
Am Fam Physician. 2024;109(1):61-70
This is one of a series of articles produced in collaboration with the American Medical Society for Sports Medicine.
Author disclosure: No relevant financial relationships.
Hip and knee injections are useful diagnostic and therapeutic tools for family physicians. This article reviews anatomic landmark–guided and ultrasound-guided injections and aspiration techniques for greater trochanteric pain syndrome, the hip joint, the knee joint, the pes anserine bursa, and the iliotibial band. Indications for injections include acute and chronic inflammatory conditions, such as rheumatoid arthritis; osteoarthritis; overuse; and traumas. Joint aspirations may be performed to aid in the diagnosis of unexplained effusions and to relieve pain. Technique, injectant, and follow-up timing depend on the physician's comfort, experience, and preference. Infections of the skin or soft tissue are the primary contraindications to injections. The most common complications are local inflammatory reactions to the injectant. These reactions usually cause soreness for 24 to 48 hours, then spontaneously resolve. Follow-up after injections is usually scheduled within two to six weeks.
Family physicians often use joint injections for the diagnosis and treatment of common musculoskeletal conditions. This review discusses techniques using anatomic landmark–guided and ultrasound-guided injections and aspiration for the hip and knee; however, many other techniques are also available for injections. Family physicians are becoming more comfortable with the use of point-of-care ultrasonography (POCUS) for diagnosis and guided procedures; however, the terminology and techniques of POCUS are beyond the scope of this article. Intra-articular injections guided by POCUS are more accurate than anatomic landmark–guided injections of the hip and knee.1–10
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Intra-articular injections guided by point-of-care ultrasonography are more accurate than anatomic landmark–guided injections of the hip and knee.1–10 | C | Multiple cohort studies and case series |
| Intra-articular injections may be used as an adjunct for short and intermediate pain relief and improved function in patients with osteoarthritis of the hip and knee.11,12,15,21–25,29–31 | C | Expert opinion and consensus guidelines |
| Intra-articular corticosteroid injections may be used for the treatment of pain caused by osteoarthritis of the hip.2,12,14,15,18,22–24 | B | Cohort studies and systematic reviews demonstrating decreased morbidity |
| Intra-articular corticosteroid injections may be used for the treatment of pain caused by osteoarthritis of the knee.11,12,21–25,27,29–32,37,38 | B | Cohort studies and systematic reviews demonstrating decreased morbidity |
Table 1 provides commonly reported needle, steroid, and anesthetic combinations.11,12 Table 2 identifies common steroids and the duration of action.12 Table 3 reviews the approximate duration of onset and action for anesthetics.12 eTable A compares the accuracy rates of hip and knee injection techniques using landmark and ultrasound guidance. eTable B provides resources for learning about POCUS.
| Site | Type of needle | Steroid options | Anesthetic |
|---|---|---|---|
| Greater trochanter | 22 gauge, 1.5 or 3.5 inch (depending on the body habitus of the patient) | Betamethasone, 6 mg Dexamethasone, 8 mg Methylprednisolone, 40 mg Triamcinolone, 40 mg | 5 mL of lidocaine 1% or bupivacaine 0.25% or 0.5% |
| Hip joint | 22 gauge, 3.5 inch | Betamethasone, 6 mg Dexamethasone, 8 mg Methylprednisolone, 40 mg Triamcinolone, 40 mg | 3 mL of bupivacaine 0.25% or 0.5% |
| Knee joint | 21 or 22 gauge, 1.5 inch | Betamethasone, 6 mg Dexamethasone, 8 mg Methylprednisolone, 40 mg Triamcinolone, 40 mg | 5 to 7 mL of lidocaine 1% or bupivacaine 0.25% or 0.5% |
| Pes anserine bursa | 22 gauge, 1.5 inch | Betamethasone, 3 to 6 mg Dexamethasone, 4 to 8 mg Methylprednisolone, 20 to 40 mg Triamcinolone, 10 to 40 mg | 2 mL of lidocaine 1% or bupivacaine 0.25% or 0.5% |
| Iliotibial band | 22 gauge, 1.5 inch | Betamethasone, 3 to 6 mg Dexamethasone, 4 to 8 mg Methylprednisolone, 20 to 40 mg Triamcinolone, 10 to 40 mg | 2 mL of lidocaine 1% or bupivacaine 0.25% or 0.5% |
| Steroid | Approximate duration of action in days |
|---|---|
| Dexamethasone sodium | 6 |
| Dexamethasone acetate | 8 |
| Methylprednisolone acetate | 8 |
| Betamethasone acetate | 14 |
| Triamcinolone acetate | 14 |
| Triamcinolone hexacetonide | 21 |
| Anesthetic | Onset of action (minutes) | Duration of action (hours) | Maximum volume of injection (mL)* |
|---|---|---|---|
| Bupivacaine 0.25% | 30 | 8 | 60 |
| Bupivacaine 0.5% | 30 | 8 | 30 |
| Lidocaine 1% | 1 to 2 | 1 | 20 |
| Lidocaine 2% | 1 to 2 | 1 | 10 |
| Author | Type of study | Sample size | Accuracy of landmark-guided injections (%) | Accuracy of ultrasound-guided injections (%) |
|---|---|---|---|---|
| Hip joint | ||||
| Diraçoğlu, et al. | Cohort | 16 patients | 66.7 | — |
| Levi | Retrospective review | 11 patients | — | 100 |
