
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2004;70(9):1685-1692
Acute rhinosinusitis is one of the most common conditions that physicians treat in ambulatory practice. Although often caused by viruses, it sometimes is caused by bacteria, a condition that is called acute bacterial rhinosinusitis. The signs and symptoms of acute bacterial rhinosinusitis and prolonged viral upper respiratory infection are similar, which makes accurate clinical diagnosis difficult. Because two thirds of patients with acute bacterial rhinosinusitis improve without antibiotic treatment and most patients with viral upper respiratory infection improve within seven days, antibiotic therapy should be reserved for use in patients who have had symptoms for more than seven days and meet clinical criteria. Four signs and symptoms are the most helpful in predicting acute bacterial rhinosinusitis: purulent nasal discharge, maxillary tooth or facial pain (especially unilateral), unilateral maxillary sinus tenderness, and worsening symptoms after initial improvement. Sinus radiography and ultrasonography are not recommended in the diagnosis of uncomplicated acute bacterial rhinosinusitis, although computed tomography has a role in the care of patients with recurrent or chronic symptoms.
Acute rhinosinusitis is defined as inflammation or infection of the mucosa of the nasal passages and at least one of the paranasal sinuses. It is one of the 10 most common conditions treated in ambulatory practice in the United States, accounting for an estimated 25 million office visits in 1995.1 Part I of this two-part article reviews the evaluation of patients with suspected acute bacterial rhinosinusitis. Part II2 reviews treatment options.
| Key clinical recommendation | Label | References |
|---|---|---|
| Most cases of acute rhinosinusitis are caused by viral upper respiratory infections. | B | 1,4 |
| Bacterial and viral acute rhinosinusitis are difficult to differentiate. The diagnosis of ABRS should be reserved for patients with a duration of symptoms of seven days or longer. | C | 3 |
| Four signs and symptoms are probably helpful in diagnosing ABRS: purulent nasal discharge, maxillary tooth or facial pain (especially unilateral), unilateral maxillary sinus tenderness, and worsening symptoms after initial improvement. | C | 3 |
| Sinus radiography is not recommended in the diagnosis of uncomplicated ABRS. | B | 5,6,7 |
Although usually caused by viruses, acute rhinosinusitis sometimes is complicated by a bacterial infection, a condition called acute bacterial rhinosinusitis (ABRS).3 A working classification of ABRS according to the timing and duration of symptoms has been developed by the Task Force on Rhinosinusitis sponsored by the American Academy of Otolaryngology–Head and Neck Surgery (Table 1).4
| Classification | Duration |
|---|---|
| Acute | ≤ 4 weeks |
| Subacute | 4 to 12 weeks |
| Recurrent acute | ≥ 4 episodes per year, with each episode lasting seven to 10 days |
| Chronic | ≥ 12 weeks |
| Acute exacerbation of chronic sinusitis | Sudden worsening of chronic sinusitis, with return to baseline after treatment |
The signs and symptoms of ABRS and prolonged viral upper respiratory infection (URI) are similar, making it difficult to come to an accurate clinical diagnosis. Although about one in eight patients presenting with URI symptoms has ABRS,3 family physicians prescribe antibiotics in up to 98 percent of suspected cases.5 Physicians understand the potential for the development of antibiotic resistance,6 yet prescribe antibiotics because they believe patients want them.7 However, several studies have shown that physicians are inaccurate in perceiving which patients expect antibiotics.8,9 Patients actually want reassurance, a careful examination, symptom relief, and the ability to resume their activities more than they want antibiotics.10
To avoid the emergence and spread of antibiotic-resistant bacteria, a judicious approach to antibiotic use in patients with URI symptoms is important. The cornerstones of management are differentiating ABRS from viral rhinosinusitis and using narrow-spectrum antibiotics.
