Am Fam Physician. 2006;73(5):810-816
This is part I of a two-part article on finger injuries. Part II, “Fractures, Dislocations, and Thumb Injuries” appears in this issue of AFP.
Related article: Common Finger Fractures and Dislocations
Patient information: See related handout on mallet finger, written by the authors of this article.
Author disclosure: Nothing to disclose.
Improper diagnosis and treatment of finger injuries can cause deformity and dysfunction over time. A basic understanding of the complex anatomy of the finger and of common tendon and ligament injury mechanisms can help physicians properly diagnose and treat finger injuries. Evaluation includes a general musculoskeletal examination as well as radiography (oblique, anteroposterior, and true lateral views). Splinting and taping are effective treatments for tendon and ligament injuries. Treatment should restrict the motion of injured structures while allowing uninjured joints to remain mobile. Although family physicians are usually the first to evaluate patients with finger injuries, it is important to recognize when a referral is needed to ensure optimal outcomes.
The severity of acute finger injuries is often underestimated, which can lead to improper treatment. Basic knowledge of the anatomy of the finger and a thorough evaluation of the patient can ensure proper diagnosis and treatment. Part I of this two-part article focuses on common tendon and ligament injuries of the finger. Part II1 discusses common finger fractures, dislocations, and thumb injuries.
Family physicians can manage most finger injuries; however, knowledge of referral criteria is important to ensure optimal outcomes. Treatment should restrict the motion of injured structures while allowing uninjured joints to remain mobile. Patients should be counseled that it is not unusual for an injured digit to remain swollen for some time and that permanent deformity is possible, even after treatment. Table 1 summarizes the evaluation and treatment of common ligament and tendon injuries.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Patients with finger injuries should receive a minimum of anteroposterior, true lateral, and oblique radiographic views. | C | 5 |
| Patient compliance should be monitored when treating mallet finger with splinting, because it is imperative for successful outcomes. All splints for mallet finger achieve similar results. | B | 15 |
| Patients with confirmed or suspected jersey finger should be referred to an orthopedic or hand surgeon. | C | 18 |
| A low threshold for referral should exist for collateral ligament injuries in children, because the growth plate often is involved. | C | 7,11 |
| Injury | Examination | Treatment | Referral criteria |
|---|---|---|---|
| Central slip extensor tendon injury (may cause a boutonniére deformity over time) | Tender at dorsal aspect of the PIP joint (middle phalanx) | Splint the PIP joint in full extension for six weeks. | Avulsion fracture involving more than 30 percent of the joint or inability to achieve full passive extension |
| Inability to actively extend the PIP joint | |||
| Collateral ligament injury (usually at the PIP joint) | Maximal tenderness at involved collateral ligament | Stable joint: buddy tape for two to four weeks. Do not leave fifth digit exposed if ring finger is taped. | Unstable joint or injury in a child |
| Test stability of joint while the finger is in 30 degrees of flexion and the MCP joint is flexed. | |||
| Extensor tendon injury at the DIP joint (mallet finger) | Tender at dorsal aspect of the DIP joint | Splint the DIP joint continuously for six weeks. | Avulsion fracture involving more than 30 percent of the joint or inability to achieve full passive extension |
| No active extension of the DIP joint | |||
| FDP tendon injury (jersey finger) | Tender at volar aspect of the DIP joint | Splint finger and refer to orthopedic or hand surgeon. | All |
| Inability to flex the DIP joint | |||
| DIP joint should be isolated during the examination. | |||
| Volar plate injury (usually at the PIP joint) | Maximal tenderness at the volar aspect of involved joint | Splint at 30 degrees of flexion and progressively increase extension for two to four weeks.Buddy tape at the joint if injury is less severe. | Unstable joints or large avulsion fragments |
| Test for full flexion and extension as well as collateral ligament stability. |
Basic Anatomy of the Finger
The anatomy of the finger is complex, but a basic knowledge is necessary to properly treat acute injuries. The index, middle, ring, and fifth digits have proximal, middle, and distal phalanges and three hinged joints: distal interphalangeal (DIP), proximal interphalangeal (PIP), and metacarpophalangeal (MCP). The thumb has a distal and proximal phalanx as well as an interphalangeal and MCP joint. The joints sit in volar plates (collateral ligaments attached to dense fibrous connective tissue), which provide joint stability.2,3
The dorsal extensor tendon divides into a central slip that extends the PIP joint and then into two lateral bands that extend the DIP joint. The volar tendons include the flexor digitorum superficialis and the flexor digitorum profundus. The flexor digitorum superficialis tendon attaches to the base of the middle phalanx and flexes the PIP joint. The flexor digitorum profundus tendon is located under and splits the flexor digitorum superficialis tendon. It attaches to the base of the distal phalanx and flexes the DIP.4 Figure 1 illustrates the basic anatomy of the finger, including joints, ligaments, and tendons.
