
A more recent article on diagnosis and management of hip fractures is available.
Am Fam Physician. 2003;67(3):537-543
Patients with hip fracture typically present to the emergency department or their physician's office after a fall. They are often unable to walk, and they may exhibit shortening and external rotation of the affected limb. Frequently, they have hip pain. In some instances, however, patients with hip fracture may complain only of vague pain in their buttocks, knees, thighs, groin, or back. Their ability to walk may be unaffected, and initial radiographic findings may be indeterminate. In these patients, additional studies, such as magnetic resonance imaging or bone scanning, may be necessary to confirm the presence of hip fracture. A high index of suspicion often is required for prompt diagnosis and treatment of an occult hip fracture. Even when a patient is able to walk and has no documented trauma, localized hip pain, or typical shortening and malrotation deformity, the family physician should be alert to the possibility of hip fracture, particularly in a patient who is older than 65 years, presents with nonspecific leg discomfort, and complains of difficulty bearing weight on the affected limb. A heightened suspicion for hip fracture should lead to further diagnostic evaluation, especially if the patient has additional risk factors, such as use of a complicated drug regimen, impaired vision, physical or neurologic impairment, or comorbid condition (e.g., osteoporosis, malignancy). When hip fracture is detected early, appropriate treatment can minimize morbidity and mortality and prevent the rapid decline in quality of life that often is associated with this injury.
Hip fracture is a major public health problem in the United States.1–3 It results in hospitalization, disability, and loss of independence for an estimated 300,000 persons annually in this country.2,4 In 1995 alone, medical treatment for this injury, including inpatient care, nursing home care, and outpatient services, cost an estimated $8.68 billion.2 With the aging of the U.S. population, the number of hip fractures is expected to increase in the near future.1,2,5
Delayed recognition of hip fracture can result in increased morbidity and mortality, as well as a rapid decline in quality of life. One-year mortality rates after this injury range from 15 to 20 percent.1,2,6,7 Approximately 50 percent of patients who lived independently before sustaining a hip fracture are unable to regain their independent lifestyle; instead, they face ongoing disability and prolonged institutionalization.2,3 Given these serious consequences, it is vital to detect and appropriately treat patients with hip fracture.
Illustrative Case
A 75-year-old woman presented to her family physician with persistent left buttock pain for several weeks. Staff at the patient's assisted living facility had noted that in recent weeks she had occasionally limped when walking from her bed to the bathroom. However, she remained able to shower, dress herself, and walk to the main dining room and garden.
On careful review of the patient's history, the physician determined that a fall had not taken place. Aside from mild Alzheimer's disease, the patient was in good health. Other than the slight limp, her physical examination was normal.
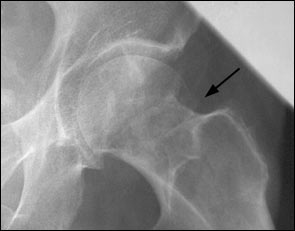

The patient subsequently underwent open reduction and internal fixation of the fracture. She had an uncomplicated postoperative course and returned to the assisted living facility.
Clinical Presentation of Hip Fracture
The typical patient with hip fracture is often an elderly woman with dementia who sustains a fall, may complain of severe hip pain, and is unable to walk. The physical examination commonly reveals an abducted and externally rotated hip with leg-length discrepancy. The patient usually has localized tenderness over the hip and limited range of motion of the affected limb during attempts at passive and active rotation and flexion. Radiographs clearly demonstrate the fracture.
In some instances, however, patients with hip fracture have normal ambulation and complain only of vague pain in their buttocks, knees, thighs, groin, or back. These patients frequently report no antecedent trauma, particularly if cognitive impairment is present. Their physical examination, including assessments of active, passive, and resisted movements of the affected hip joint and limb, may be normal. They often have additional injuries (e.g., scalp lacerations, knee sprains, or other impairments) that mask the hip pathology and direct the physician's attention away from the diagnosis of hip fracture.
Diagnostic Imaging
The diagnosis of hip fracture can usually be established with a detailed history, a thorough physical examination, and plain-film radiographs of the symptomatic hip. If radiographic findings are indeterminate but suspicious for a hip fracture, other imaging modalities can be useful in confirming the diagnosis.
Various nonrandomized, observational studies have shown that bone scanning of the hip using technetium Tc 99m polyphosphate as the radiopharmaceutical can be up to 98 percent sensitive in confirming the presence of hip fracture when initial radiographic findings are normal or indeterminate.8–10 The current recommendation is to delay scanning for up to 72 hours to optimize the chance of detecting the fracture.11 [Evidence level C, consensus/expert guidelines] In such cases, patients may be admitted to the hospital, treated with bed rest, and reevaluated in two to three days.