Pathophysiology
The ostiomeatal complex, the area at the confluence of drainage from the sinuses, is particularly vulnerable to inflammatory changes, swelling, and obstruction. Anatomic variations and other factors generally predispose patients to ABRS by causing inflammation in the ostiomeatal complex (Table 2).11–13 The two most common causes of community-acquired ABRS in adults are Streptococcus pneumoniae and nontypeable Haemophilus influenzae (Table 3).14 Patients with nosocomial infections are more likely to have gram-negative organisms.15 Anaerobic sinus infections often are associated with dental infections or procedures.16 Immunocompromised patients are prone to fungal infections, particularly those caused by Aspergillus and Mucor species.17 It is important to remember that most cases of rhinosinusitis are viral in origin.3
| Viral infection | Cystic fibrosis | ||
| Allergic/nonallergic rhinitis | Mechanical ventilation | ||
| Anatomic variations | Head injuries | ||
| Abnormality of the ostiomeatal complex | Use of nasal tubes | ||
| Septal deviation | Samter’s triad† | ||
| Concha bullosa | Sarcoidosis | ||
| Hypertrophic middle turbinates | Wegener’s granulomatosis | ||
| Haller cells* | Immune deficiency | ||
| Topical nasal medications | Common variable | ||
| Cigarette smoking | IgA | ||
| Diabetes mellitus | IgG subclass | ||
| Swimming/diving/high-altitude climbing | Iatrogenic | ||
| Dental infections and procedures | Acquired immunodeficiency syndrome | ||
| Cocaine abuse | Immotile cilia syndrome | ||
| Agents | Percentage |
|---|---|
| Haemophilus influenzae | 35 |
| Streptococcus pneumoniae | 34 |
| Anaerobes | 6 |
| Gram-negative bacteria | 4 |
| Staphylococcus aureus | 4 |
| Moraxella catarrhalis | 2 |
| Streptococcus pyogenes | 2 |
Clinical Evaluation
Based on the overall clinical impression, physicians correctly diagnose patients with bacterial rhinosinusitis in only about 50 percent of cases.18,19 The duration of symptoms often is cited by physicians as an important factor in deciding whether a patient has a viral URI or ABRS.20 One trial19 studied the natural history of rhinovirus infection in adults and found that the duration of illness ranged from one to 33 days, with most patients feeling well or improved in seven to 10 days. Sixty percent of sinus aspiration cultures from patients who had URI symptoms for at least 10 days are positive for bacteria.21 Therefore, seven days (10 days in children22) has been proposed as a reasonable cutoff, after which a diagnosis of ABRS should be considered in a patient with typical clinical findings.23 The Task Force on Rhinosinusitis4 sponsored by the American Academy of Otolaryngology–Head and Neck Surgery recommends considering a diagnosis of ABRS after 10 to 14 days of URI symptoms or if symptoms worsen after five to seven days.
Studies of the accuracy of signs and symptoms of sinusitis have been limited by the choice of reference standard (Table 4).18,24–28 None has used the “gold standard”—culture showing at least 105 organisms per mL from a direct sinus aspiration. Only two studies compared clinical findings with the presence of purulent sinus aspirates. One study was limited by the overlap of clinical criteria and the lack of aspiration cultures29 and, in the second study, only patients with positive computed tomographic (CT) scans underwent sinus aspiration.18 Five studies have used CT, ultrasonographic, or plain radiographic abnormalities of the sinuses as the reference standard. These studies probably overestimate the presence of ABRS, resulting in biased estimates of the accuracy of clinical findings.24,25,30,31 It is clear, though, that no single clinical finding accurately diagnoses ABRS.
