
Am Fam Physician. 1998;57(11):2775-2782
Hoarseness is the term often used by patients to describe changes in their voice quality. The causes of hoarseness are determined after obtaining a detailed medical history of the circumstances preceding the onset of hoarseness and performing a thorough physical examination. The latter may include visualization of the vocal cords, possibly using indirect laryngoscopy, flexible nasolaryngoscopy or strobovideolaryngoscopy. In the absence of an upper respiratory tract infection, any patient with hoarseness persisting for more than two weeks requires a complete evaluation. When the patient has a history of tobacco use, cancer of the head and neck must be considered and ruled out. Voice abuse is one of the most common causes of hoarseness and can lead to other vocal pathologies such as vocal nodules. Good vocal hygiene can prevent and treat some pathologies, and voice therapy is a cornerstone of management in some cases of hoarseness.
Hoarseness has many causes, ranging from a simple upper respiratory tract infection to a serious pathology such as head and neck cancer. This article discusses voice changes that may be described by patients as hoarseness and addresses the most important etiologies (Table 1). The physiology of voice production, diagnostic techniques for voice evaluation and recommendations for voice disorder prevention are outlined.
| Functional dysphonia | Abnormal use of the vocal mechanism despite normal anatomy. This condition can be related to stress, psychologic disturbance or habituation of compensatory techniques developed during an upper respiratory infection. |
| Laryngeal papilloma | Growths on the larynx caused by human papilloma viral infection. |
| Muscle tension dysphonia | A voice disorder resulting from excessive or unequal tension while speaking. This condition results from improper speaking technique and is commonly associated with reflux laryngitis. |
| Reflux laryngitis | Inflammation of the larynx caused by gastric acid irritation. |
| Reinke's edema | An accumulation of fluid in the vocal cords. This condition is associated with smoking and voice abuse. It may also occur with reflux laryngitis. |
| Spasmodic dysphonia | A condition resulting in irregular voice breaks and interruptions of phonation. This is a focal dystonia of the laryngeal muscles. |
| Vocal cord paralysis | Weakness or immobility of the vocal cord(s). |
| Vocal nodules | Fibrotic formations on the vocal cords. Commonly referred to as “nodes.” |
Definition
Dysphonia is defined as an abnormal voice quality. The patient's complaint of hoarseness frequently represents something entirely different from the way the physician defines hoarseness, so it is important that the physician consider the different descriptions of voice quality when evaluating a patient's complaint. Voice quality may be described as breathy, strained, rough, tremorous or weak. On questioning, the physician may discover that what the patient terms hoarseness is actually increased vocal effort or vocal fatigue. Other aspects of dysphonia to inquire about, particularly in patients who are singers, are changes in pitch and abnormal pitch range. These specific disturbances often help the physician focus on possible diagnoses (Table 2).
| Voice quality | Differential diagnosis |
|---|---|
| Breathy | Vocal cord paralysis, abductor spasmodic dysphonia, functional dysphonia |
| Hoarse | Vocal cord lesion, muscle tension dysphonia, reflux laryngitis |
| Low-pitched | Reinke's edema, vocal abuse, reflux laryngitis, vocal cord paralysis, muscle tension dysphonia |
| Strained | Adductor spasmodic dysphonia, muscle tension dysphonia, reflux Laryngitis |
| Tremor | Parkinson's disease, essential tremor of the head and neck, spasmodic dysphonia, muscle tension dysphonia |
| Vocal fatigue | Muscle tension dysphonia, vocal cord paralysis, reflux laryngitis, vocal abuse |
Voice Production
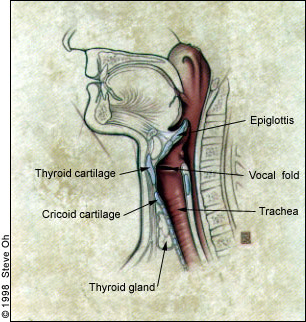
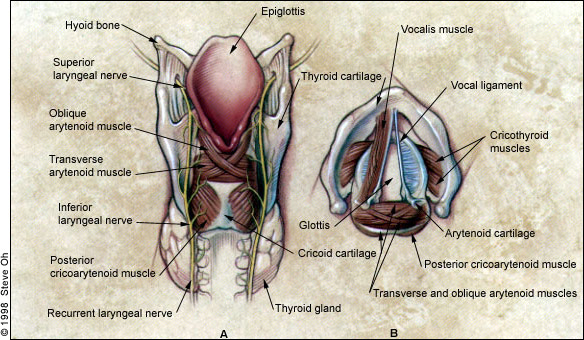
The larynx consists of four basic anatomic components: a cartilaginous skeleton, intrinsic and extrinsic muscles, and a mucosal lining1 (Figures 1 and 2). The cartilaginous skeleton, which houses the vocal cords (the thyroarytenoid muscles), is composed of the thyroid, cricoid and arytenoid cartilages. These cartilages are connected with other structures of the head and neck through the extrinsic muscles. The intrinsic muscles of the larynx alter the position, shape and tension of the vocal cords. An important consideration, therefore, is the innervation of these muscles and the characteristic features of lesions of these nerves.