| Pourbagher, et al. | Case series | 10 patients | — | 100 |
| Smith, et al. | Cohort | 28 patients | — | 97 |
| Ziv, et al. | Cohort | 40 patients | 77.5 | — |
| Knee joint | ||||
| Berkoff, et al. | Meta-analysis | 5 studies | 77.8 | 95.8 |
| Curtiss, et al. | Cohort | 20 patients | 55 (less experienced clinician) 100 (experienced clinician; superolateral) | 100 (any clinician; superolateral) |
| Daley, et al. | Systematic review | 11 studies | 70 (medial) 83 (superolateral) 84 (lateral midpatellar) | 99 (superolateral) |
| Esenyel, et al. | Cohort | 39 patients | 56 (medial midpatellar) 73 (anteromedial) 76 (lateral midpatellar) 85 (anterolateral) | — |
| Hermans, et al. | Systematic review | 9 studies | 67 (anterolateral) 72 (anteromedial) 85 (lateral midpatellar) 91 (superolateral) | — |
| Jackson, et al. | Cohort | 240 patients | 71 (anterolateral) 75 (anteromedial) 93 (lateral midpatellar) | — |
| Lopes, et al. | Case series | 37 patients | 100 (superolateral) | — |
| Resource | Cost | Comments |
|---|---|---|
| American College of Emergency Physicians Sonoguide https://www.acep.org/sonoguide | Free | Online curriculum of test-based descriptions with photos and videos; referenced by Ultrasound Ninja curriculum; developed for emergency department clinicians |
| American Institute of Ultrasound in Medicine https://www.aium.org | Prices vary by course and CME credits | Collection of CME materials for ultrasound certification; credentialing program recommending 50 credits in each body area; links to recent articles on point-of-care ultrasonography |
| American Medical Society for Sports Medicine https://www.amssm.org/Onlinelearning-CME.php https://www.amssm.org/US-Case-Studies.php | Free | Collection of short videos demonstrating examination of the musculoskeletal system and ultrasound-guided injections; library of case studies with teaching pearls |
| Core Ultrasound https://coreultrasound.com/5ms | Free | Collection of short videos demonstrating examinations; podcast; course for beginners, including an introduction to basic ultrasonography (fee required for courses) |
| Point-of-Care Ultrasound Certification Academy https://pocus.org | $125 for fundamental certification; $150 for each of 10 clinical area certificates; $625 for emergency medicine certification with seven clinical areas | Certification programs, including examination and certificate; collection of webinars, podcasts, and other clinical programs |
| SonoSpot: Topics in Bedside Ultrasound http://sonospot.com | Free | Tutorials with photos and verbal descriptions for probe placement; short videos of ultrasound images showing expected results |
| Ultrasound Ninja http://www.ultrasoundninja.com | Free | Emergency medicine ultrasound program; curriculum consisting of podcasts and references for each curricular element; free e-book |
Greater Trochanteric Pain Syndrome
Patients with tenderness to palpation over the greater trochanter may have greater trochanteric bursitis, gluteal tendinitis, or both. Greater trochanter pain syndrome presents with pain over the lateral hip around the greater trochanter that is worse with lying down on the affected side, passive stretching, and eccentric loading of the external rotators.13,14
ANATOMY
The greater trochanter of the femur comprises four facets. The gluteus minimus tendon attaches to the anterior facet. The gluteus medius tendon is comprised of anterior and posterior bands that attach to the lateral and superior posterior facets. The iliotibial band overlies the gluteus minimus and medius muscles. There are three bursas located in the greater trochanteric region of the hip. The greater trochanteric bursa is between the iliotibial band and the gluteus medius and minimus tendons. The subgluteus minimus bursa is between the gluteus minimus tendon and the femur. The subgluteus medius bursa is between the gluteus medius tendon and the femur.14–18
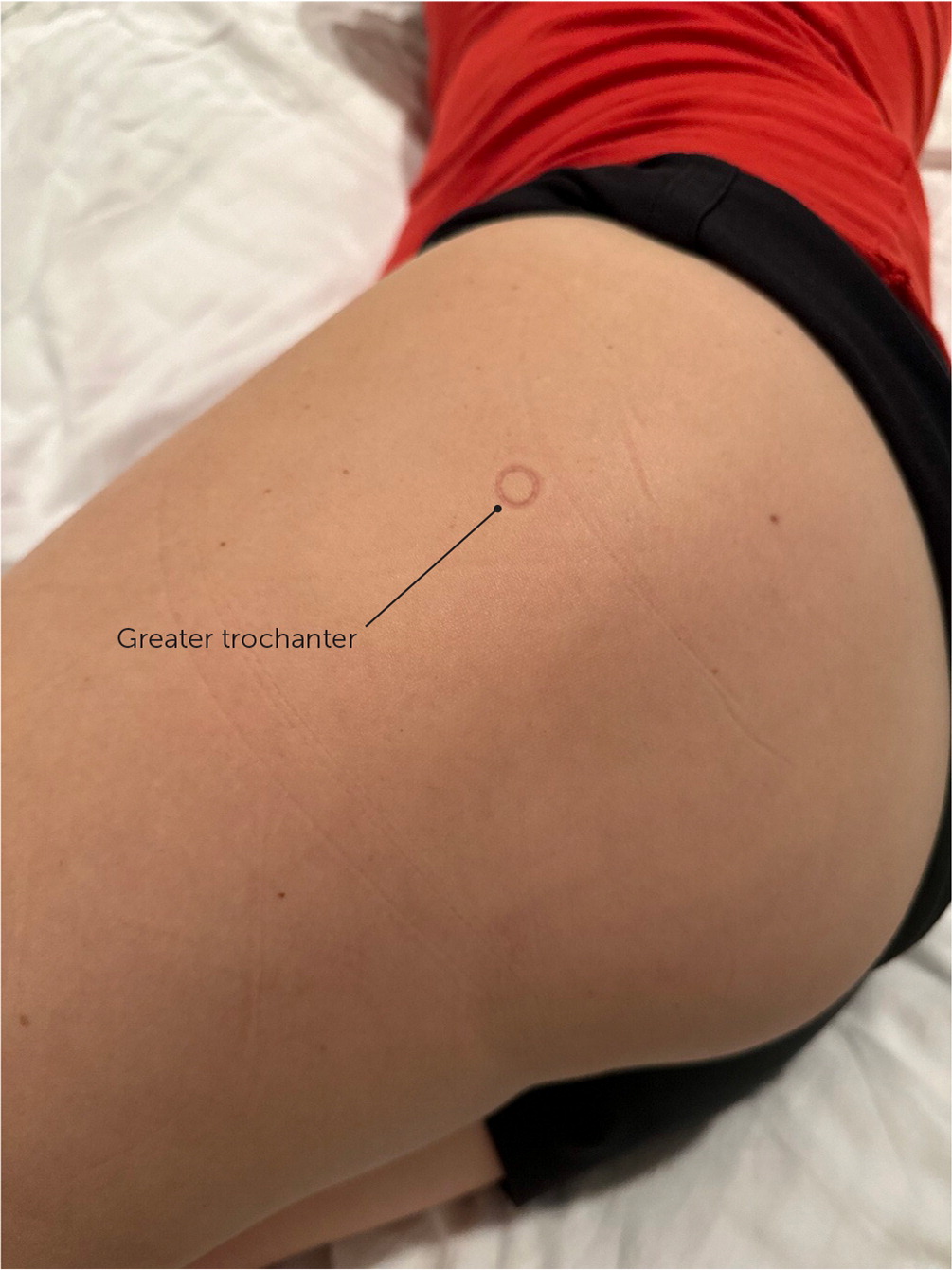
ANATOMIC TECHNIQUE
The patient is in the lateral recumbent position with the painful hip up. The hip and knee are flexed 30 to 50 degrees and 60 to 90 degrees, respectively. The greater trochanter is palpated, and the injection site is the point of maximal tenderness (eFigure A). After the skin is cleaned, a 22- or 25-gauge, 1.5-inch or 3.5-inch needle (depending on the patient's body habitus) is inserted perpendicular to the skin directly toward the greater trochanter and then withdrawn 2 to 3 mm. The injectant should flow easily.
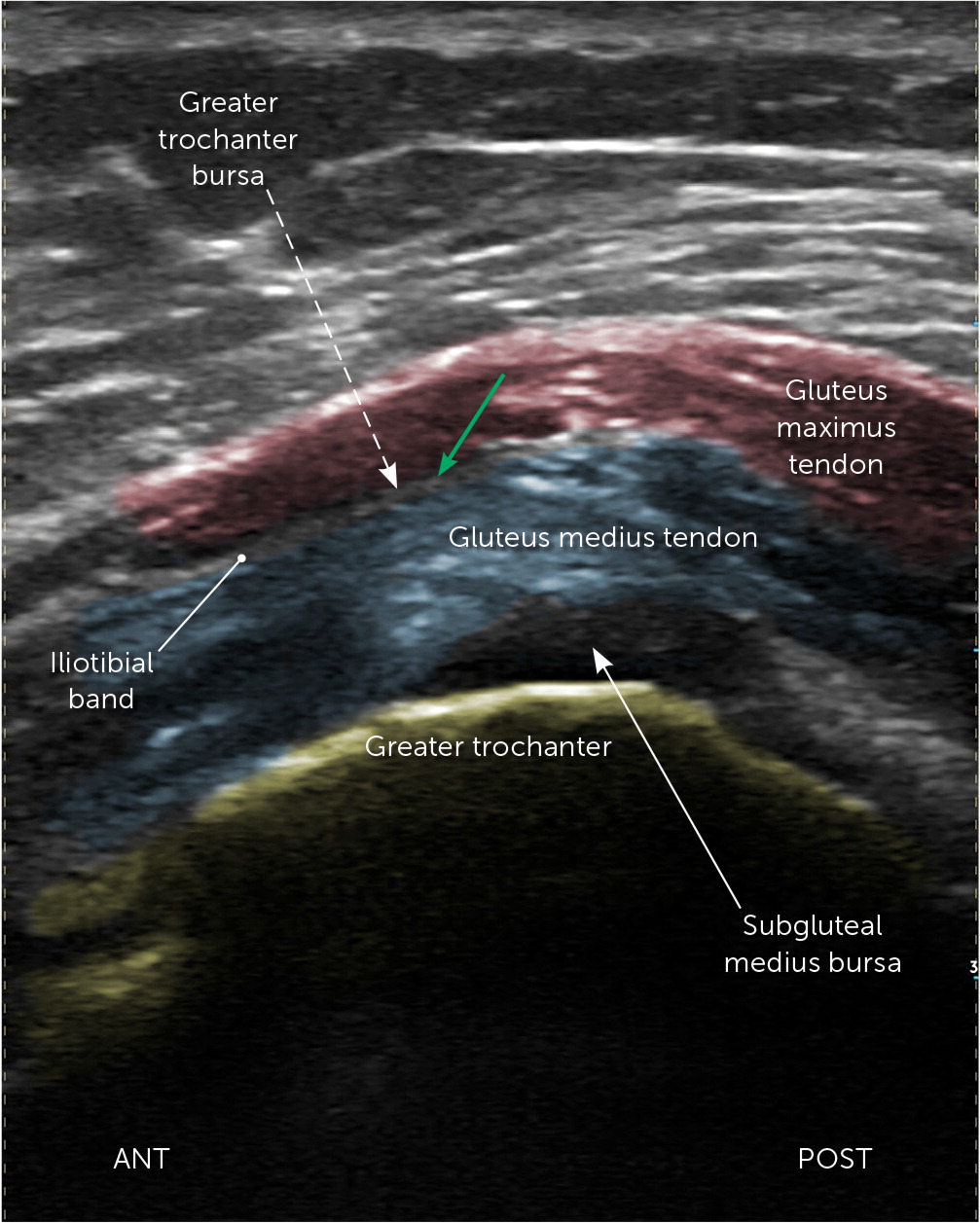
ULTRASOUND TECHNIQUE
The patient is in the lateral recumbent position with the painful hip up. The 5 MHz curvilinear transducer is placed horizontally on the greater trochanter transverse to the femur. The anterior, lateral, and posterior facets are identified. Directly above the lateral facet is the anterior band of the gluteus medius tendon, and the iliotibial band is above that. The needle is inserted in a long axis with the probe from posterior to anterior, targeting the space between the gluteus medius tendon and the iliotibial band14,16,17,19 (Figure 1; https://youtu.be/zkqjTQhn-vs).
