
Am Fam Physician. 2003;68(1):135-140
A more recent article on Bartholin gland cyst and gland abscess is available.
Bartholin's duct cysts and gland abscesses are common problems in women of reproductive age. Bartholin's glands are located bilaterally at the posterior introitus and drain through ducts that empty into the vestibule at approximately the 4 o'clock and 8 o'clock positions. These normally pea-sized glands are palpable only if the duct becomes cystic or a gland abscess develops. The differential diagnosis includes cystic and solid lesions of the vulva, such as epidermal inclusion cyst, Skene's duct cyst, hidradenoma papilliferum, and lipoma. The goal of management is to preserve the gland and its function if possible. Office-based procedures include insertion of a Word catheter for a duct cyst or gland abscess, and marsupialization of a cyst; marsupialization should not be used to treat a gland abscess. Broad-spectrum antibiotic therapy is warranted only when cellulitis is present. Excisional biopsy is reserved for use in ruling out adenocarcinoma in menopausal or perimenopausal women with an irregular, nodular Bartholin's gland mass.
Family physicians can expect to encounter Bartholin's duct cysts or gland abscesses in their female patients. These common problems often can be resolved with the use of simple office-based procedures such as Word catheter placement for duct cysts or gland abscesses, and marsupialization for duct cysts.
Anatomy
Bartholin's glands (greater vestibular glands) are homologues of the Cowper's glands (bul-bourethral glands) in males.1 At puberty, these glands begin to function, providing moisture for the vestibule.
The Bartholin's glands develop from buds in the epithelium of the posterior area of the vestibule. The glands are located bilaterally at the base of the labia minora and drain through 2- to 2.5-cm–long ducts that empty into the vestibule at about the 4 o'clock and 8 o'clock positions2,3 (Figure 1). The glands are usually the size of a pea and rarely exceed 1 cm. They are not palpable except in the presence of disease or infection.
Epidemiology
Bartholin's duct cysts, the most common cystic growths in the vulva,4,5 occur in the labia majora.6 Two percent of women develop a Bartholin's duct cyst or gland abscess at some time in life.6 Abscesses are almost three times more common than cysts. One case-control study7 found that white and black women were more likely to develop Bartholin's cysts or abscesses than Hispanic women, and that women of high parity were at lowest risk.
Gradual involution of the Bartholin's glands can occur by the time a woman reaches 30 years of age.8 This may account for the more frequent occurrence of Bartholin's duct cysts and gland abscesses during the reproductive years, especially between 20 and 29 years of age.
Because a vulvar mass in a postmenopausal woman can be cancer, excisional biopsy may be required. Some investigators9 have suggested that surgical excision is unnecessary because of the low risk of Bartholin's gland cancer (0.114 cancers per 100,000 woman-years). However, if the diagnosis of cancer is delayed, the prognosis can be poor.
Pathology
Obstruction of the distal Bartholin's duct may result in the retention of secretions, with resultant dilation of the duct and formation of a cyst. The cyst may become infected, and an abscess may develop in the gland. A Bartholin's duct cyst does not necessarily have to be present before a gland abscess develops.10
Bartholin's gland abscesses are polymicrobial (Table 1).4,11,12 Although Neisseria gonorrhoeae is the predominant aerobic isolate, anaerobes are the most common pathogens.10,11,13 Chlamydia trachomatis also may be a causative organism.14 However, Bartholin's duct cysts and gland abscesses are no longer considered to be exclusively the result of sexually transmitted infections.4 Vulvovaginal surgery is an uncommon cause of these cysts and abscesses.15
| Aerobic organisms |
| Neisseria gonorrhoeae |
| Staphylococcus aureus |
| Streptococcus faecalis |
| Escherichia coli |
| Pseudomonas aeruginosa |
| Chlamydia trachomatis |
| Anaerobic organisms |
| Bacteroides fragilis |
| Clostridium perfringens |
| Peptostreptococcus species |
| Fusobacterium species |
Presentation
If a Bartholin's duct cyst remains small and does not become inflamed, it may be asymptomatic. However, the cyst typically presents as a medially protruding mass in the posterior introitus in the region where the duct opens into the vestibule.10 If the cyst becomes infected, an abscess may form in the gland (Figure 2).10 Induration usually is present around the gland,10 and walking, sitting, or sexual intercourse may result in vulvar pain.
