
Fam Pract Manag. 2026;33(1):5-8
The publication of this content is funded by the American Academy of Family Physicians. Journal editors were not involved in the development of this content.

Since the health care quality measure movement began more than 25 years ago, transparent quality-performance information has become more widely available. With the information, comes some benefits but also risks and unintended consequences. Measurement can lead to greater accountability and improved care.1,2,3 However, the proliferation of measures has also caused confusion, increased burden and burnout, and spurred misalignment of approaches.
A recent study found that primary care physicians are required to report an average of 57 unique performance measures (PMs) to different payers through various contracts.4 For 2025, 66 measures are included in the family medicine specialty set for the Centers for Medicare & Medicaid Services (CMS) Merit-based Incentive Payment System.5 Among the 66 measures, family physicians must select six measures to report on. Overall, nearly 350 PMs are currently endorsed,6 some designed to evaluate care provided by family physicians.
Reducing the number of performance measures for primary care practices participating in value-based payment is essential to continued growth in alternative payment models. Aledade, a national network of independent primary care practices, reports on 108 different performance measures across many payer contracts.7 Aledade asserts—and the American Academy of Family Physicians (AAFP) agrees—that primary care shoulders a disproportionately large burden of performance measure reporting when compared to other medical specialties.
Multistakeholder Efforts to Align Measures, Reduce Burden
To alleviate the burden and other unintended consequences associated with performance measurement, CMS and public-private partnerships have attempted to create more parsimonious sets of measures through various efforts, such as aligning measures across federal programs8 and the Core Quality Measures Collaborative (CQMC).9 While these efforts are laudable for their intent, the lack of alignment across payers and programs continues to create challenges for family physicians, care teams and patients. One of the most challenging issues in primary care performance measurement is that many of the factors that influence performance, such as patient cost-sharing that interferes with medication adherence, are beyond physicians’ control (see the AAFP’s advocacy on the 2025 Medicare Physician Fee Schedule). From a more technical perspective, some measures are misapplied at the individual clinician level when they have been tested and validated only for use at the system or health plan level, and some measures do not lead to measurable improvements in patient outcomes.10
