
Am Fam Physician. 2007;76(9):1314-1322
A more recent article on pet-related infections is available.
Author disclosure: Nothing to disclose.
Human contact with cats, dogs, and other pets results in several million infections each year in the United States, ranging from self-limited skin conditions to life-threatening systemic illnesses. Toxoplasmosis is one of the most common pet-related parasitic infections. Although toxoplasmosis is usually asymptomatic or mild, it may cause serious congenital infection if a woman is exposed during pregnancy, particularly in the first trimester. Common pet-borne fungal infections include tinea corporis/capitis (ringworm); campylobacteriosis and salmonellosis are among the most common bacterial infections associated with pet ownership. Less commonly, pets can transmit arthropod-borne and viral illnesses (e.g., scabies, rabies). Infection in a pet can provide sentinel warning of local vectors and endemic conditions, such as Lyme disease risk. Treatment is infection-specific, although many infections are self-limited. Prevention involves common sense measures such as adequate hand washing, proper disposal of animal waste, and ensuring that infected animals are diagnosed and treated. Special precautions are indicated for immunocompromised persons. Increased communication between primary care physicians and veterinarians could improve treatment and prevention of these conditions.
Most human infectious diseases are zoonotic in origin; consequently, many infections can pass between pets and people. The scope of the problem is not well understood because many zoonotic diseases are underdiagnosed or not reportable to health authorities. A 1987 study estimated that approximately 4 million pet-derived infections occur annually in the United States with direct medical costs in excess of $300 million.1 Since then, the pet population has continued to increase.
More than 50 percent of U.S. households have at least one pet. The American Veterinary Medical Association estimates that between 1996 and 2001 the U.S. population of dogs and cats grew by 16 percent to 62 million dogs and 68 million cats.2 The booming international trade in exotic pets led to an outbreak of monkeypox traced to imported African rodents. The encroachment of suburbs into formerly rural areas has increased contact between domestic pets and wildlife pathogens.
At the same time, survey results have suggested that many physicians are uncomfortable advising patients about the health risks of animal contact.3 Because most pet-associated infections are preventable with simple measures, greater awareness on the part of family physicians could help reduce the impact of these conditions.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Wash hands after handling pets and avoid contact with pet feces. | C | 42 |
| High-risk persons* should avoid contact with reptiles (i.e., turtles, lizards, and snakes), baby chicks and ducklings, puppies and kittens younger than six months, and pets with diarrhea. | C | 42,43 |
| High-risk persons* should exercise caution at petting zoos and farms. | C | 42,43 |
| Pregnant women should keep their cats indoors, should avoid handling cat litter, and should not feed cats uncooked meat. | C | 42 |
Specific Conditions
Table 1 outlines the key aspects of clinical presentation, diagnosis, and treatment of infections associated with domestic pets in the United States.4–16 Although the list is not exhaustive, it attempts to present the most common and clinically significant infections according to type of organism. Readers are advised to consult infectious-disease references for comprehensive information about treatment of particular conditions.6
| Disease | Route of infection | Signs and symptoms | Diagnosis | Primary treatment |
|---|---|---|---|---|
| Parasitic | ||||
| Toxoplasmosis | Ingestion of oocysts in soil/fomites, undercooked meat | Immunocompetent: asymptomatic or lymphadenopathy | Serology, biopsy | Pregnancy: spiramycin (investigational in United States) Chorioretinitis: pyrimethamine (Daraprim) plus sulfadiazine plus leucovorin plus prednisone4 |
| Congenital: congenital defects | ||||
| Immunocompromised: febrile syndrome, meningitis | ||||
| Visceral larva migrans | Ingestion (usually by a child) of Toxocara spp. eggs in soil or feces | Eosinophilia, cough, wheezing, fever, seizures, hepatosplenomegaly | Eosinophilia, elevated WBC count, ELISA | Albendazole (Albenza)5 |