Bartholin's duct cysts and gland abscesses must be differentiated from other vulvar masses.1,6,8,10 The most common cystic and solid vulvar lesions are listed in Table 2. Because the Bartholin's glands usually shrink during menopause, a vulvar growth in a postmenopausal woman should be evaluated for malignancy, especially if the mass is irregular, nodular, and persistently indurated.10
| Lesion | Location | Characteristics |
|---|---|---|
| Cystic lesions | ||
| Bartholin's duct cyst | Vestibule | Usually unilateral; asymptomatic if remains small |
| Epidermal inclusion cyst | Labia majora (usually) | Benign, mobile, nontender; caused by trauma or obstruction of pilosebaceous ducts |
| Mucous cyst of the vestibule | Labia minora, vestibule, periclitoral area | Soft, less than 2 cm in diameter, smooth surface, superficial location; solitary or multiple; usually asymptomatic |
| Hidradenoma papilliferum | Between labia majora and labia minora | Benign, slow-growing, small nodule (2 mm to 3 cm); arises from apocrine sweat glands |
| Cyst of the canal of Nuck | Labia majora, mons pubis | Soft, compressible; peritoneum entrapped within round ligament; may mimic inguinal hernia |
| Skene's duct cyst | Adjacent to urethral meatus in vestibule | Benign, asymptomatic; if large, may cause urethral obstruction and urinary retention |
| Solid lesions | ||
| Fibroma | Labia majora, perineal body, introitus | Firm, asymptomatic; may develop pedicle; may undergo myxomatous degeneration; potential for malignancy |
| Lipoma | Labia majora, clitoris | Benign, slow-growing; sessile or pedunculated |
| Leiomyoma | Labia majora | Rare; solitary, firm; arises from smooth muscle |
| Acrochordon | Labia majora | Benign, fleshy, variable size; usually pedunculated but may be sessile; polypoid in appearance |
| Neurofibroma | Multicentric | Small, fleshy; polypoid in appearance; multiple; associated with von Recklinghausen's disease |
| Angiokeratoma | Multicentric | Rare, benign; vascular; variable size and shape; single or multiple; associated with and aggravated by pregnancy; associated with Fabry's disease |
| Squamous cell carcinoma | Multicentric | Related to benign epithelial disease in older women and to human papillomavirus infection in young women |
Treatment
The treatment of a Bartholin's duct cyst depends on the patient's symptoms. An asymptomatic cyst may require no treatment,2 but symptomatic Bartholin's duct cysts and gland abscesses require drainage. Unless spontaneous rupture occurs, an abscess rarely resolves on its own.
Although incision and drainage is a relatively quick and easy procedure that provides almost immediate relief to the patient, this approach should be discouraged because there is a tendency for the cyst or abscess to recur.1,5,16 One investigator17 reported a 13 percent failure rate for the procedure. Furthermore, incision and drainage may make later Word catheter placement or marsupialization difficult.1,16
Definitive drainage involves Word catheter placement for Bartholin's duct cysts and gland abscesses, and marsupialization for duct cysts.
