practices to practices embedded in larger organizations and residency programs.
Training and Education
Positioning family physicians for success in a whole health approach will require more than just improving primary care payment. The training and education of medical students, residents and family physicians currently focus more on diagnosing and treating patients' symptoms than integrating lifestyle, behavior and social health improvements. Training and education should include offerings on what NASEM refers to as the physical, behavioral, spiritual and socioeconomic well-being of patient care,3 moving beyond solely treating symptoms.
FAMILY PHYSICIANS LEADING THE CHARGE
Family physicians and the AAFP must be vocal leaders in spreading the message that primary care brings a unique and essential value to treating patients' holistic needs to improve the nation's health. Leveraging the research and work NASEM and others bring to whole health, the AAFP is convening family and other primary care physicians from across a wide range of disciplines and perspectives. Key stakeholders who influence primary care payment and training will join us in developing plans that ensure these critical foundational elements are well-informed and implemented to support primary care's essential role in delivering whole health care. In late fall of 2025, we will gather physician leaders, federal and state policy leaders, health plan representatives, employers and patients. The group will produce an action brief on how primary care payment and training MUST change to accomplish the shared aims of family physicians and the growing cadre of whole health champions.
We welcome the opportunity to continue the great work in whole health and express our gratitude to the Ardmore Institute of Health for their support related to many of the AAFP resources you'll find in the next section. We are also grateful to the Healing Works Foundation who is joining them to make the gathering in the fall of 2025 a reality.
In addition to our leadership on whole health, the AAFP remains committed to helping our members revolutionize America's health system by transforming it from one that thrives by identifying and treating illness (in both payment systems and training) to one that focuses on achieving and sustaining health across individuals' lifespan. While we continually push Congress and others for sweeping, systemic changes in all areas of medicine, we will also continue to help family physicians gain the knowledge, skills and tools they need to get to the root of what matters most to their patients in achieving whole health.
AAFP RESOURCES
In addition to the resources and information available through other sources, the AAFP has numerous resources to help you incorporate a broad range of lifestyle and behavioral interventions in your practice setting.
If you have experience and perspective that you would like to share, please contact us at asktheexpert@aafp.org. We would love to hear from you.
Incorporating Lifestyle Medicine into Everyday Family Practice: Implementation Guide and Resources