Hip Joint Pain
Indications for aspiration or injection of the hip joint include osteoarthritis, inflammatory arthritis, infectious conditions, femoroacetabular impingement, and osteonecrosis. These conditions can cause pain in the groin or thigh that radiates to the buttocks, lower back, or knee with varying degrees of stiffness and locking.1,2,16,17,19,20 Intra-articular injections (with or without corticosteroids) may be used as an adjunct for short and intermediate pain relief and improved function in patients with osteoarthritis of the hip.12,14,15,21–24
ANATOMY
The femoroacetabular joint is a ball-and-socket synovial joint consisting of a bony acetabulum and femoral head with a fibrocartilaginous labrum that stabilizes the joint. The joint capsule originates superior to the labrum and extends distally to the intertrochanteric line of the femur.1,2,16,19,20
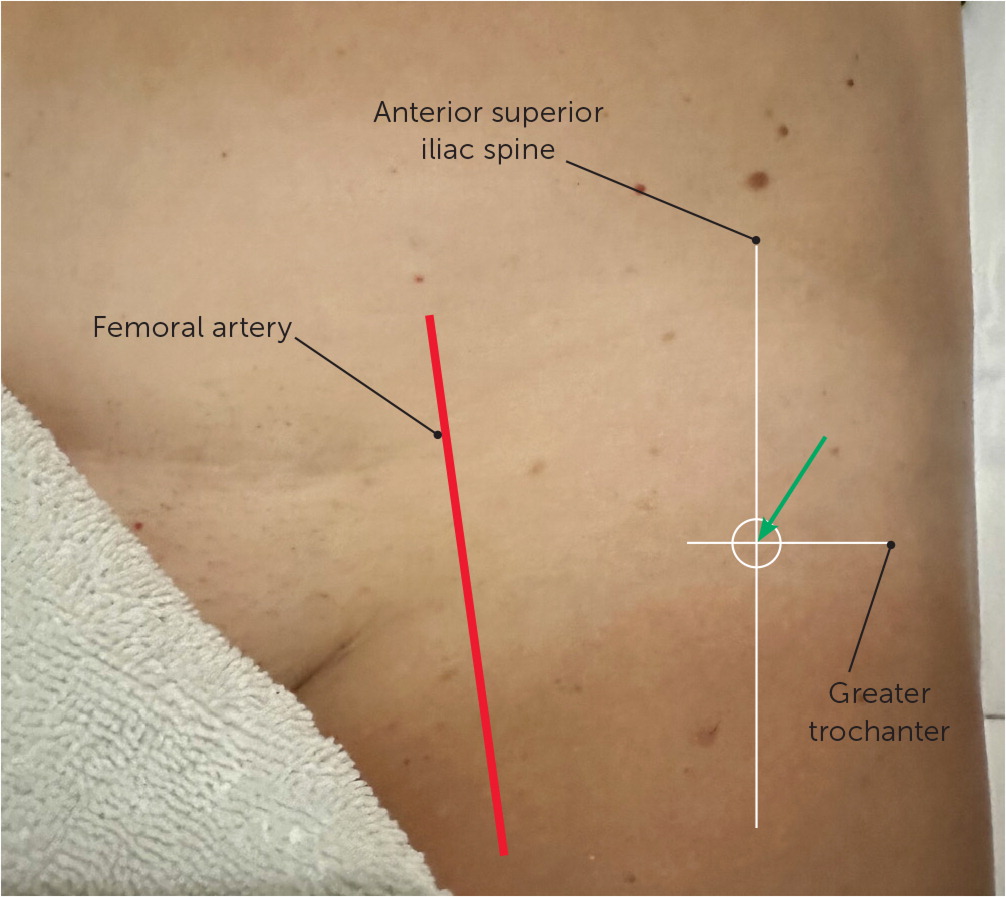
ANATOMIC TECHNIQUE
The patient is in the supine position, with the physician standing next to the painful hip. The injection site is the intersection of a sagittal line drawn distally from the anterosuperior iliac spine and a line drawn transversely from the proximal tip of the greater trochanter (Figure 2). The injection site should be approximately 3 cm lateral from the femoral artery. After the skin has been cleaned, a 22-gauge, 3.5-inch needle is directed posteriorly toward the femoral neck until the needle tip contacts the junction of the femoral head and neck. The needle is withdrawn 1 to 2 mm, and the plunger is retracted to ensure no blood is present before the injection is performed.
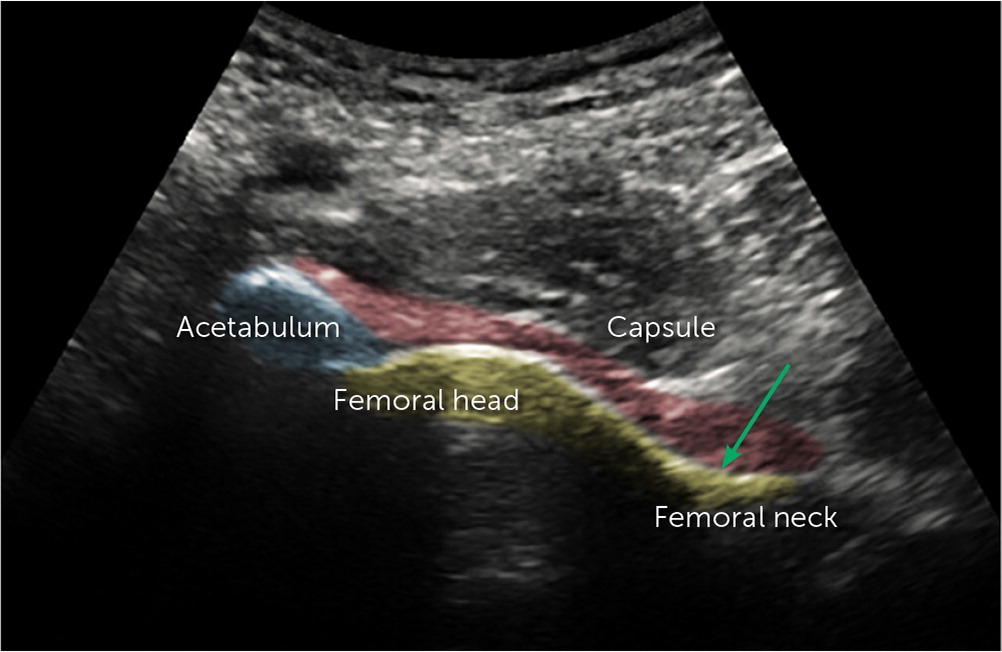
ULTRASOUND TECHNIQUE
The patient is in the supine position, with the 5 MHz curvilinear transducer placed along the femoral neck in a longitudinal, oblique plane. The anterior recess is seen in this position, and any effusion can be identified. After finding the femoral head, the transducer can be moved distally to locate the junction of the femoral neck and head in the axial plane. After the skin has been cleaned, a 22-gauge, 3.5-inch needle is inserted from the lateral side in the long axis of the probe (Figure 3). When the needle is seen in the joint capsule next to the bone, the injection can be performed1,2,16,19,20 (https://youtu.be/zkqjTQhn-vs).
