
A more recent article on injections of the hip and knee is available.
Am Fam Physician. 2003;67(10):2147-2152
Joint injection of the hip and knee regions is a useful diagnostic and therapeutic tool for the family physician. In this article, the injection procedure for the greater trochanteric bursa, the knee joint, the pes anserine bursa, the iliotibial band, and the prepatellar bursa is reviewed. Indications for greater trochanteric bursa injection include acute and chronic inflammation associated with osteoarthritis, rheumatoid arthritis, repetitive use, and other traumatic injuries to the area. For the knee joint, aspiration may be performed to aid in the diagnosis of an unexplained effusion and relieve discomfort caused by an effusion. Injection of the knee can be performed for viscosupplementation or corticosteroid therapy. Indications for corticosteroid injection include advanced osteoarthritis and other inflammatory arthritides, such as gout or calcium pyrophosphate deposition disease. Swelling and tenderness of pes anserine or prepatellar bursae can be relieved with aspiration and corticosteroid injection. Persistent pain and disability from iliotibial band syndrome respond to local injection therapy. The proper technique, choice and quantity of pharmaceuticals, and appropriate follow-up are essential for effective outcomes.
This article, part of a series on diagnostic and therapeutic injections, reviews the hip and knee regions. The rationale, indications, contraindications, and general approach to this technique are discussed in the first article of the series.1 The hip and knee are sites of multiple injuries and inflammatory conditions2 that lend themselves to diagnostic and therapeutic injection.3–8 Intra-articular injection of the hip is rarely performed by family physicians because this procedure is commonly performed with fluoroscopic guidance. This article focuses on the anatomy, pathology, diagnosis, and injection technique of the common sites for which this skill is applicable, including the greater trochanteric bursa, knee joint, pes anserine bursa, iliotibial band, and the prepatellar bursa.
Greater Trochanteric Bursa
ANATOMY
The trochanteric bursa is located over the lateral prominence of the greater trochanter of the femur.
INDICATIONS
Trochanteric bursitis, the primary indication for therapeutic injection at this site, usually is associated with chronic pressure or trauma to the area. Leg-length abnormalities, obesity, rheumatoid arthritis, and osteoarthritis are associated factors in many patients.9 Friction from a tight iliotibial band, typically seen in runners, also can cause this problem. Diagnosis is confirmed by palpation of tenderness, and sometimes swelling, in the region of the bursa.
TIMING AND OTHER CONSIDERATIONS
Early corticosteroid injection frequently is the preferred treatment, because it has been shown to be effective with satisfactory duration of effect.10
TECHNIQUE
See Table 1 for a list of pharmaceuticals and equipment.
Position of Patient
The patient should be in the lateral recumbent position with the affected side up. For the patient's comfort and stabilization, the hip is flexed 30 to 50 degrees and the knee is flexed 60 to 90 degrees.
| Site | Syringe | Needle | Anesthetic | Corticosteroid* | Hydrocortisone equivalents per injection | |
|---|---|---|---|---|---|---|
| Greater trochanteric bursa | 5 to 10 mL | 22 or 25 gauge, 1.5 inch (longer if patient is very obese) | 3 to 5 mL of 1 percent lidocaine (Xylocaine) or 0.25 or 0.5 percent bupivacaine (Marcaine) | 1 mL betamethasone sodium phosphate and acetate (Celestone Soluspan) | 150 | |
| or | ||||||
| 1 mL methylprednisolone (Depo-Medrol), 40 mg per mL | 200 | |||||
| Knee joint | 30 to 60 mL (for aspiration), 10 mL (for injection) | 18, 20, or 22 gauge 1.5 inch† | 5 to 7 mL of 1 percent lidocaine or 0.25 or 0.5 percent bupivacaine | 2 to 3 mL betamethasone sodium phosphate and acetate | 300 to 450 | |
| or | ||||||
| 2 to 3 mL methylprednisolone, 40 mg per mL | 400 to 600 | |||||
| Pes anserine bursa | 5 mL | 25 gauge, 1 inch | 2 mL of 1 percent lidocaine or 0.25 or 0.5 percent bupivacaine | 1 mL betamethasone sodium phosphate and acetate | 150 | |
| or | ||||||
| 1 mL methylprednisolone, 40 mg per mL | 200 | |||||
| Iliotibial band | 5 mL | 25 gauge, 1 inch | 1 to 2 mL of 1 percent lidocaine or 0.25 or 0.5 percent bupivacaine | 1 mL betamethasone sodium phosphate and acetate | 150 | |
| or | ||||||
| 1 mL methylprednisolone, 40 mg per mL | 200 | |||||
| Prepatellar bursa | 20 to 30 mL (for aspiration), 5 to 10 mL (for injection) | 18 or 22 gauge, 1 or 1.5 inch† | 2 mL of 1 percent lidocaine or 0.25 or 0.5 percent bupivacaine | 1 mL betamethasone sodium phosphate and acetate | 150 | |
| or | ||||||
| 1 mL methylprednisolone, 40 mg per mL | 200 | |||||
Palpation of Landmarks
The greater trochanter is identified by palpating the femur from the mid-shaft proximally until the area of bony protrusion is reached. The injection site is the point of maximal tenderness or swelling.