The vagus nerve innervates the larynx through its branches, the superior laryngeal nerve and the recurrent laryngeal nerve (Figure 3). The superior laryngeal nerve supplies sensation to the epiglottis and false vocal cords, as well as motor function to the cricothyroid muscle (which serves to tense the vocal cord). A loss of the ability to sing high notes or to change pitch easily, or loss of sensation in the larynx and pharynx, therefore, may be caused by a lesion affecting the superior laryngeal nerve.
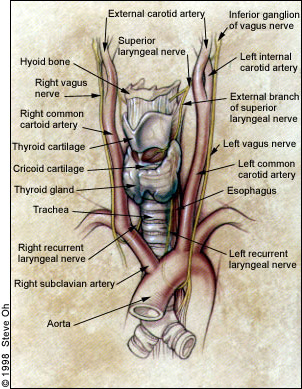
With the exception of the cricothyroid, all of the intrinsic muscles of the larynx are innervated by the recurrent laryngeal nerve. An important anatomic consideration is the location of the left and right branches of the recurrent laryngeal nerve; after leaving the vagus, the right recurrent laryngeal nerve loops around the subclavian artery, while the left recurrent laryngeal nerve loops around the arch of the aorta. Both branches travel cephalad into the neck in the tracheoesophageal groove and then enter the larynx. A mass lesion anywhere along the course of the nerve may result in paralysis of the vocal cord. Diseases of the brain stem, the neck and the mediastinum must, therefore, be included in the evaluation of dysphonia resulting from vocal cord paralysis. Surgical injury or penetrating trauma to these areas may also cause vocal cord paralysis (Table 3).
| Carotid surgery |
| Neck dissection for head and neck cancer |
| Cardiac surgery |
| Patent ductus ligation |
| Valve repair |
| Coronary artery bypass (rare) |
| Mediastinal surgery |
| Thymectomy |
| Mediastinoscopy |
| Esophagectomy |
| Thyroid surgery |
| Anterior cervical disc surgery |
| Tracheal surgery |
| Tracheal reconstruction |
| Tracheotomy (rare) |
The larynx functions in deglutition, respiration and phonation. Voice production can be thought of in terms of three components: generation of airflow, vocal cord vibration that produces sound and shaping of the sound to produce various resonances.2 The lips, tongue, teeth and palate provide the distinct sounds of speech. The lungs first supply adequate airflow to overcome the resistance of the adducted vocal cords. The vocal cords are finely tuned neuromuscular units that adjust pitch and tone by altering their position, length, tension and mass. Sound production occurs as a result of the vibration of the mucosa at the medial edge of each vocal cord. Thus, any structural, inflammatory or neoplastic lesion of the vocal cord affects voice production and quality. Final modification of speech occurs in the oropharynx and nasopharynx, where the tongue, palate, cheek and lips are involved in articulation. The integrated anatomy of voice production requires the physician to consider that a change in the anatomy or function of any of the structures involved in voice production, from the lungs to the nasopharynx, may result in dysphonia (Table 4).