Evaluation
Neurovascular and active flexion/extension testing will reveal clues to tendon and ligament injuries as well as subtle rotational abnormalities. The neurovascular evaluation should include two-point discrimination and capillary refill assessments. The physician should evaluate active flexion and extension by asking the patient to open and close his or her fist.
Clinical examination alone cannot diagnose fractures, and treatment protocols depend on radiography results. Patients with finger injuries should receive oblique, anteroposterior, and true lateral radiographic views.5 True lateral radiography is the most effective way to examine anatomic joint congruity.6,7 Ultrasonography is emerging as an effective tool to evaluate soft tissue structures.8
The evaluation of finger injuries during an athletic event differs from an evaluation in the office. The primary goal on the field is to detect neurovascular compromise and determine if the athlete can safely continue participation. All on-field evaluations must be readdressed in the office for a more thorough examination including radiography. Failure to do so increases the risk of future dysfunction.
Common Injuries
Several techniques may be used to diagnose common ligament and tendon injuries. Most injuries require splinting and follow-up to evaluate the healing process.
EXTENSOR TENDON INJURY AT THE DIP JOINT
Injury to the extensor tendon at the DIP joint, also known as mallet finger (Figure 2), is the most common closed tendon injury of the finger. Mallet finger usually is caused by an object (e.g., a ball) striking the finger, creating a forceful flexion of an extended DIP. The extensor tendon may be stretched, partially torn, or completely ruptured or separated by a distal phalanx avulsion fracture.9
Patients with mallet finger present with pain at the dorsal DIP joint; inability to actively extend the joint; and, often, with a characteristic flexion deformity. It is important to isolate the DIP joint during the evaluation to ensure extension is from the extensor tendon and not the central slip. The absence of full passive extension may indicate bony or soft tissue entrapment requiring surgical intervention.4,7,10 Bony avulsion fractures are present in one third of patients with mallet finger.11,12
If no avulsion fracture is present on radiographs, the DIP joint should be splinted in a neutral or slight hyper-extension position for six weeks13; the PIP joint should remain mobile. A Cochrane review14,15 confirmed that all available splints achieve similar results. Furthermore, the use of surgical wires (i.e., fixing the affected joint in a neutral position by drilling a wire through the DIP joint to the PIP joint) did not improve clinical outcomes.14,15 Figure 3 describes different types of splints.
Physicians should advise patients with mallet finger not to flex the DIP joint during treatment; the splinting period must restart every time flexion occurs. A Cochrane review15 showed that patient compliance is the most important factor in the success of splint treatments. The distal phalanx should be supported during splint changes.16 This is difficult to achieve alone, and the patient may need to return to the physician’s office for splint changes. Necrosis of the skin can occur if the DIP joint is overextended during splinting. If the skin blanches, the DIP joint is overextended. Allowing the skin to “breathe” for 10 to 20 minutes between splint changes minimizes the risk of maceration.
Patients may continue to participate in athletic events during the splinting period, and physicians should follow up with patients every two weeks to ensure compliance. After six weeks of splinting, the joint should be reexamined. If active extension is present, splinting can be limited to when the patient is sleeping and during athletic events for another six weeks.
Conservative treatment is successful for up to three months, even with delayed presentation.11 Referral criteria include bony avulsions involving over 30 percent of the joint space or the inability to achieve full passive extension. Despite proper treatment of mallet finger, permanent flexion of the fingertip is possible. The finger can become deformed if the injury is left untreated.17
FLEXOR DIGITORUM PROFUNDUS TENDON INJURY
Disruption of the flexor digitorum profundus tendon, also known as jersey finger (Figure 4), commonly occurs when an athlete’s finger catches on another player’s clothing, usually while playing a tackling sport such as football or rugby. The injury causes forced extension of the DIP joint during active flexion. The ring finger is the weakest finger and accounts for 75 percent of jersey finger cases.18 The injury can occur if the force is concentrated at the middle phalanx or at the distal phalanx.

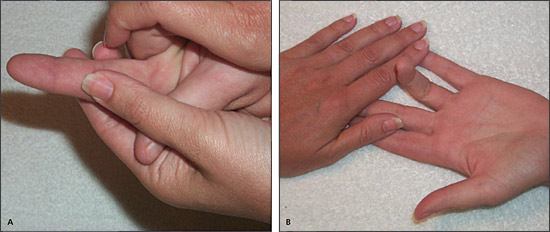
A patient with jersey finger may present with pain and swelling at the volar aspect of the DIP joint and the finger may be extended with the hand at rest. There may be a tender fullness if the tendon has been retracted. The digitorum profundus tendon should be evaluated by isolating the affected DIP joint (i.e., holding the affected finger’s MCP and PIP joints in extension while the other fingers are in flexion) and asking the patient to flex the DIP joint.18,19 If the digitorum profundus tendon is damaged, the joint will not move. The flexor digitorum superficialis tendon should be evaluated by holding the unaffected fingers in extension and asking the patient to flex the injured finger.19 An injured flexor digitorum superficialis tendon will produce no movement. Figure 5 illustrates these techniques.