WORD CATHETER

After sterile preparation and the administration of a local anesthetic, the wall of the cyst or abscess is grasped with a small forceps, and a no. 11 blade is used to make a 5-mm (stab) incision into the cyst or abscess2,16 (Table 3). It is important to grasp the cyst wall before the incision is made; otherwise the cyst can collapse, and a false tract may be created.16 The incision should be within the introitus external to the hymenal ring in the area of the duct orifice.10,16 If the incision is too large, the Word catheter will fall out.
| Sterile gloves |
| Iodine solution |
| Lidocaine (Xylocaine), 1% or 2% solution |
| 30-gauge, 1-inch needle with 5-mL syringe for injecting lidocaine |
| Word catheter |
| Saline solution, 3 mL |
| 25-gauge, 1-inch needle with 3-mL syringe for inflating balloon with saline solution |
| Small forceps for grasping cyst wall |
| No. 11 scalpel |
| Gauze pads, 4 3 4 inch |
| Hemostats to break up loculations |
After the incision is made, the Word catheter is inserted, and the balloon tip is inflated with 2 to 3 mL of saline solution injected through the hub of the catheter. The inflated balloon allows the catheter to remain within the cavity of the cyst or abscess (Figure 3). The free end of the catheter can be placed in the vagina.16 To allow epithelialization of the surgically created tract, the Word catheter is left in place for four to six weeks,1,10,16 although epithelialization may occur as soon as three to four weeks.18
Sitz baths taken two to three times daily may aid patient comfort and healing during the immediate postoperative period. Coitus may be resumed after catheter insertion.
Unless there is evidence of cellulitis, antibiotic therapy is unnecessary. If cellulitis is present, cultures may be obtained, but the results rarely change management. Empiric broad-spectrum antibiotic therapy is started before culture results are available.13
If a Bartholin's cyst or abscess is too deep, Word catheter placement is impractical, and other options must be considered.10
MARSUPIALIZATION
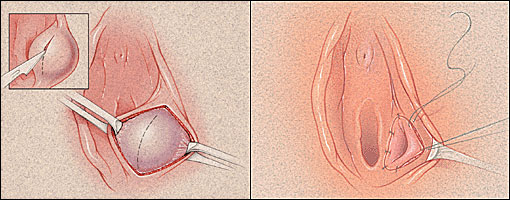
After sterile preparation and the administration of a local anesthetic, the cyst wall is grasped with two small hemostats2,16 (Table 4). A vertical incision is made in the vestibule over the center of the cyst and outside the hymenal ring.18 The incision should be about 1.5 to 3 cm long, depending on the size of the cyst.
| Sterile gloves |
| Iodine solution |
| Lidocaine (Xylocaine), 1% or 2% solution |
| 25-gauge, 1-inch needle with 5-mL syringe for injecting lidocaine |
| No. 11 scalpel |
| Two small hemostats for grasping cyst wall |
| Gauze pads, 4 3 4 inch |
| Hemostats to break up loculations |
| Small needle threaded with 2-0 absorbable suture |
| Needle holder |
| Scissors |
After the cyst is vertically excised, the cavity drains spontaneously. The cavity also may be irrigated with saline solution and, if necessary, loculations can be broken up with a hemostat. The cyst wall is then everted and approximated to the edge of the vestibular mucosa with interrupted 2-0 absorbable suture.18 Daily sitz baths should begin on the first postoperative day.
EXCISION
Although Bartholin's gland abscesses may rupture and drain spontaneously, recurrence is likely, and surgical excision may be necessary. Excision is not an office-based procedure.
Cultures for N. gonorrhoeae and C. trachomatis may be obtained. However, Bartholin's gland abscesses tend to be polymicrobial, and empiric broad-spectrum antibiotic therapy should be used.
Excision of the Bartholin's gland should be considered in patients who do not respond to conservative attempts to create a drainage tract, but the procedure should be performed when there is no active infection.1,4 If multiple attempts have been made to drain a cyst or an abscess, adhesions may be present, making excision difficult and resulting in postoperative scarring and chronic pain in the area.2,10
Some investigators2,10 recommend excision of the Bartholin's gland to exclude adenocarcinoma when cysts or abscesses occur in patients more than 40 years of age. Even though adenocarcinoma of the Bartholin's gland is rare, gynecologic oncology referral should be considered for older patients with Bartholin's duct cysts or gland abscesses.