| Neoplastic |
| Vocal cord polyp |
| Vocal cord nodules |
| Vocal cord granulomas |
| Vocal cord cyst |
| Laryngeal papilloma |
| Squamous cell cancer of the larynx |
| Inflammatory |
| Gastroesophageal reflux laryngitis |
| Viral laryngitis |
| Bacterial laryngitis |
| Tubercular or fungal laryngitis |
| Allergic laryngitis |
| Neurologic |
| Vocal cord paralysis (unilateral) |
| Spasmodic dysphonia |
| Movement disorder (i.e., Parkinson's disease) |
| Essential tremor |
| Cerebrovascular accident |
| Miscellaneous |
| Vocal abuse |
| Vocal cord atrophy |
| Vocal cord scarring |
| Hypothyroidism (myxedematous laryngitis) |
| Muscle tension dysphonia |
| Reinke's edema |
| Medications |
Evaluation of Hoarseness
History
In the absence of an upper respiratory tract infection, any patient with hoarseness persisting for more than two weeks requires evaluation. The history can yield important information for narrowing the differential diagnosis. In any patient with hoarseness and a history of tobacco use, head and neck cancer is the first diagnosis to consider, as hoarseness is often the only presenting symptom.
An essential part of a thorough history is elucidating the patient's voice use pattern. This process includes an evaluation of the patient's “vocal personality type” (amount and style of voice use), recent voice use (such as screaming at a baseball game) and vocal environment (where the patient uses his or her voice—such as talking while wearing earmuffs on an assembly line). A history of hearing loss in the patient or in a family member may be a contributing factor in voice abuse. This abuse is a common, often preventable, cause of dysphonia and may be underestimated by the patient, so it is important to question the patient and family members specifically about patterns of voice use.
A patient to consider in a special way is the professional voice user—anyone, from teachers to professional singers, whose occupation or livelihood depends on the normal use of the voice. These persons need earlier and more aggressive intervention and often require more specialized care.
Other aspects of the history include the nature and timing of the dysphonia; associated symptoms such as pain, dysphagia, cough or shortness of breath; symptoms of gastroesophageal reflux, such as an acid taste in the mouth in the morning; associated sinonasal diseases (allergic rhinitis or chronic sinusitis) and use of medications that dry the upper airway mucosa. Tobacco and ethanol use must be determined, as these products are irritating to the oral and laryngeal mucosa, and use of either is a risk factor for head and neck cancer. A history of other irritant exposure, particularly in the workplace, should be obtained. The patient should also be questioned about previous surgery on the head and neck or other surgery requiring intubation.
Physical Examination
A thorough head and neck examination, including assessment of hearing acuity, upper airway mucosa, tongue mobility and cranial nerve function, is essential in the evaluation of dysphonia. Visualization of the larynx, using either indirect laryngoscopy, flexible nasolaryngoscopy or strobovideolaryngoscopy, is central to the evaluation. The physician looks for lesions, erythema or edema of the mucosa and assesses vocal cord motion. It is essential to visualize the entire larynx. If clinical suspicion is high, the patient should also be examined for signs of systemic disease such as hypothyroidism, or neurologic dysfunction, such as tremor, Parkinson's disease or multiple sclerosis (Table 4).
Strobovideolaryngoscopy
The vocal cords typically vibrate during speech, singing or humming at a rate of 80 to 400 times per second. These vibrations are too fast for the unaided eye to see and, therefore, cannot be completely evaluated with indirect mirror laryngoscopy. Stroboscopy may be used to evaluate vocal cord vibrations. Stroboscopy allows the examiner to view the vocal cords in slow motion. Strobovideolaryngoscopy is done using a 70 degree rigid telescope or a flexible nasopharyngoscope.
Vocal cord vibration involves high-speed, minute vibrations; thus, a subtle change in the muscosa or tension of the vocal cord—that results in hoarseness—may be observed. Strobovideolaryngoscopy is especially important in the evaluation of subtle lesions affecting the vibration of the cords. This mode allows for the discovery of small lesions such as a vocal cord scar, hemorrhage or cyst.