| Ocular larva migrans | Ingestion (usually by a child) of Toxocara spp. eggs in soil or feces | Endophthalmitis, choroidal granuloma | Eosinophilia, slit lamp, eosinophils in aqueous humor | Steroids5 |
| Cutaneous larva migrans | Skin contact with soil | Serpiginous rash, itching | Typical lesion, biopsy | Ivermectin (Stromectol)6 |
| Cystic echinococcosis | Ingestion of animal feces containing Echinococcus eggs | Cysts in liver or lungs, symptoms if rupture, mass effect | CT, ultrasonography | Percutaneous aspiration, saline injection, and re-aspiration6; albendazole |
| Alveolar echinococcosis | Ingestion of animal feces containing Echinococcus eggs | Cysts in liver, jaundice, pain | CT, ultrasonography | Surgical resection6; albendazole |
| Dipylidiasis | Ingestion of infected fleas | Often asymptomatic, anal itching, abdominal pain | Eosinophilia, stool ova and parasites examination for proglottids | Praziquantel (Biltricide)6 |
| Cryptosporidiosis | Contact with infected pet feces (e.g., dog, cat, ferret, rodent) | Diarrhea | Stool studies | Nitazoxanide (Alinia)6 |
| Giardiasis | Contact with infected pet feces (e.g., dog, cat, ferret, rodent) | Diarrhea | Stool studies, string test, endoscopy | Tinidazole (Tindamax), nitazoxanide6 |
| Fungal | ||||
| Tinea corporis/capitis | Physical contact/petting | Erythematous plaques, alopecia | KOH prep | Topical or oral antifungal7,8 |
| Bacterial | ||||
| Campylobacteriosis | Ingestion through contact | Diarrhea, fever | Stool WBC count, culture | Azithromycin (Zithromax)7 |
| Salmonellosis | Ingestion through contact | Diarrhea, fever, septicemia | Stool WBC count, culture | If asymptomatic or mild, antimicrobial not indicated Ciprofloxacin (Cipro)7 |
| Pasteurellosis | Bites, scratches | Wound infection | Culture | Amoxicillin/clavulanic acid (Augmentin)7 |
| Cat-scratch disease | Scratch or bite | Swelling at site of skin lesion, lymphadenopathy | IFA serology, biopsy | Azithromycin7 |
| Psittacosis | Inhalation of bird droppings or nasal secretions | Influenza-like illness, atypical pneumonia | Serology | Doxycycline (Vibramycin), erythromycin7 |
| Brucellosis | Contact with infected dogs | Fever, weight loss, adenopathy, splenomegaly | Blood culture, ELISA | Doxycycline plus gentamicin (Garamycin; brand not available in the United States) or streptomycin9 |
| Leptospirosis | Contact with urine or secretions (usually dog) | Influenza-like illness, conjunctival suffusion, fever, jaundice | Serology | Penicillin G, doxycycline, ceftriaxone (Rocephin)7,10 |
| Methicillin-resistant Staphylococcus aureus | Contact with infected animal | Colonization, soft tissue infection, pneumonia | Gram stain, culture | Treatment based on sensitivity testing |
| Lyme disease | Ticks from pet | Erythema chronicum migrans rash, fever, headache, arthritis, carditis | Western blot test | Early: doxycycline, amoxicillin, cefuroxime (Ceftin)11 |
| Plague | Contact with infected cats | Fever, myalgia, lymphadenopathy | ELISA, culture | Gentamicin, streptomycin12 |
| Tularemia | Ticks, contact with infected cats | Influenza-like illness, lymphadenopathy, pneumonia | ELISA | Gentamicin13 |
| Fish tank granuloma | Contact with fish aquarium | Localized granuloma | Biopsy, culture | Clarithromycin (Biaxin), minocycline (Minocin), doxycycline, TMP/SMX (Bactrim, Septra), rifampin (Rifadin) plus ethambutol (Myambutol), surgical excision14 |
| Arthropod | ||||
| Scabies | Contact | Itching, papular rash | Skin scraping | Permethrin (Acticin), ivermectin7,15 |
| Viral | ||||
| Rabies | Bites, scratches | Encephalitis | Biopsy | Vaccine prophylaxis; case report of survival with induction of coma and other treatment16 |
| Lymphocytic choriomeningitis | Petting, kissing animal (e.g., guinea pigs, other rodents) | Influenza-like illness, severe disease in immunocompromised persons | Serology | No specific antiviral therapy |
| Monkeypox | Direct contact with infected rodents | Fever, headache, cough, adenopathy, vesicular papular rash | Virus isolation, PCR | No proven antiviral therapy7 |
PARASITIC INFECTIONS
Toxoplasmosis
Toxoplasmosis, caused by the protozoa Toxoplasma gondii, is one of the most common zoonoses. The parasite undergoes sexual reproduction in cats and is excreted as an unsporulated oocyst. After two to three days, the oocysts develop spores that are infective.
Risk factors for toxoplasmosis include direct contact with cat feces (e.g., cleaning the litter box, gardening in feces-contaminated soil), and consumption of undercooked meat.17 Dogs have been implicated as mechanical vectors of toxoplasmosis because of their inclination for rolling in feces and carcasses.
