
These simple strategies based on self-determination theory can help you maximize your patients’ motivation to change.
Fam Pract Manag. 2025;32(4):8-14
Author disclosures: no relevant financial relationships.
Facilitating patient behavior change is a constant challenge for primary care physicians and other clinicians. According to one estimate, up to 75% of primary care visits involve engaging patients in changing a habit or starting medications.1 Given the time pressure and complex psychosocial dynamics we encounter daily in primary care, it can be daunting to effectively promote behavior changes that will improve health outcomes. Ultimately, the motivation to change must come from patients themselves. The key question is how can we maximize our patients’ motivation to change?
The answer lies in self-determination theory (SDT). By incorporating simple, evidence-based strategies rooted in SDT,2 clinicians can help facilitate behavior change, foster stronger patient relationships, improve patient outcomes, and reduce frustration for both clinicians and patients.
KEY POINTS
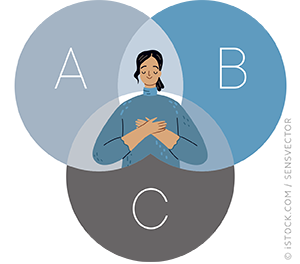
Self-determination theory posits that individuals have three basic psychological needs that are essential for motivation and well-being — autonomy, belonging, and competence.
By understanding these needs and actively supporting them through simple, evidence-based strategies, clinicians can enhance their effectiveness in helping patients internalize behavior change and achieve lasting results.
This approach shifts clinical dialogue from “need-thwarting” to “need-supporting.”
Subscribe
From $110- Immediate, unlimited access to all FPM content
- 30 CME credits/year
- Print delivery available
Issue Access
$39.95- Immediate, unlimited access to this issue's content
- CME credits
- Print delivery available
Article Only
$25.95- Immediate, unlimited access to just this article
- CME credits
- Print delivery available