Illustrative Cases
Illustrative Case 1
A 50-year-old overweight salesman presented with a three-month history of hoarseness, which he stated was worse in the morning. He also reported a sour taste in his mouth when awakening and described episodes of “choking on fluid” in his throat during his sleep. He denied heartburn or any symptoms of gastrointestinal distress during the day. He had smoked two packs of cigarettes per day for many years and had received a promotion to a more stressful position a few months before.
Visualization of his larynx revealed edema and erythema of the posterior larynx and swelling of his vocal cords. Vocal cord motion was normal, and no focal mucosal lesions were seen. He was diagnosed with reflux laryngitis. Treatment strategies included decreasing caffeine intake, discontinuing late night eating, and sleeping with the head of the bed elevated. The patient was also taught to decrease coughing and throat-clearing behaviors. A proton pump inhibitor was prescribed. The patient noticed a significant improvement in hoarseness within two weeks and complete resolution by six weeks.
Discussion. Reflux laryngitis often causes vague symptoms and is often not associated with the classic symptoms of gastroesophageal reflux, such as “heartburn.” This condition has recently been found to be highly prevalent, with a previously unrecognized effect on the larynx and pharynx.3 More aggressive treatment (i.e., high-dose histamine H2-receptor blockers or proton pump inhibitors) may be needed for reflux laryngitis than for reflux associated with esophagitis.
Illustrative Case 2
A 24-year-old woman complained of a three-month history of hoarseness following weekly choir practice. She was not a smoker and did not drink alcohol. She had no formal vocal training and several months before started singing solos with a choir.
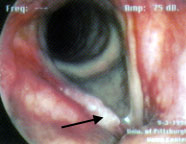
Examination revealed bilateral smooth swellings on her vocal cords at the junction of the anterior one third and the posterior two thirds of her vocal cords (Figure 4). Vocal nodules were diagnosed, and the patient was treated with voice therapy, which included a total of 10 sessions in six weeks. Re-evaluation after voice therapy found complete resolution of the patient's hoarseness and of the vocal nodules.

Discussion. Vocal nodules are common in children and adult women. These nodules are actually epithelial thickenings of the medial surface of the vocal cord, similar to callouses. A history of voice abuse or misuse can usually be elucidated.4,5 Voice therapy, the cornerstone of treatment, is usually effective within 12 weeks. If it is not effective, typically either the patient has been noncompliant, or the voice therapy is not being administered correctly. These patients rarely require surgery.
Illustrative Case 3
A 67-year-old man reported the recent onset of hoarseness and easy fatigability of his voice. He also stated that he had difficulty being heard in a crowd and complained of the recent onset of coughing that was most noticeable when drinking liquids. He had been a heavy smoker for many years.
The patient's speech was breathy, and he was unable to speak loudly or project his voice. When asked to swallow water, he aspirated a small amount.
Examination revealed paralysis of the left vocal cord (Figure 5). Chest radiograph revealed a solitary, 3-cm peripheral lesion in the left lung field and mediastinal adenopathy. He was diagnosed with adenocarcinoma of the lung and a left recurrent laryngeal nerve paralysis secondary to mediastinal adenopathy.

After voice therapy and medialization laryngoplasty6 (a procedure that medializes the paralyzed vocal cord using a silastic implant), the patient experienced dramatic improvement in both voice and swallowing.
Discussion. Patients with unilateral vocal cord paralysis typically present with a breathy, weak voice caused by incomplete adduction of the paralyzed vocal cord. A unilateral vocal cord paralysis can occur as a result of a lesion anywhere along the path of the vagus or recurrent laryngeal nerve, and the evaluation of this condition may necessitate imaging from the base of the skull to the level of the arch of the aorta. Other etiologies include injury of the recurrent laryngeal nerve during thyroid surgery, carotid endarterectomy, anterior cervical laminectomy, thoracic surgery or cervical trauma.7 Speech therapy and surgery aimed at medializing the paralyzed vocal cord (medialization laryngoplasty) are the primary treatment options after identifying and treating the etiology of the paralysis.
Illustrative Case 4
A 45-year-old woman stated that over the past month her voice had begun to tire more easily and she had begun to have pain with speaking at the end of the day. She also noted that her voice had been sounding “rough” lately. She expressed concern that these vocal changes were affecting her work as a salesperson.