Knee Joint Pain
Pain relief is the primary indication for knee joint injection or aspiration. Aspiration of the knee joint decreases intra-articular pressure, relieving pain. Any fluid obtained can be analyzed to confirm a diagnosis.25,26 Most physicians perform landmark-guided injections for the knee despite multiple studies demonstrating increased accuracy and improved outcomes with ultrasound guidance. Physicians may be more likely to use ultrasound guidance when landmarks are difficult to locate, such as with a history of trauma to the knee or morbid obesity. A systematic review found that knee joint injections are most accurate using the superior lateral approach, with or without ultrasonography.27,28 Intra-articular injections (with or without corticosteroids) may be used as an adjunct for short and intermediate pain relief and improved function in patients with osteoarthritis of the knee.11,12,15,21–25,29–32
ANATOMY
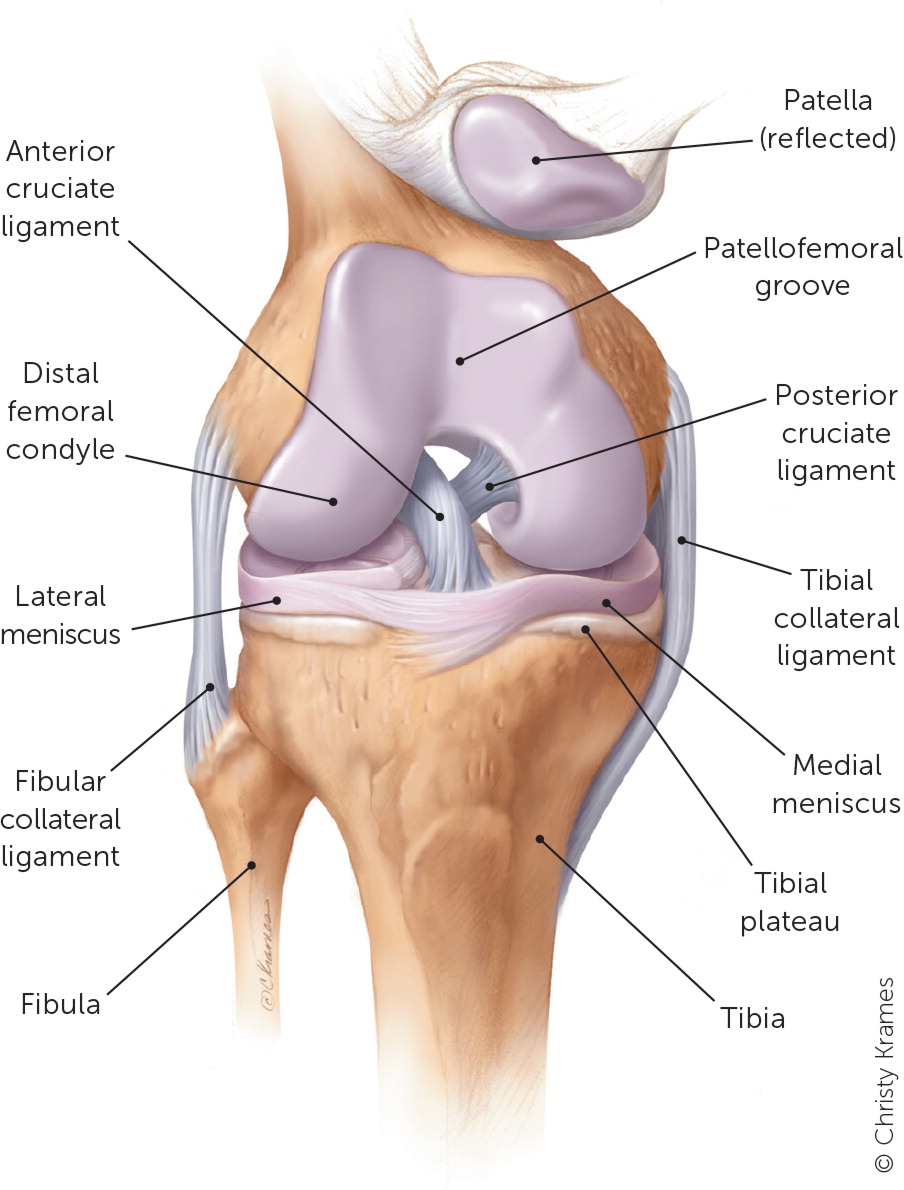
The knee is the largest synovial joint. It comprises a hinge joint with the femoral condyles superiorly, the tibial plateau inferiorly, the patella (sesamoid bone) anteriorly, and two fibrocartilaginous menisci between the tibia and the femur, which act as guides for the femur to glide on top of the tibia33,34 (Figure 435).