Various studies also have demonstrated the efficacy of MRI in diagnosing hip fractures.12–19 One prospective study showed that coronal T1-weighted hip MRI was 100 percent sensitive in confirming the presence of hip fracture in patients with indeterminate findings on initial plain-film radiographs.17 [Evidence level B, nonrandomized study] The authors of the study concluded that MRI is more accurate and probably less expensive than other imaging alternatives (i.e., bone scanning and computed tomographic [CT] scanning), especially if consideration is given to the fact that earlier detection results in faster recovery and shorter hospital stays. In this study, the estimated total charges were $448 for MRI, $455 for bone scanning, and $797 for CT scanning.
Other cited advantages of MRI over bone scanning or CT scanning include its ability to detect fractures within 24 hours and its noninvasive nature (i.e., no exposure to ionizing radiation).11,14 The decision to use bone scanning or MRI largely depends on the availability of these technologies at a given medical facility and the preference of the treating physician. If these resources are not available, the physician should confer with an orthopedic surgeon to decide which imaging modalities should be used.
Differential Diagnosis
The differential diagnosis of hip or leg pain is extensive. Therefore, a thorough history and careful physical examination are crucial in determining the underlying cause. Because certain types of hip fracture are associated with an increased risk of avascular necrosis of the femoral head, hip pain subsequent to major trauma should be considered indicative of hip fracture until proved otherwise.20,21
Other lower body fractures must be excluded. For example, fractures of the acetabulum and pubic ramus or stress fractures may present with signs and symptoms similar to those of a hip fracture. In particular, patients with stress fractures may present with little or no history of trauma.8,11 Symptoms that suggest a stress fracture include limping and hip or leg pain that is generally worse at night. Stress fractures are often associated with comorbid conditions such as malnutrition, gait impairment, and mechanical overuse.11,20 In the elderly, stress fractures are often caused by osteopenic bone or pathologic conditions such as malignancy.11,20
Once the diagnosis of hip or other lower body fracture has been ruled out, more common but chronic sources of hip or leg pain should be considered. Osteoarthritis remains one of the most frequent causes of hip or leg pain in patients older than 50 years.22 Classic symptoms include limping and hip pain that progressively worsen over time. Plain-film radiographs are generally sufficient to diagnose the narrowing of the joint space that occurs with osteoarthritis. Other acute and chronic diagnostic possibilities are listed in Table 1.11,20,22
| Source of pain | Diagnosis |
|---|---|
| Bone | Fracture, avascular necrosis of the femoral head, primary neoplasm, metastatic disease |
| Joint | Osteoarthritis, inflammatory arthritis, septic arthritis, crystalloid arthritis, osteoid osteoma, osteitis pubis, acetabular tear |
| Muscle, tendon, bursa | Contusion, iliotibial band syndrome, muscle strain, tendonitis, trochanteric bursitis, iliopsoas bursitis, pyriformis syndrome, myositis ossificans |
| Spine, neuropathic source | Disorders of the lumbar disc, lumbar spinal stenosis, sciatica, coccygodynia, meralgia paresthetica |
| Others | Hernia, abdominal pathology, pelvic pathology, referred pain from knee, ankle, or foot |
Classification and Treatment of Hip Fractures
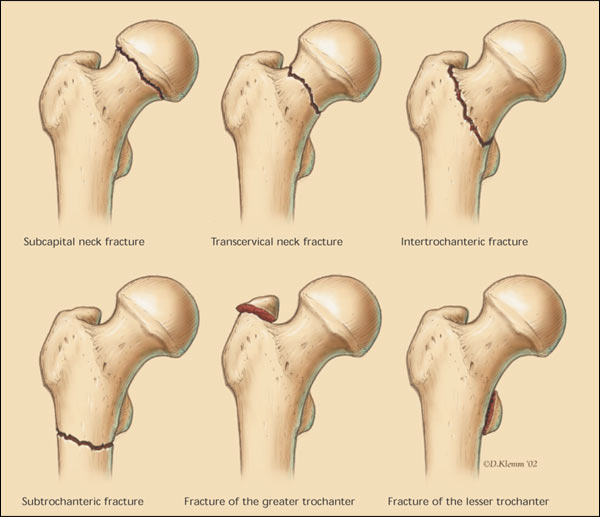
Hip fractures are usually classified according to anatomic location (Table 220,21,23 and Figure 3). They are typically identified as intracapsular (femoral neck fracture) or extracapsular (intertrochanteric or subtrochanteric fracture). These fractures are also classified according to severity and degree of stability24; the Garden classification is an example20,21 (Table 3).25,26
| Fracture type | Frequency | Potential complications | |
|---|---|---|---|
| Intracapsular fracture | |||
| Femoral neck | 45 percent in the elderly; male-to-female ratio: 1:3 | Avascular necrosis of the femoral head, nonunion or malunion, late degenerative changes | |
| Extracapsular fracture | |||