CENTRAL SLIP EXTENSOR TENDON INJURY
Central slip extensor tendon injury occurs when the PIP joint is forcibly flexed while actively extended; it is a common injury in basketball players. Volar dislocation of the PIP joint also can cause central slip ruptures.21
The PIP joint should be evaluated by holding the joint in a position of 15 to 30 degrees of flexion. If the PIP joint is injured, the patient will be unable to actively extend the joint; however, passive extension should be possible. Tenderness over the dorsal aspect of the middle phalanx will be present. A delay in proper treatment may cause a boutonnière deformity (flexion of the PIP joint coupled with hyperextension of the DIP and MCP joints) (Figure 6). A boutonnière deformity usually develops over several weeks as the intact lateral bands of the extensor tendon slip inferiorly. Occasionally, boutonnière deformities occur acutely.
The PIP joint should be splinted in full extension for six weeks if there is no avulsion or if the avulsion involves less than one third of the joint. All available splints (Figure 3) can be used to treat PIP injuries, except for the stack splint, which is used only for DIP injuries. As with mallet finger, extension of the PIP joint must be maintained continuously. If full passive extension is not possible, the physician should refer the patient to an orthopedic or hand surgeon.
Patients with PIP joint injuries may continue to participate in athletic events during the splinting period, although some sports are difficult to play with a fully-extended PIP joint. Splinting duration is the same as with mallet finger.
COLLATERAL LIGAMENT INJURIES
Forced ulnar or radial deviation at any of the interphalangeal joints can cause partial or complete collateral ligament tears. The PIP joint usually is involved in collateral ligament injuries, which are commonly classified as “jammed fingers.”
Collateral ligament injuries present as pain located only at the affected ligament. The injury should be evaluated by applying valgus or varus stress to the involved joint in 30 degrees of flexion while the MCP joint is flexed at 90 degrees; an extended MCP joint will tighten the collateral ligaments, inhibiting the evaluation. The physician should compare the laxity of the injured finger with an unaffected finger. Radiography may demonstrate an avulsion fracture at the ligamentous insertion point.
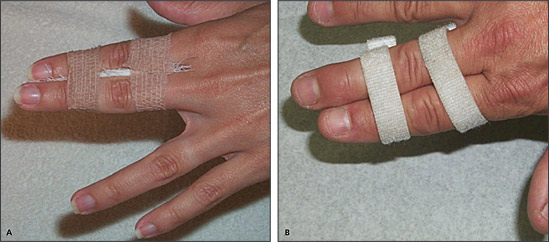
If the joints are stable and no large fracture fragments are present, the injury can be treated with buddy taping (i.e., taping the injured finger, above and below the joint, to an adjacent finger) (Figure 7). If the ring finger is involved, it should be secured to the fifth digit, because the fifth digit is naturally extended and easily injured if exposed.
Patients with collateral ligament injuries may continue participating in athletic events as symptoms allow. If joints are unstable with active ranges of motion, patients should be referred to an orthopedic or hand surgeon. A low threshold for referral should exist for collateral ligament injuries in children, because the growth plate often is involved.7,11
VOLAR PLATE INJURY
Hyperextension of a finger joint, such as a dorsal dislocation, can injure the volar plate (Figure 8). The PIP joint usually is affected, and collateral ligament damage often is present. The volar plate can be partially or completely torn, with or without an avulsion fracture.11 The subsequent loss of joint stability may allow the extensor tendon to gradually pull the joint into hyperextension, causing deformity.
Maximal tenderness will be located at the volar aspect of the affected joint. Full extension and flexion will be possible if the joint is stable. The collateral ligaments should be tested as with collateral ligament injuries. Radiographs may show an avulsion fragment at the base of the involved phalanx.
A stable joint without a large avulsion fragment should be splinted with a progressive extension splint (“block splint”) (Figure 9) starting at 30 degrees of flexion7,22 for two to four weeks, depending on injury severity; buddy taping should follow. Increasing the extension of a dorsal aluminum splint weekly will progressively increase range of motion.22 In less severe injuries, the injured joint should be buddy taped. This will restrict some extension and provide support. These two techniques may allow a patient to continue participating in athletic events sooner; however, participation depends on the athlete’s sport and position; it is difficult to play some sports with a flexed PIP joint. Referral criteria include an unstable joint or a large avulsion fragment.