SUPINE ANATOMIC TECHNIQUE
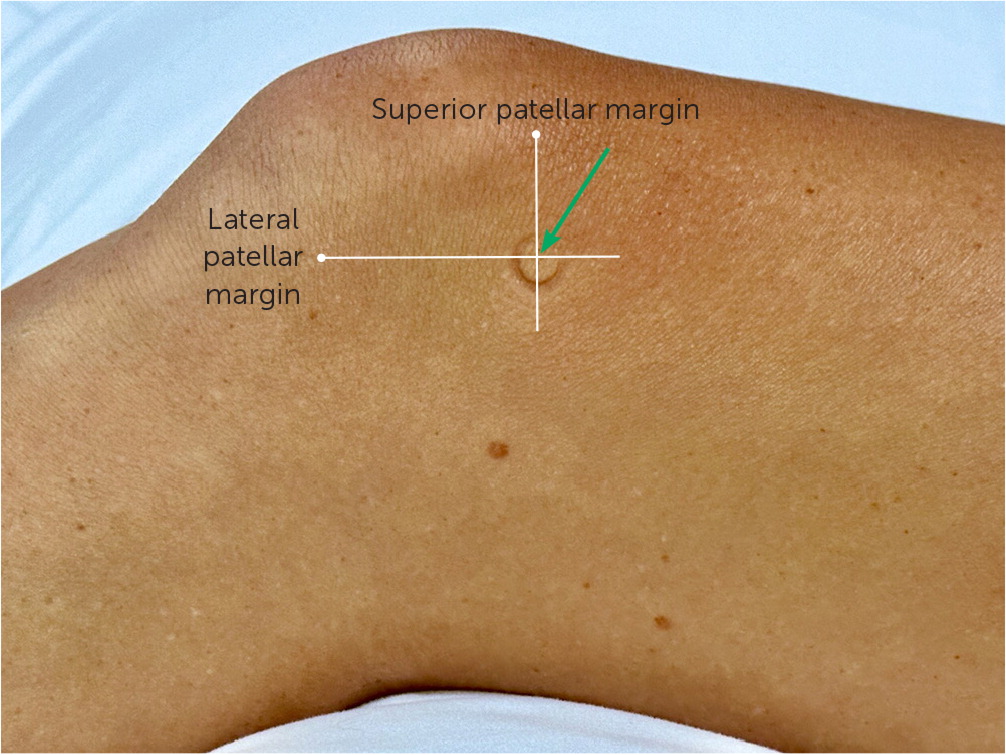
The patient is in the supine position with the knee slightly flexed (15 to 20 degrees) and supported by a foam roll, pillow, or rolled towel. Lines are drawn along the lateral and superior margins of the patella (Figure 5). A 22-gauge, 1.5-inch needle is inserted into the soft tissue between the patella and the femur at the intersection of these two lines. The needle should be aimed toward the middle of the medial side of the joint (approximately a 45-degree angle). The injectant flow should be even with no resistance.27,28,36,37
SEATED ANATOMIC TECHNIQUE
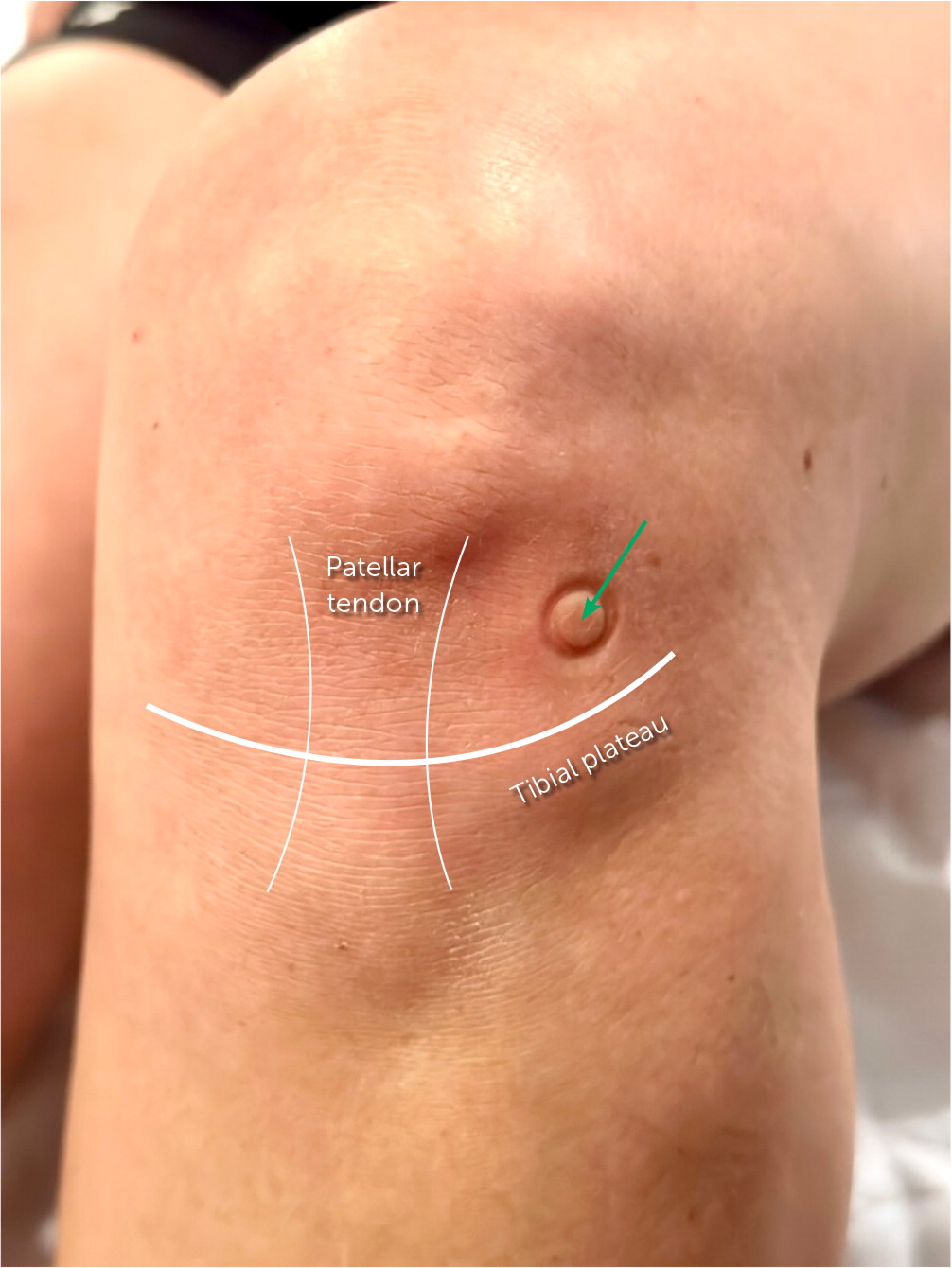
The patient is seated at the end of the examination table. The physician palpates up from the tibia tubercle along the patellar tendon, then moves laterally or medially to the soft tissue between the femur and tibia. A 22-gauge, 1.5-inch needle is inserted parallel to the floor, aiming toward the center of the joint (Figure 6).
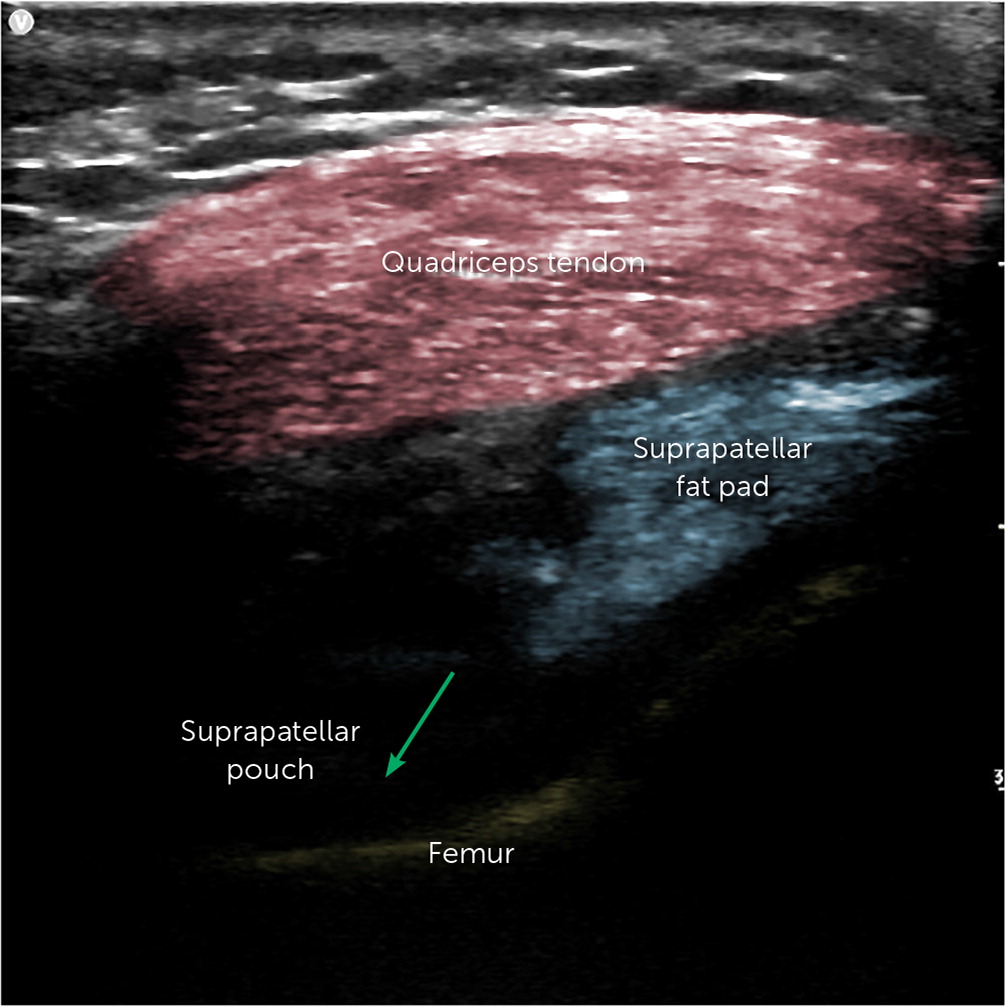
ULTRASOUND TECHNIQUE
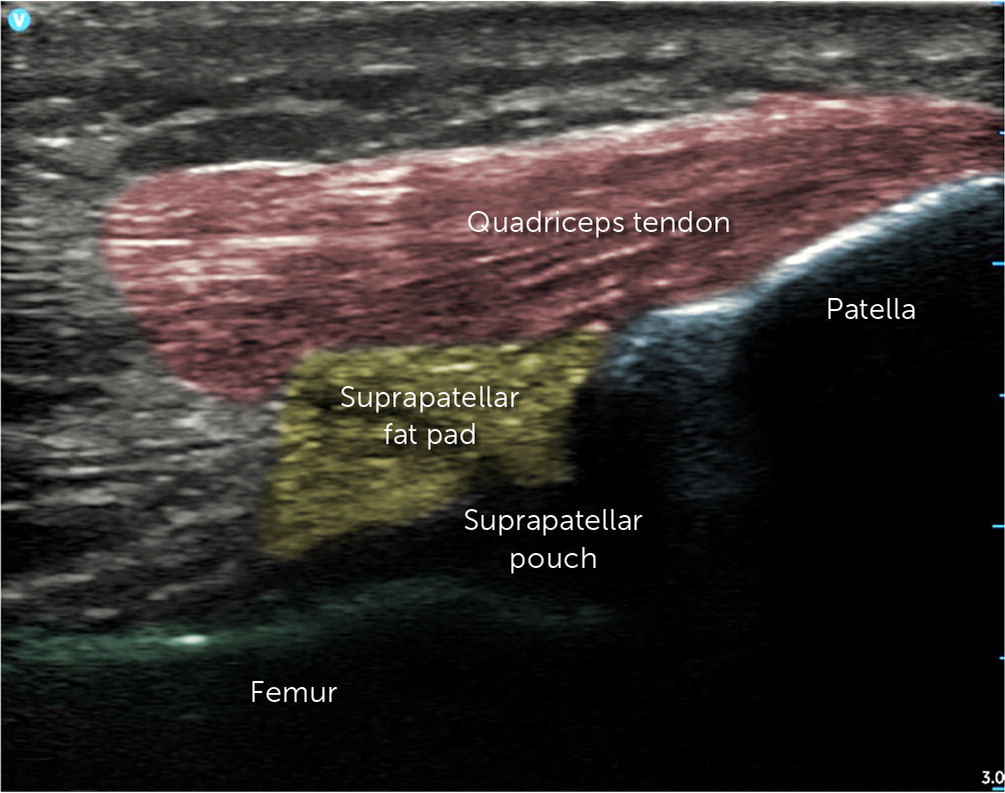
The patient is in the supine position with the knee slightly flexed. The 12 MHz linear array probe is placed superolaterally to the patella with the beam directed medially toward the patellofemoral