| Probability of sinusitis if finding is: | |||||||
|---|---|---|---|---|---|---|---|
| Finding | Sensitivity (%) | Specificity (%) | Positive likelihood ratio* | Negative likelihood ratio | Positive† | Negative | |
| Signs and symptoms in guidelines‡ | |||||||
| Maxillary pain18,25 | 51 | 61 | 1.4 | 0.8 | 19 | 12 | |
| Maxillary toothache24,25 | 18 to 36 | 83 to 93 | 2.1 to 2.5 | 0.7 to 0.9 | — | — | |
| Purulent secretions18,24–26 | 32 to 62 | 67 to 89 | 1.4 to 5.5 | 0.5 to 0.9 | — | — | |
| Maxillary tenderness18 | 49 | 68 | 1.5 | 0.8 | 21 | 12 | |
| Worsening symptoms after initial improvement (“double sickening”)26 | 72 | 65 | 2.1 | 0.4 | 27 | 7 | |
| Other signs and symptoms | |||||||
| General clinical impression27 | 69 | 79 | 3.2 | 0.3 | 37 | 6 | |
| Previous URI18,25,26 | 85 to 99 | 8 to 28 | 1.1 to 1.2 | 0.1 to 0.6 | — | — | |
| History of colored discharge24,26 | 72 to 89 | 42 to 52 | 1.5 | 0.3 to 0.5 | — | — | |
| Poor response to decongestants24 | 41 | 80 | 2.1 | 0.7 | 26 | 11 | |
| Pain on bending forward25,26 | 67 to 90 | 22 to 58 | 1.2 to 1.6 | 0.5 to 0.6 | — | — | |
| Abnormal transillumination§24 | 73 | 54 | 1.6 | 0.5 | 22 | 8 | |
| Imaging studies | |||||||
| Radiography | |||||||
| Opacification [ corrected] | 41 | 85 | 1.4 | 0.37 | 20 | 6 | |
| Air-fluid level or opacification | 73 | 80 | 3.7 | 0.34 | 39 | 6 | |
| Air-fluid level, opacity, or mucus thickening | 90 | 61 | 2.3 | 0.16 | 29 | 3 | |
| Ultrasonography | 84 (54 to 98) | 69 (30 to 94) | 2.7 | 0.23 | 32 | 4 | |
| Computed tomography∥ | NA | NA | NA | NA | — | — | |
Considering the results of these studies,24,25,30,31 a position paper endorsed by the Centers for Disease Control and Prevention (CDC), the American Academy of Family Physicians, the American College of Physicians–American Society of Internal Medicine, and the Infectious Diseases Society of America concluded that four signs and symptoms are the most helpful in predicting ABRS: purulent nasal discharge, maxillary tooth or facial pain (especially unilateral), unilateral maxillary sinus tenderness, and worsening symptoms after initial improvement.3 Although based on the best available diagnostic test studies, this particular set of findings has not been prospectively validated as a clinical decision rule.
Other groups also have combined findings into clinical decision rules in an attempt to improve the diagnosis of ABRS. The Canadian Sinusitis Symposium guidelines14 recommend the use of a clinical prediction rule based on the Williams criteria (Table 5).24 Using this rule, ABRS is diagnosed when at least four findings are positive, and the diagnosis is ruled out when there are fewer than two positive findings. Sinus radiography is recommended when two or three findings are positive. A second clinical prediction rule is based on findings from a study by Berg and Carenfelt (Table 6).29 In this rule, two or more of four positive findings is 95 percent sensitive and 77 percent specific for ABRS. Given an overall likelihood of ABRS of 15 percent, the likelihood of ABRS is 41 percent if the rule is positive and only 1 percent if the rule is negative. If the likelihood of ABRS is higher, as in a patient who presents after seven to 10 days of symptoms (i.e., 50 percent), the probability of ABRS is 80 percent if the rule is positive and 6 percent if it is negative.
| Probability of sinusitis (%) | |||||
|---|---|---|---|---|---|
| Findings† | Sinusitis | No sinusitis | Likelihood ratio | Given 15% probability | Given 40% probability |
| ≥ 4 | 16 | 4 | 6.4 | 53 | 81 |
| 3 | 29 | 18 | 2.6 | 31 | 63 |
| 2 | 27 | 39 | 1.1 | 16 | 43 |
| 1 | 14 | 48 | 0.5 | 8 | 24 |
| 0 | 2 | 32 | 0.1 | 2 | 6 |
| Totals | 88 | 141 | |||
| Probability of sinusitis (%) | |||||
|---|---|---|---|---|---|
| Findings† | Sinusitis | No sinusitis | Likelihood ratio | Given 15% probability | Given 40% probability |
| 3 or 4 | 55 | 10 | 7.0 | 55 | 82 |
| 2 | 10 | 10 | 1.3 | 18 | 46 |
| 0 or 1 | 3 | 67 | 0.06 | 1 | 4 |
| Totals | 68 | 87 | |||
The Task Force on Rhinosinusitis considers the presence of two or more major findings or one major finding and two or more minor findings (from a list of seven major and seven minor findings) or nasal purulence on examination to be diagnostic of ABRS.4 However, the validity of these recommendations has not been studied, and it is not clear how applicable they are in the primary care setting.