Approach and Needle Entry
At the area most tender or swollen to palpation in the region of the greater trochanter, a 22- or 25-gauge, one and one-half–inch needle is inserted perpendicular to the skin (Figure 1). In very obese patients, a longer needle may be required. The needle should be inserted directly down to bone and then withdrawn two to three millimeters before injecting.

Knee Joint
ANATOMY
Two functional joints, the femoral-tibial and the femoral-patellar, make up the knee. Primary stabilizers of the knee are the anterior and posterior cruciate ligaments, the medial and lateral collateral ligaments, and the capsular ligaments.
INDICATIONS
Indications for aspiration include unexplained effusion, possible septic arthritis, and relief of discomfort caused by an effusion.11 Indications for injection include corticosteroid delivery for advanced osteoarthritis and other noninfectious inflammatory arthritides such as gout or calcium pyrophosphate deposition disease, or the delivery of viscosupplementation therapy.12–14 Viscosupplementation preparations such as hylan G-F 20 (Synvisc) come with prefilled syringes and are used to treat the pain of knee joint osteoarthritis. Viscosupplementation and corticosteroid therapies are not used concomitantly.
TIMING AND OTHER CONSIDERATIONS
The use of intra-articular corticosteroids is reserved for patients with more advanced disease and after other modalities have been tried. Aspiration for suspected septic arthritis must be performed immediately.
TECHNIQUE
See Table 1 for a list of pharmaceuticals and equipment.
Position of Patient
The patient is in the supine position with the knee slightly flexed with a pillow or rolled towel in the popliteal space.
Palpation of Landmarks
Identify the medial, lateral, and superior borders of the patella.
Approach and Needle Entry
There are many different techniques for aspirating or injecting the knee. These include medial, lateral, and anterior approaches. Each has its own merit, but choice of approach is dependent on physician preference. The lateral approach is most commonly used and is illustrated here (Figure 2). For this approach, lines are drawn along the lateral and proximal borders of the patella. The needle is inserted into the soft tissue between the patella and femur near the intersection point of the lines, and directed at a 45-degree angle toward the middle of the medial side of the joint. Before injection or aspiration, local anesthesia with lidocaine (Xylocaine) should be obtained. Always use sterile technique. Intra-articular injection flow should be even and without resistance.

For the medial approach, the needle enters the medial side of the knee under the middle of the patella (midpole) and is directed toward the opposite patellar midpole. In the anterior approach, the knee is flexed 60 to 90 degrees, and the needle is inserted just medial or lateral to the patellar tendon and parallel to the tibial plateau. This technique is preferred by some physicians for its ease of joint entry in advanced osteoarthritis. However, the anterior approach may incur greater risk for meniscal injury by the needle.

Pes Anserine Bursa
ANATOMY
The pes anserine bursa is located between the medial collateral ligament and the sartorius, gracilis, and semitendinosus tendons. The bursa is located distal to the joint line in close proximity and posterior to the medial collateral ligament.
INDICATIONS
Direct trauma or repeated friction over the bursa can lead to inflammation. When the bursa is inflamed, contraction of the hamstring muscles, rotational movements of the tibia, and direct pressure over the pes anserine bursa usually will produce pain. The pain is in the posterior medial aspect of the knee distal to the joint space. This condition is more commonly seen in middle-aged or older overweight women, many with osteoarthritis of the knee.15
TIMING AND OTHER CONSIDERATIONS
Injection in this condition often is performed early in the course of treatment rather than after a trial of other modalities.
TECHNIQUE
See Table 1 for a list of pharmaceuticals and equipment.