AAFP Advocacy Evolves
The AAFP has engaged in national advocacy to influence and improve the measurement landscape since the beginning of health care quality measurement. As a founding member of the National Quality Forum in 1999, the Academy had family physicians serving on technical expert panels, workgroups and committees that reviewed single quality measures one at a time. In this early era, measurement focused on internal quality improvement (QI) within organizations. Measurement has since evolved, and QI has progressed to performance measurement, which is used by public and private payers, often with financial incentives and/or penalties tied to performance.
The AAFP’s advocacy approach continues to evolve alongside the broader measurement landscape. While family physicians often focus their day-to-day efforts on internal QI within their clinics, the AAFP’s national advocacy efforts focus on performance measurement tied to payment. Thus, we engage with multiple stakeholders at every stage of the performance measure lifecycle.
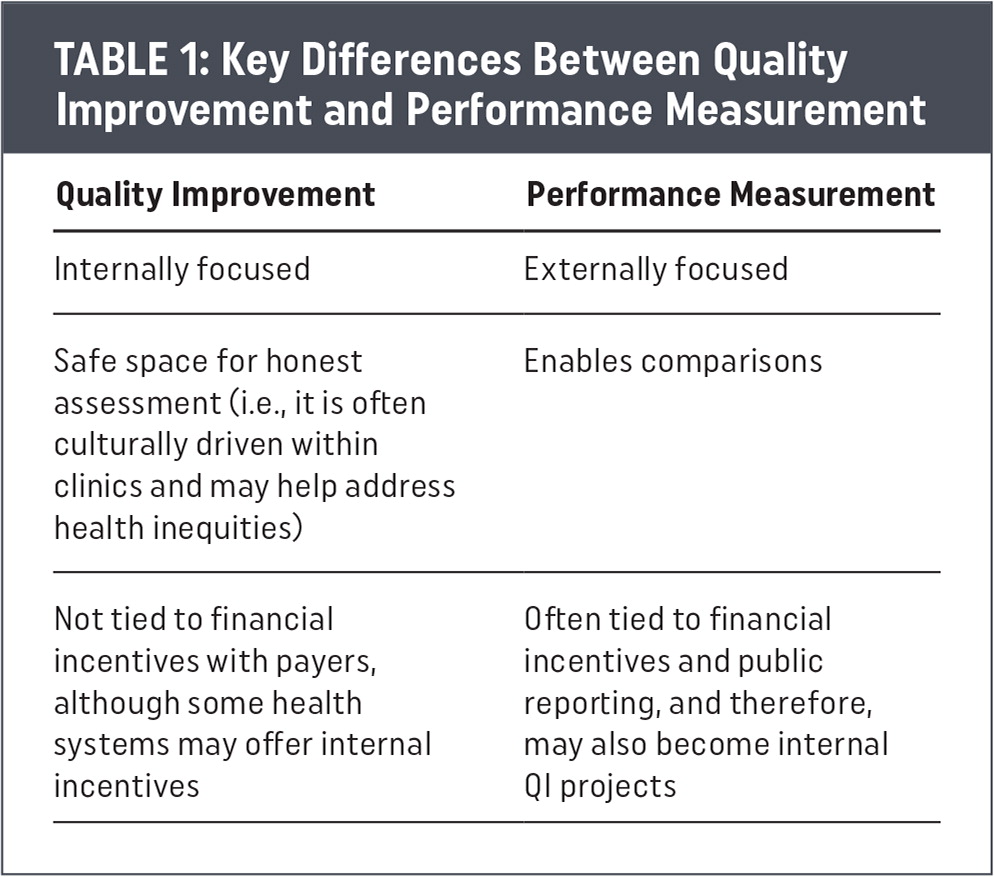
Key Differences Between Quality Improvement and Performance Measurement
| Quality Improvement | Performance Measurement |
|---|---|
| Internally focused | Externally focused |
| Safe space for honest assessment (i.e., it is often culturally driven within clinics and may help address health inequities) | Enables comparisons |
| Not tied to financial incentives with payers, although some health systems may offer internal incentives | Often tied to financial incentives and public reporting, and therefore, may also become internal QI projects |
Lifecycle of a Performance Measure
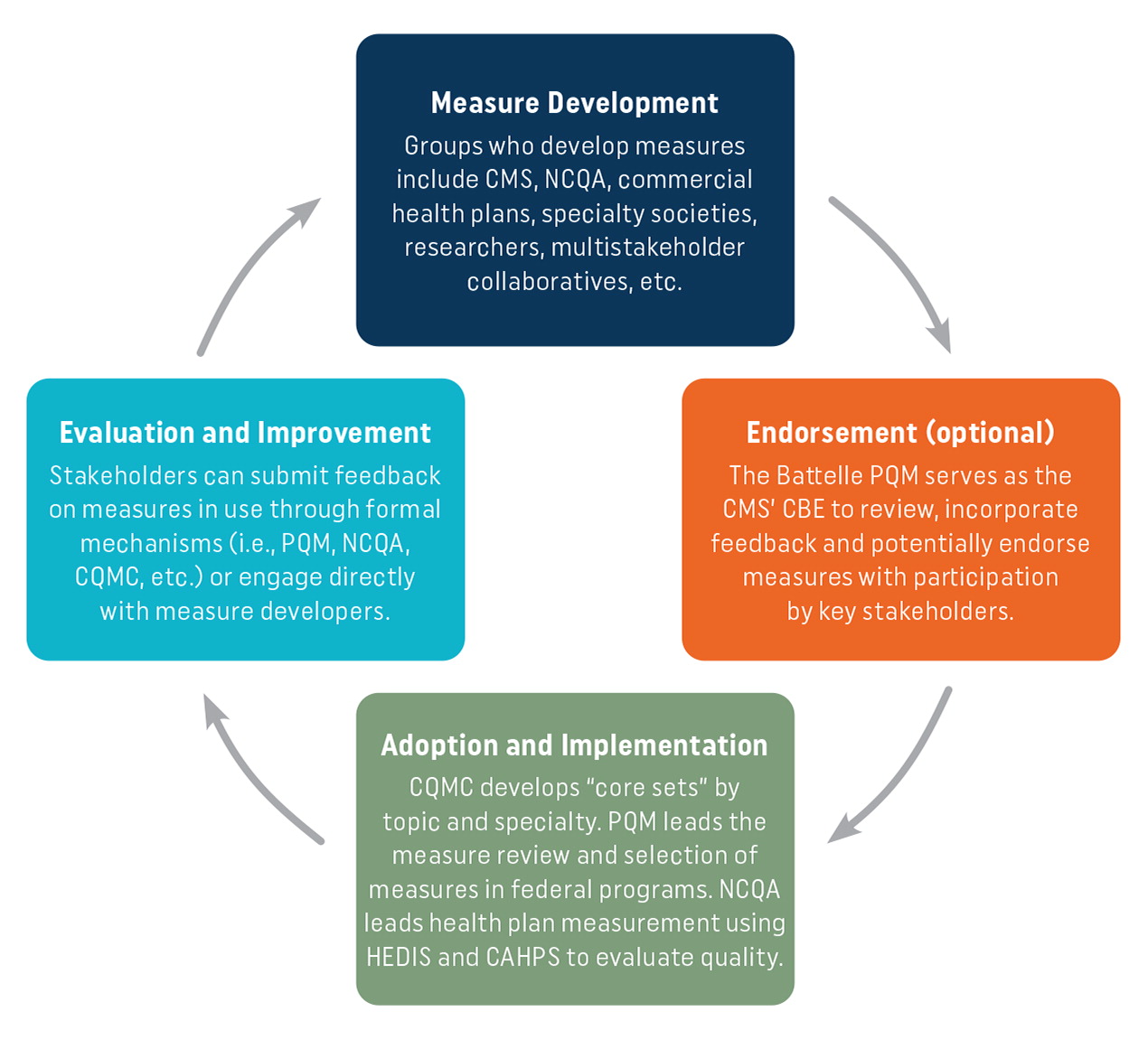
The development and use of a performance measure is a cyclical process involving many stakeholders and roles, including the following:
Measure development – Key players develop measures, including CMS, other federal agencies, the National Committee for Quality Assurance (NCQA), specialty societies, researchers and delivery organizations.11 These groups collaborate to design measures that reflect clinical priorities and quality goals.