space (Figure 7). The image seen from anterior to posterior includes the quadriceps tendon, suprapatellar fat pad, suprapatellar pouch, and femur (Figure 8). A 22-gauge, 1.5-inch needle is inserted in the long axis with the probe directed into the suprapatellar pouch34,36 (Figure 9; https://youtu.be/qKQKzFQgYAs).

Pes Anserine Bursitis
Patients with pes anserine bursitis report pain and swelling on the medial side of the knee, directly over the pes anserine insertion. The pain may radiate proximally when palpated along the semitendinosus tendon. The pain gradually increases with running and especially with climbing stairs.34
ANATOMY
The pes anserine bursa is located 2 cm distal to the tibial plateau on the medial side of the knee and is the insertion of the pes anserine tendon, which is the combination of the sartorius, gracilis, and semitendinosus muscles.
ANATOMIC TECHNIQUE
The patient is supine with the knee slightly flexed (10 to 20 degrees) or seated with the knee flexed 90 degrees. The pes anserine tendon and its associated muscles can be located by having the patient flex the knee against resistance. The tendons can be palpated and followed distally to their insertion on the tibia. The bursa is the area of tenderness just proximal to the insertion point. The needle is inserted into the bone at the area of maximal tenderness and then withdrawn 2 to 3 mm (Figure 10).