Examination revealed muscle tension in the patient's strap muscles. Laryngeal examination revealed abnormal medialization of the false vocal cords and a squeezing of the larynx in an anterior-posterior direction during phonation. Muscle tension dysphonia was diagnosed and, after six weeks of voice therapy in which she learned effective laryngeal relaxation techniques, the patient reported return of normal vocal quality and effort.
Discussion. Muscle tension dysphonia is a condition of muscle strain and misuse in the larynx and neck that usually occurs in patients who use their voices extensively as part of their work—teachers, attorneys and sales personnel, for example. The generalized increase in muscular tension has several interacting causes, including poor vocal technique, extraordinary voice-use demands and psychologic factors such as anxiety.8 Vocal fatigue and discomfort are common presenting symptoms in patients with muscle tension dysphonia.
Illustrative Case 5
A 35-year-old man who smoked one pack per day and drank two to three beers per week reported a one-month history of hoarseness. He denied symptoms of airway compromise, dysphagia or throat pain.
On laryngeal examination he was found to have an irregular exophytic lesion of the mid-portion of his right true vocal cord (Figure 6). His vocal cords demonstrated normal mobility, and neck examination revealed no masses. The patient underwent direct laryngoscopy and biopsy, and a diagnosis of squamous cell carcinoma, stage T1, was made on the basis of those findings.
The patient underwent surgical excision of the lesion and has remained tumor-free after five years.
Discussion. Any adult patient with hoarseness and a history of tobacco use may have a laryngeal malignancy. Alcohol use increases the risk of head and neck malignancy in smokers. Glottic lesions are the most common laryngeal cancers and usually present early with hoarseness. Later presentations may include throat irritation, hemoptysis, dysphagia or referred otalgia. Surgery or radiation therapy are the primary treatment options, depending on the stage of the tumor at diagnosis.9–11 Laryngeal cancer may have a 90 to 95 percent cure rate when detected early.
Prevention of Hoarseness
Vocal Hygiene
An integral aspect of the prevention of vocal pathology is the maintenance of good vocal hygiene. Patients should be advised to avoid straining their voices by shouting, whispering or attempting to talk over excessive background noise. The importance of hydration should be emphasized. Certain medications, such as antihistamines and drugs that dry the mucosa through anticholinergic side effects (such as tricyclic antidepressants), may also create unfavorable voice changes, and these drugs should be avoided if possible. Irritants such as tobacco, alcohol, marijuana and industrial chemicals should be avoided.
Table 5 outlines ways to avoid and ease vocal abuse. Patients with hoarseness lasting more than two weeks, pain occurring with speech or swallowing, or a foreign-body sensation in the throat should be examined.
| Things to do |
| Get plenty of rest |
| Drink plenty of water—eight glasses per day |
| Things to avoid |
| Breathing foul air |
| Using tobacco or marijuana |
| Using drugs |
| Drinking alcohol |
| Shouting at sporting events |
| Trying to be heard in noisy places like bars or airports |
| Making sounds while yawning |
| Clearing throat continually |
| Trying to talk over a cold or laryngitis |
| Whispering loudly or for very long |
| Trying to change natural speaking voice |
Voice Therapy
Voice therapy includes four major components—vocal hygiene, vocal production, muscle relaxation and respiratory support—in addition to education about the vocal mechanism. Vocal hygiene includes the establishment of healthy attitudes about use and treatment of the voice mechanism, similar to a dental hygiene program. Vocal production includes the analysis and alteration of speaking pitch, loudness and voice quality, using listening and feeling techniques, and postures. Respiratory support and muscle relaxation involve posture, timing of respiration-phonation coordination and respiratory effort using relaxed upper thoracic muscles. Education helps the patient understand the goals of correcting the vocal mechanism.
Voice therapy is a behavior-based process in which maladaptive vocal habits and techniques are replaced with appropriate uses of the vocal mechanism. The treatment process incorporates auditory, visual and proprioceptive feedback channels to produce a healthy and efficient voice. Voice therapy is typically administered six to 14 times (in 30- to 40-minute sessions) over a six- to eight-week period. Following therapy, examination of the larynx and documentation of improvement are routine.