Position of Patient
The patient is in the supine position with the knee slightly flexed.
Palpation of Landmarks
Identify the tendinous border of the medial thigh muscles and follow them across the joint line to their insertion at the pes anserine.
Approach and Needle Entry
The needle is inserted perpendicular to the tibia into the point of maximal tenderness (Figure 3). The needle is gently guided down to the bone and then withdrawn two to three millimeters to perform the injection.
Iliotibial Band
ANATOMY
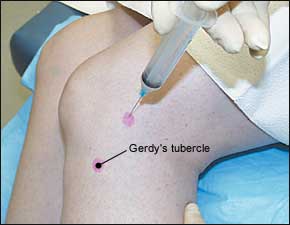
The iliotibial band originates at the lateral iliac crest and inserts on the lateral proximal tibia. Gerdy's tubercle (sometimes called the lateral tubercle of the tibia) is a prominence of the anterior surface of the lateral condyle and is easily palpated just lateral to the distal portion of the patellar tendon.
INDICATIONS
Iliotibial band syndrome is a disorder of pain and degenerative changes that occurs as the iliotibial band repeatedly rubs over the prominence of the lateral femoral condyle. It is seen in activities with repetitive flexion and extension of the knee, such as running.16–19 Diagnosis is made by elicitation of tenderness over Gerdy's tubercle or the lateral femoral condyle. Ober's test is performed with the patient lying on the unaffected side. The affected hip is abducted against gravity, and the knee is flexed to 90 degrees with the knee and distal leg supported by the examiner's forearm and hand. The knee is then released. In a contracted iliotibial band, the knee does not drop with gravity.
TIMING AND OTHER CONSIDERATIONS
TECHNIQUE
See Table 1 for a list of pharmaceuticals and equipment.
Position of Patient
The patient is placed in the lateral recumbent position with the knee flexed 20 to 30 degrees.
Palpation of Landmarks
Along the lateral thigh, follow the course of the iliotibial band across the femoral condyle to its insertion at Gerdy's tubercle.
Approach and Needle Entry
The needle is inserted at the point of maximal tenderness in the region of the lateral condyle (Figure 4).
Prepatellar Bursa
ANATOMY
The prepatellar bursa is located between the skin and the anterior surface of the patella, making it vulnerable to direct trauma.
INDICATIONS
Bursitis is manifested by swelling and tenderness anterior to the patella and can be the result of acute trauma.22,23 Chronic prepatellar bursitis is more common than an acute episode and usually is the result of repeated episodes of microtrauma.24 In the evaluation of a patient with prepatellar bursitis, the physician should be aware of possible underlying infection, fracture of the patella, or an associated intra-articular injury of the knee.25,26 Bursitis-related prepatellar swelling must be differentiated from an intra-articular effusion. Aspiration of an inflamed bursa can be performed for relief of discomfort associated with a bursitis. If the symptoms of prepatellar bursitis are recurrent, corticosteroid injection may be performed.
TIMING AND OTHER CONSIDERATIONS
Aspiration of the prepatellar bursa may be performed acutely for relief of swelling and discomfort. Corticosteroid injection can be performed in cases of chronic or persistent bursitis after a trial of more conservative therapy.
TECHNIQUE
See Table 1 for a list of pharmaceuticals and equipment.
Position of Patient
The patient is placed in the supine position with the knee resting in a comfortable position. A small pillow may be placed under the knee for comfort and support.
Palpation of Landmarks
The area over the patella is palpated for fluctuance.
Approach and Needle Entry
Aspiration and injection are performed by placing the needle directly into the fluid-filled bursa from the side (Figure 5). Before injection with a corticosteroid, fluid should be aspirated from the bursa. If injecting, a hemostat is used to hold the needle in place while changing the syringe.

Follow-Up
Following aspiration of the prepatellar bursa, a pressure dressing should be applied, and the patient should remain in the supine position for several minutes. Following injection, the joint or injected region may be put through passive range of motion. The patient should remain in the office for 30 minutes after the injection to monitor for any adverse reactions. In general, patients should avoid strenuous activity involving the injected region for several days. Patients should be cautioned that they may experience worsening symptoms during the first 24 to 48 hours related to a possible steroid flare, which can be treated with ice and nonsteroidal anti-inflammatory drugs. Patients should be instructed against the application of heat. A follow-up appointment should be scheduled within three weeks.