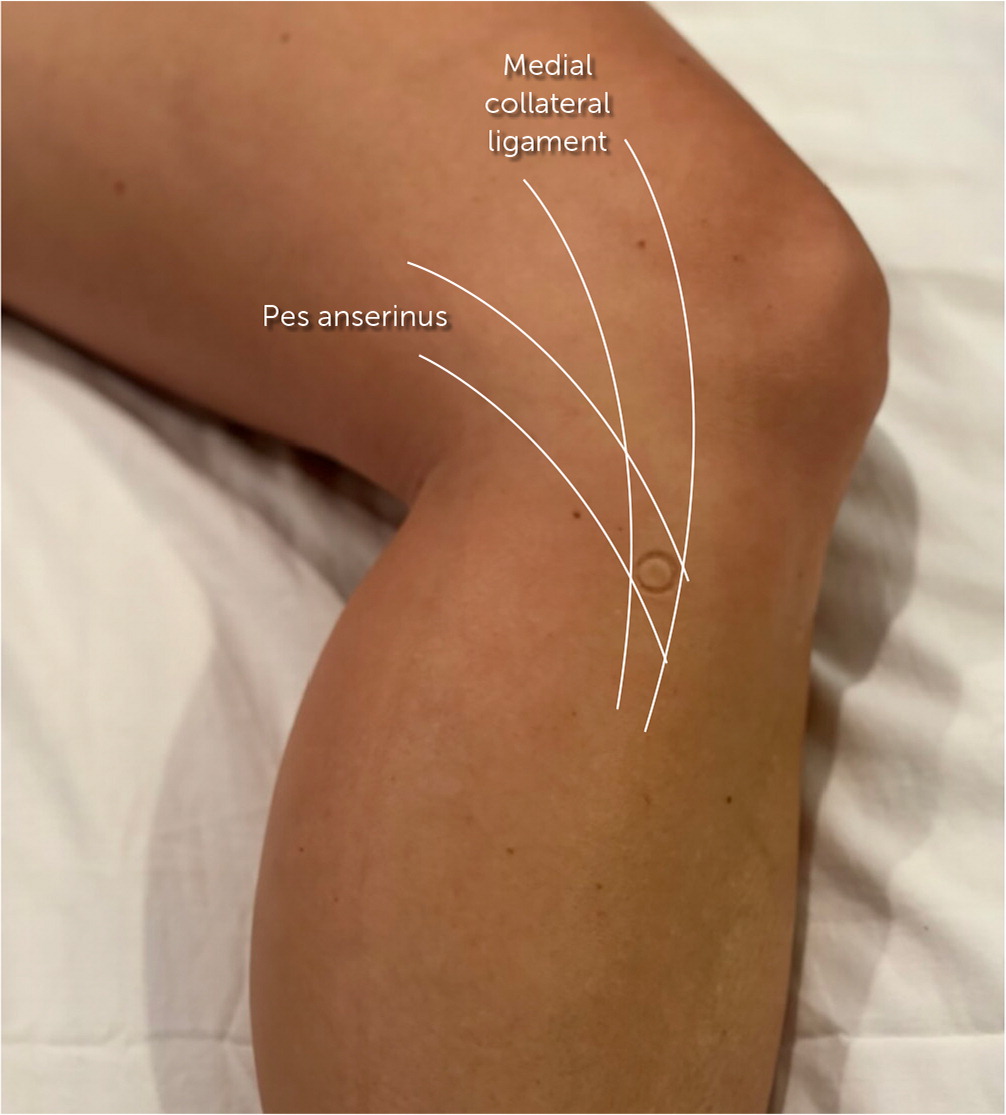
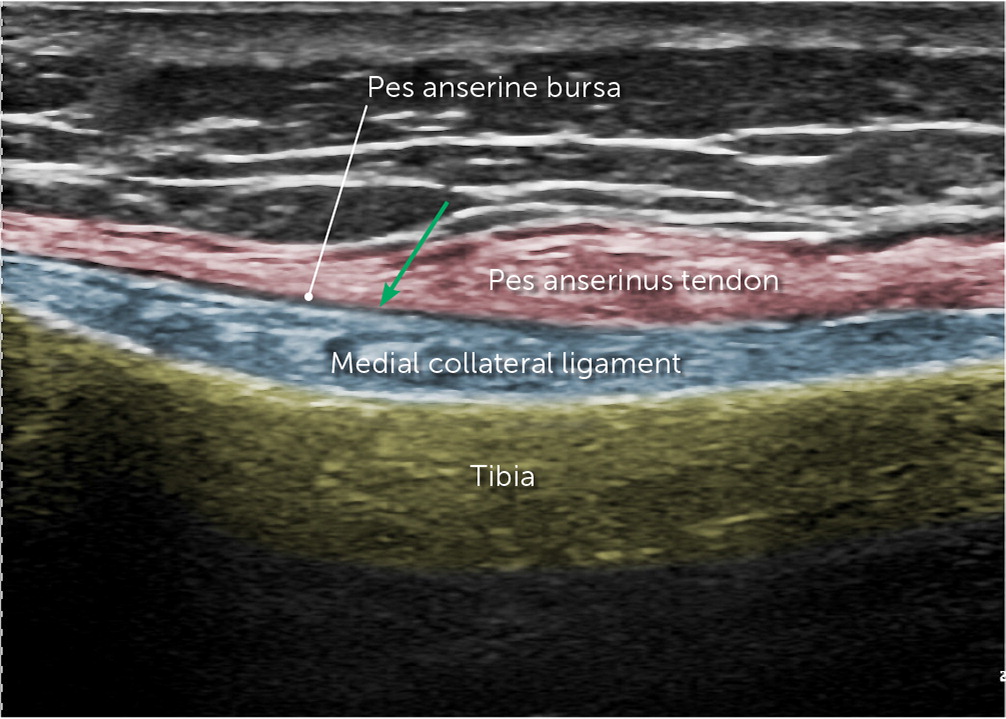
ULTRASOUND TECHNIQUE
The patient is supine with the hip externally rotated and the knee slightly flexed. The 12 MHz linear array probe is placed in the coronal plane over the anterior fibers of the distal medial collateral ligament. Deep to the pes anserine fibers and superficial to the medial collateral ligament, the pes anserine bursa can be identified as the target when it contains fluid. A 22-gauge, 1.5-inch needle is directed into the bursa in the long axis with the probe 11,34 (Figure 11; https://youtu.be/C4NmmyzvbcA).
Iliotibial Band Syndrome
Patients with iliotibial band syndrome present with pain at the lateral femoral condyle or its insertion at the proximal tibia. The pain worsens with activity, running, or walking and improves with rest.
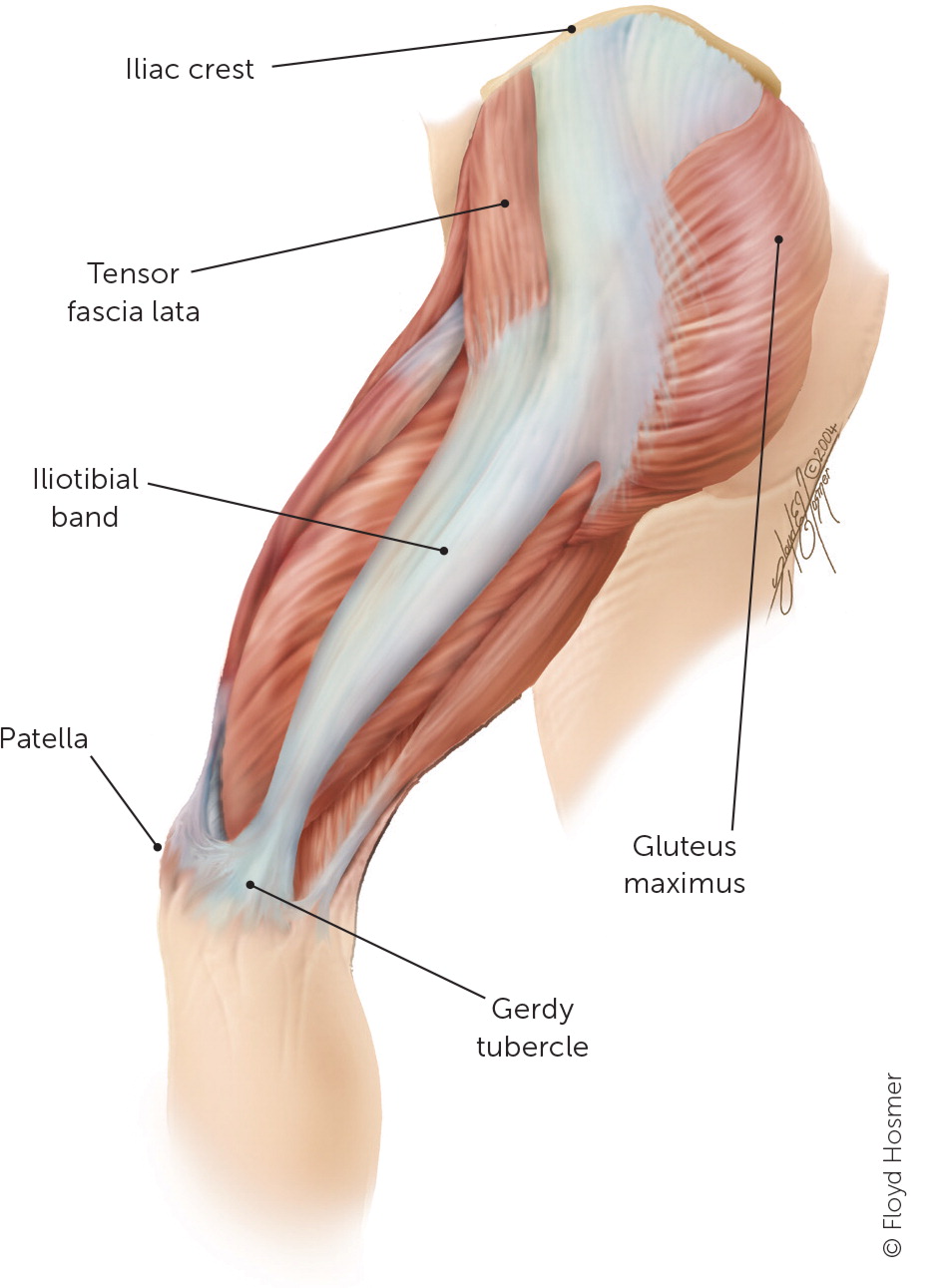
ANATOMY
The iliotibial band begins at the iliac crest and runs down the leg to the tibia, attaching to the Gerdy tubercle (Figure 1238). The iliotibial band helps abduct and stabilize the hip during a single-leg stance. Overuse can cause pain, tightness of the tensor fasciae latae muscle, pes cavus, and/or gluteal muscle weakness.