Endorsement – Once developed, many measures undergo an optional endorsement process to ensure validity and reliability.12 The Partnership for Quality Measurement™ (PQM) serves as CMS’ consensus-based entity (CBE) for this endorsement, working with stakeholders to review and endorse measures.
Adoption and implementation – Even if a measure is not officially endorsed, it may be adopted by CMS, private health plans, providers and programs.13 Adoption and implementation occur when measures are integrated into practice and reporting systems.
Evaluation and improvement – Endorsed measures in use are re-evaluated for effectiveness and relevance by a CBE every five years.14 There is no requirement for non-endorsed measures to be re-evaluated. At re-evaluation, stakeholders can submit feedback through formal mechanisms, such as through PQM or by engaging directly with measure developers. This feedback may inform updates and refinements, and/or measures may be removed from federal payment programs.
The AAFP engages and advocates at every stage of the measure lifecycle by serving on technical expert panels and committees, commenting on rules and advocating among key stakeholders. Figure 1 illustrates the key players and processes of the measure lifecyle and Table 2 outlines the Academy’s role, actions and stakeholders we engage with for each stage of the measure lifecycle.
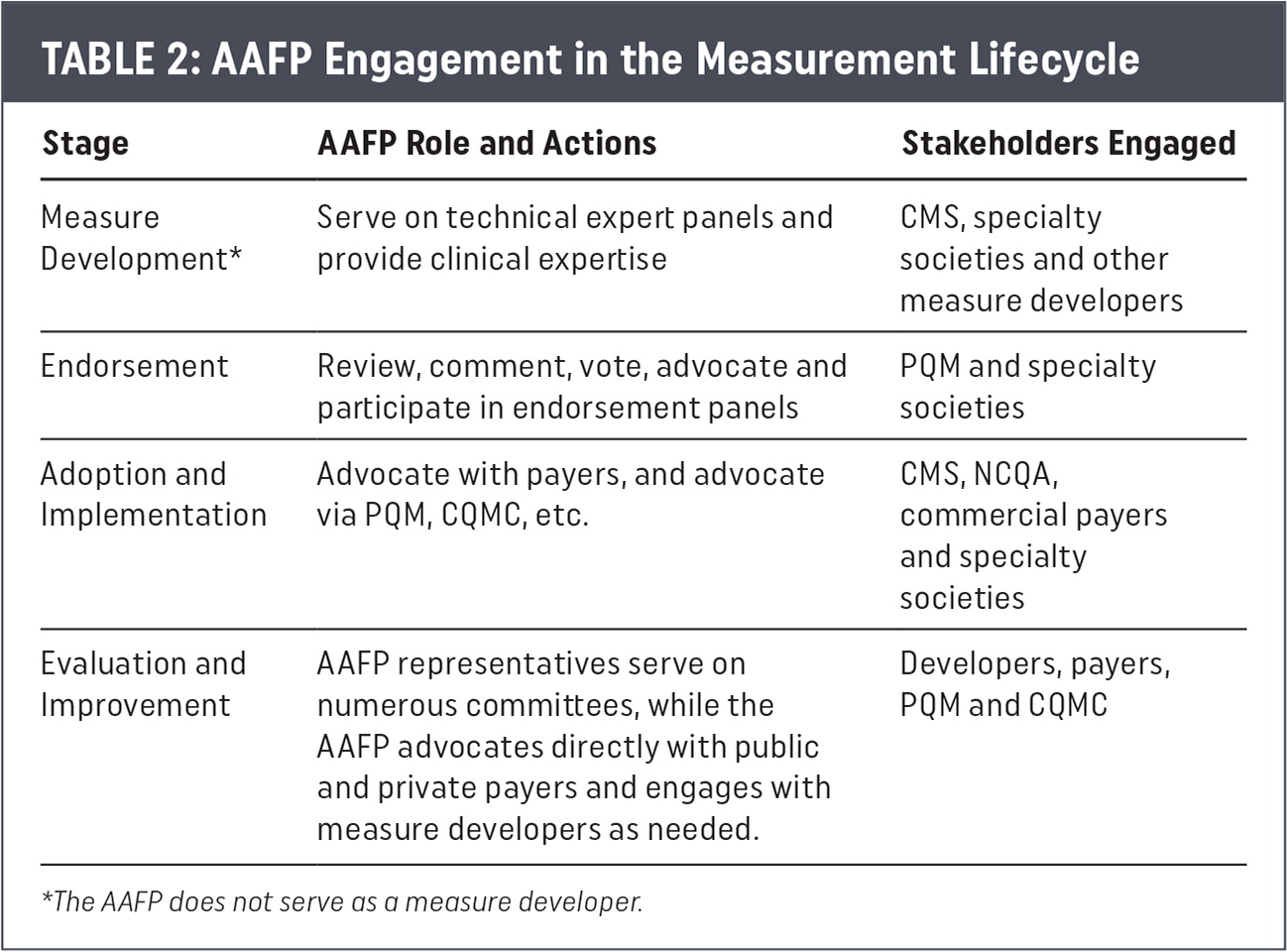
AAFP Engagement in the Measurement Lifecycle
| Stage | AAFP Role and Actions | Stakeholders Engaged |
|---|---|---|
| Measure Development* | Serve on technical expert panels and provide clinical expertise | CMS, specialty societies and other measure developers |
| Endorsement | Review, comment, vote, advocate and participate in endorsement panels | PQM and specialty societies |
| Adoption and Implementation | Advocate with payers, and advocate via PQM, CQMC, etc. | CMS, NCQA, commercial payers and specialty societies |
| Evaluation and Improvement | AAFP representatives serve on numerous committees, while the AAFP advocates directly with public and private payers and engages with measure developers as needed. | Developers, payers, PQM and CQMC |
AAFP Advocates Upstream to Improve Downstream Practice Environment
Current AAFP advocacy focuses on influencing upstream stakeholders to improve the downstream measurement environment at the practice level. Upstream stakeholders, such as CMS and NCQA, are decision-making bodies whose actions heavily influence which measures are included in payment programs that affect AAFP members. Our upstream advocacy includes close collaboration with the quality and performance measurement teams at the American College of Physicians, the American Medical Association and other specialty societies that share our concerns and collective goals to improve the measurement environment for our physician members.