Imaging
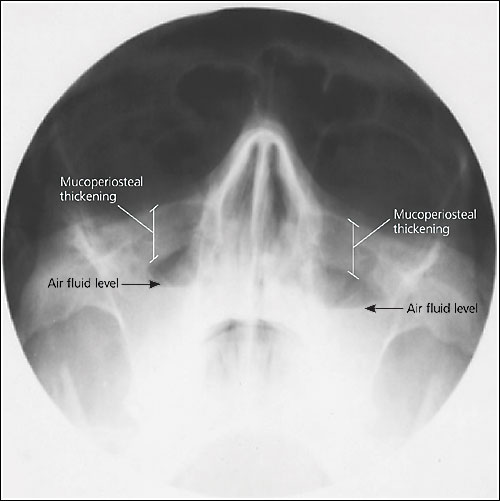
Six studies have investigated the accuracy of plain sinus radiographs, using sinus aspiration as the diagnostic criterion. Sensitivities and specificities of various radiographic findings have been estimated from a meta-analysis of these studies(Table 4).18,24–28 Air-fluid levels or opacity are 73 percent sensitive and 80 percent specific (Figure 1). Adding mucus thickening increased the sensitivity to 90 percent but decreased the specificity. Conversely, restricting the definition of a positive radiograph to only opacification increased the specificity slightly to 85 percent but decreased the sensitivity significantly. The CDC does not recommend sinus radiography in the diagnosis of uncomplicated ABRS.3 The Canadian Sinusitis Symposium guidelines14 recommend radiographs when the probability of ABRS is intermediate based on clinical evaluation. The decision to obtain radiographs should include consideration of the desire for diagnostic certainty, drawbacks to unnecessary antibiotic use, convenience, and cost.
Five studies compared ultrasonography with sinus aspiration. The results demonstrated variable test accuracy, with sensitivities ranging from 54 to 98 percent (mean, 84 percent) and specificities ranging from 30 to 94 percent (mean, 69 percent).23 However, the poor performance in some studies suggests that training and experience are necessary to interpret results accurately; therefore, ultrasonography cannot be recommended for routine use.
CT scanning provides better visualization of the sinuses and ostiomeatal complex than plain radiographs and ultrasonography. CT signs of rhinosinusitis are air-fluid levels, total opacification, or mucosal thickening greater than 5 mm. Limited-sinus CT is a series of four noncontiguous, 5-mm slices in the coronal plane through the frontal sinus, the anterior ethmoid and maxillary sinuses, the posterior ethmoid and maxillary sinuses, and the sphenoid sinus. Limited-sinus CT is less expensive and results in less radiation exposure than full-sinus CT. The sensitivity of CT is unknown because it has never been compared with sinus aspiration. Only 62 percent of patients with sinus symptoms have CT abnormalities.11 In addition, the CT scan lacks specificity. Forty-two percent of patients undergoing head CT for other reasons have sinus mucosal abnormalities,32,33 and up to 87 percent of patients with common colds have abnormalities of at least one maxillary sinus.34
Radiography and ultrasonography have a limited role in the evaluation of patients with suspected ABRS. CT scanning should not be used for routine evaluation of ABRS, but it has an important role in defining anatomic abnormalities that predispose patients to recurrent and chronic sinusitis.
Approach to the Patient
It seems reasonable to consider the diagnosis of ABRS in patients who have had at least seven days of symptoms with two or more of the key signs and symptoms identified in the CDC guideline,3 the Williams rule, or the Berg rule (Tables 5 and6).24,29 This diagnosis also should be considered in patients who have worsening symptoms after five to seven days and those with severe symptoms regardless of duration.3 Patients without severe symptoms who have had symptoms for fewer than seven days are unlikely to have ABRS. They should be treated symptomatically for viral URI and should not be given antibiotics.