Patients with pain at the distal femoral condyle (Noble compression test) or over the Gerdy tubercle should have a positive Ober sign with tightness of the iliotibial band at the greater trochanter. The Ober test is performed by having the patient lie on the unaffected side with the physician stabilizing the affected pelvis. The physician passively flexes, abducts, and extends the affected hip with the knee flexed 90 degrees until it is aligned with the patient's trunk, then lowers the knee to the table. If the affected knee reaches the table (the level of the unaffected leg) with no pain, the test result is normal. If pain is felt or the knee is not able to reach the unaffected leg, the test result is positive, indicating a tight iliotibial band.38
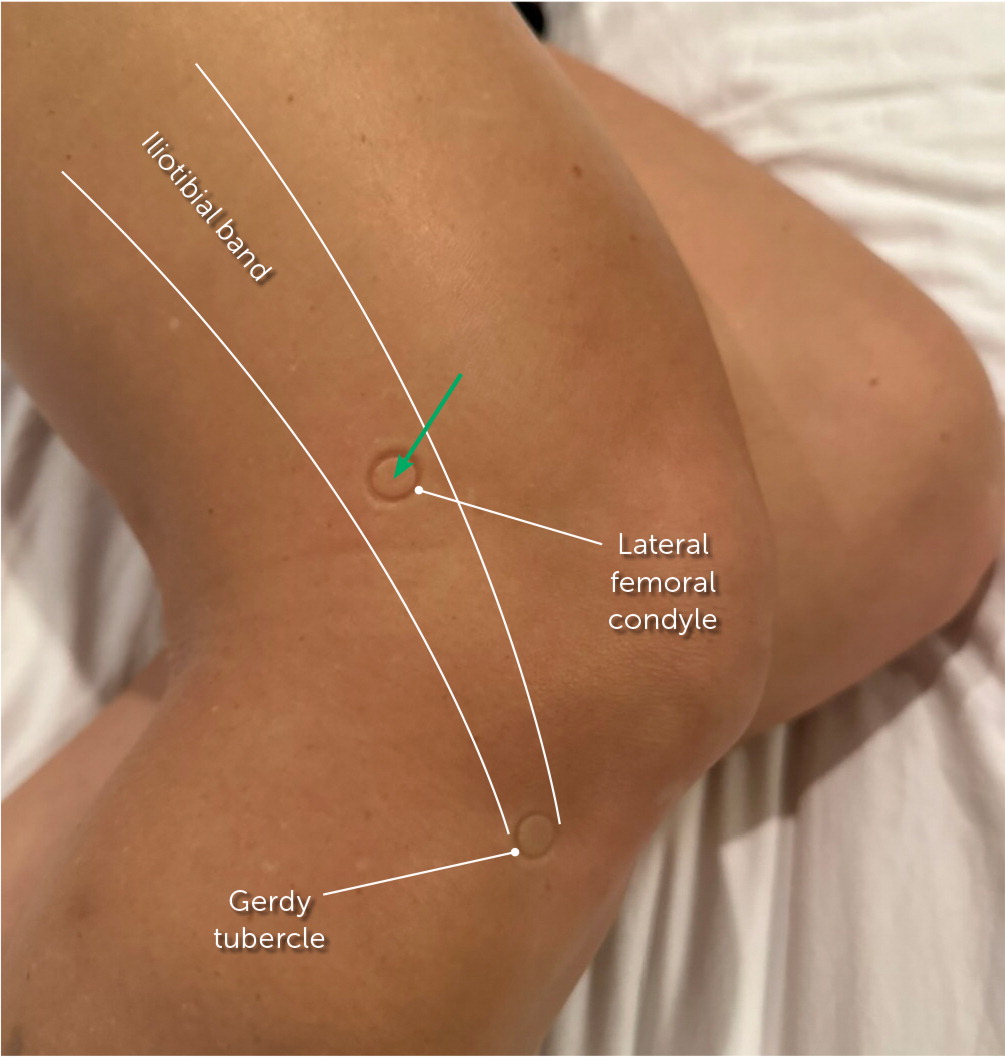
ANATOMIC TECHNIQUE
The patient is in the lateral recumbent or supine position. The knee is flexed 20 to 30 degrees or over a pillow or rolled towel. The iliotibial band is palpated over the femoral condyle to insertion at the Gerdy tubercle. A 22-gauge, 1.5-inch needle is then inserted into the point of maximal tenderness near the lateral femoral condyle11 (Figure 13).
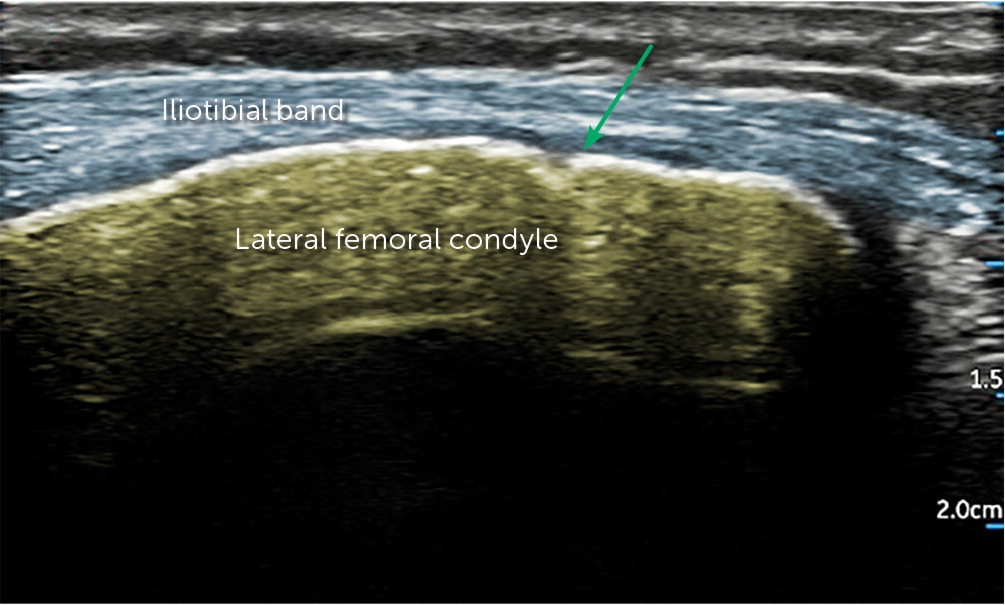
ULTRASOUND TECHNIQUE
The patient is in the lateral recumbent position with the knee flexed to 20 to 30 degrees. The 12 MHz linear array probe is placed on the long axis over the iliotibial band, with the iliotibial band and the lateral femoral condyle in view. A collection of fluid between the iliotibial band and the lateral femoral condyle is the target for the injection (Figure 14). A 22-gauge, 1.5-inch needle is used for the injection, using an out-of-plane ultrasound technique with the needle perpendicular to the probe (https://youtu.be/qKQKzFQgYAs).
Contraindications
There are few contraindications for injections that are not related to the actual injectant. Superficial skin or soft tissue infections are contraindications because injections could potentially seed the joint or bursa. Aspiration can be therapeutic (pain relieving) and diagnostic if a joint infection is suspected. Unstable coagulopathies and fractures are relative contraindications; however, patients with hemarthrosis may benefit from pain-relieving aspirations.2,21,29,30
Aftercare
Following the aspiration of a bursa, especially those that are more superficially located, a pressure dressing should be used to limit the accumulation of fluid. Following any injection or aspiration of a joint or bursa, patients should be advised to avoid strenuous activity for several days. Patients should also be advised that a steroid flare-up may occur in the first 24 to 48 hours after injection. Pain, soreness, or irritation that worsens or lasts more than 72 to 96 hours after injection can be a sign of iatrogenic infection, and the patient should be reevaluated as soon as possible. All patients should have a follow-up appointment scheduled for two to six weeks postinjection.11,26,29,38
This article updates a previous article on this topic by Cardone and Tallia.11
Data Sources: A PubMed search was completed in Clinical Queries using the key terms injection technique, ultrasound, landmark, hip, and knee. The search included meta-analyses, randomized controlled trials, and systematic reviews. Also searched were the Cochrane database, DynaMed, and UpToDate. A second PubMed search was completed using the key terms musculoskeletal injections, hip injections, knee injections, ultrasound injections, and landmark guided injections. Search dates: November 22, 2022; January 20, 2023; May 1, 2023; and November 6, 2023.