| Intertrochanteric | 45 percent in the elderly; male-to-female ratio: 1:3 | Rarely, nonunion or malunion; degenerative changes | |
| Subtrochanteric | 10 percent, with bimodal distribution (i.e., persons 20 to 40 years of age and persons more than 60 years of age) | High rates of nonunion and implant (i.e., intramedullary nails or devices); fatigue because of high physical stresses in the region | |
| Type 1: Valgus impaction of the femoral head |
| Type 2: Complete but nondisplaced fracture |
| Type 3: Varus displacement of the femoral head |
| Type 4: Complete loss of continuity between both fragments |
The distinction between intracapsular and extracapsular fracture has prognostic value. For example, early detection of intracapsular fractures is especially important, because these fractures are prone to complications for two primary reasons. First, disruption of the blood supply to the femoral head frequently occurs and can lead to avascular necrosis. Second, the head fragment of the fracture is often a shell containing fragile cancellous bone that provides poor anchorage for a fixation device, a situation that often increases the possibility of nonunion or malunion.20,21,27
Most patients with hip fracture require surgical reduction and internal fixation. However, the choice of surgical procedure depends on the type of fracture, the preference of the orthopedic surgeon, the severity of the injury, the age of the patient, the presence or absence of comorbid conditions (e.g., osteoporosis, hip joint osteoarthritis), and the prognosis for recovery during rehabilitation.21 For example, extracapsular intertrochanteric fractures are typically repaired with surgical reduction and internal fixation. In contrast, treatments for intracapsular femoral neck fractures vary from internal fixation to hemiarthroplasty to total hip replacement, depending on the severity of the fracture, the stability of the joint, the patient's condition, and the surgeon's preference.21,27
Measures for Preventing Hip Fracture
| Calcium supplementation (1,000 to 1,500 mg per day) |
| Vitamin D supplementation (400 to 800 IU per day) |
| Bisphosphonates (e.g., alendronate [Fosamax], risedronate [Actonel]) |
| Selective estrogen receptor modulators (e.g., raloxifene [Evista]) |
| Calcitonin |
| Regular physical activity (e.g., weight-bearing and muscle-strengthening exercises) |
| Reduction of modifiable risk factors (e.g., smoking cessation, alcohol abstinence) |
| Fall prevention (e.g., use of assistive devices, home safety practices, physical therapy for gait stabilization) |
| Anabolic steroids, pulsatile growth hormone, or parathyroid hormone therapy (experimental) |
Osteoporosis is probably the most important disease associated with hip fracture. Prevention of this disease is crucial to reducing the risk of hip fracture, especially in postmenopausal women.6,28,29 Family physicians should maintain a high index of suspicion for osteoporosis in postmenopausal women with multiple risk factors, screening for (e.g., bone density testing) and treating the disease when indicated.28
Regardless of risk factors and if no contraindications exist, all patients should be encouraged to take appropriate doses of calcium (1,000 to 1,500 mg per day) and vitamin D (400 to 800 IU per day), and to engage in weight-bearing, and muscle-strengthening exercises.6,28 [References 6 and 28—Evidence level C, consensus/expert guidelines] Other useful interventions to decrease the risk of osteoporosis and subsequent hip fracture include bisphosphonates or selective estrogen receptor modulators, smoking cessation, moderation of alcohol use, simplification of drug regimens, gait stabilization therapy, and the use of assistive devices to prevent falls.28,29,31 [References 29 and 31—Evidence level C, consensus/expert guidelines]
Although hormone replacement therapy has been used for osteoporosis prevention, recent results from the Women's Health Initiative (WHI) trial32 demonstrated that overall health risks exceeded the benefits of using combined estrogen plus progestin for an average follow-up period of 5.2 years in healthy postmenopausal women in the United States. The WHI findings indicated that the estrogen-progestin combination is not a viable intervention for primary prevention of chronic diseases. Results from the estrogen-only arm of the WHI trial are pending.