The AAFP currently has representatives serving on more than 20 measure development and/or measure review panels, including national panels that recommend whether measures should be added or removed from federal payment programs. In addition to these measure-specific committees, the AAFP regularly meets with the nation’s largest private payers to advocate for measure alignment, burden reduction and increased payment for primary care.
The following AAFP position paper and policy statements guide all our measurement advocacy:
To effect change locally, AAFP members are encouraged to engage with their local AAFP chapters to advocate for change with their local and regional payers.
Rethinking Measurement
The American Board of Family Medicine, through The Center for Professionalism & Value in Health Care, offers a new approach to measurement focused on capturing the unique value of primary care through its Measures that Matter to Primary Care (MTM) initiative.17 Their four performance measures align with the functions of family medicine. This targeted initiative aims to create measures that reflect the value of family medicine and could replace some of the measures currently in use.
The AAFP has provided detailed input on these measures and will continue to do so as they are further refined and begin to gain wider adoption. In the meantime, the Academy will continue its strong advocacy and engagement in the performance measurement process at every stage of the measure lifecycle.
Conclusion
There are too many measures, the measurement process is inefficient and burdensome, and the measures do not always reflect the value of primary care or improve patient outcomes. Despite these challenges, the AAFP will continue to push key stakeholders throughout the process to better align measures with the value functions of primary care and to ensure our members’ priorities are represented. We are encouraged by the goals of the MTM initiative to help reduce primary care practice burden and burnout, support better physician-patient relationships and their experiences, improve patient care and outcomes, and reduce costs in the health care system. By advocating upstream at the national level to reduce the downstream practice-level burden, our goals remain the same as they always have been—to allow you to focus on what you do best—care for your patients.