Toxoplasmosis in adults is usually asymptomatic, but patients may develop cervical lymphadenopathy and a mononucleosis-like illness that is generally self-limited. Rarely, acute infection in pregnant women, especially during the first trimester, can cause serious congenital infection. It can also cause severe disease in immunocompromised persons.
Toxocariasis
Roundworm infection (toxocariasis) caused by the ascarid Toxocara canis (dogs) and Toxocara cati (cats) is one of the most common zoonotic infections associated with dogs and cats.18 Young children become infected by ingesting soil contaminated with animal feces that contains parasite eggs in areas such as playgrounds and sandboxes.19 Because of transplacental and trans-mammary animal transmission, many puppies are born infected and pose a particular risk. Most human infection is asymptomatic, in part because the larvae cannot complete their life cycle in humans. Eosinophilia is common. Rarely, the parasite migrates to the liver or lungs (visceral larva migrans) or to the eyes (ocular larva migrans). The annual U.S. incidence of visceral larva migrans has been estimated at 10,000 cases, whereas the annual incidence of ocular larva migrans has been estimated at 700 cases.
Cutaneous Larva Migrans
Cutaneous larva migrans is a common condition caused by dog and cat hookworms (Ancylostoma spp.). Fecal matter deposited on soil or sand may contain hookworm eggs that hatch and release larvae that are infective if they penetrate skin. Walking barefoot on contaminated beaches or park land can lead to infection. Although the larvae cannot reproduce in a human host, a pruritic papule forms at the site of infection, followed by an erythematous, serpiginous “track” that advances as the larvae migrate in the skin (Figure 1), with itching that is worse at night.

Echinococcosis
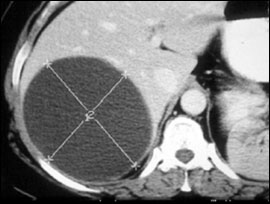
Echinococcosis (hydatid disease) is caused by the cestodes (tapeworms) Echinococcus granulosus and Echinococcus multilocularis. Dogs and other canids are the definitive hosts for E. granulosus and may become infected by eating the viscera of animals such as sheep or rabbits infected with the cysts. Humans may become infected by ingesting eggs shed in dog feces. Most of the cases in the United States occur in specific risk groups such as sheep farmers, Native Americans, and immigrants.20 After years of silent infection, enlarging cysts in the liver or lung (Figure 2) may cause symptoms including abdominal pain and chest pain and in some cases can affect other areas of the body such as the brain, bones, and heart.
E. multilocularis causes alveolar echinococcosis, which primarily affects the liver, can be confused with hepatic carcinoma, and has a higher case-fatality rate than cystic echinococcosis. Although the risk of human exposure to E. multilocularis is considered to be less than for E. granulosus, cats and dogs may serve as hosts, and there is concern that increases in infected fox and rodent populations in urban areas could lead to greater emergence of E. multilocularis infection in pets and their owners.21
Dipylidium Caninum
A more common tapeworm infection in cats and dogs is Dipylidium caninum. Fleas are intermediate hosts, and humans, especially children, can become infected by ingesting infected fleas. Fortunately, human infections are usually mild or asymptomatic and are believed to occur only sporadically.
Other Parasitic Infections
Cats and dogs, as well as ferrets, rodents, and other animals kept as pets, may be carriers of the intestinal parasites Cryptosporidium spp. and Giardia lamblia. Although cases of pet-to-human transmission have been reported, the frequency with which such transmission occurs is unknown.
FUNGAL INFECTIONS
After parasitic infections, fungal skin infections (cutaneous dermatophytosis, or ringworm) from contact with cats and dogs are probably the most common pet-associated diseases, causing an estimated 2 million or more infections each year.1 Cats may be more infectious than dogs, and even asymptomatic animals may transmit infection.
BACTERIAL INFECTIONS
Campylobacteriosis and Salmonellosis
Perhaps the most common bacterial infections associated with pet ownership are campylobacteriosis and salmonellosis. Many animals, including cats and dogs, are carriers of Campylobacter spp., and transmission between pets and humans (presumably through fecal-oral contact) has been estimated to cause more than 200,000 cases of gastroenteritis per year.1 Salmonella is also common in cats, dogs, chicks, ducklings, and reptiles, such as turtles and iguanas. Serious human salmonella infection from pets is a significant public health problem, particularly in children.22 Recent outbreaks of multi-drug-resistant salmonella have been traced to infected pet food derived from animal sources, as well as contact with pet rodents.23
Cat-Scratch Disease
Exposure to young cats or cats with fleas is a risk factor for infection with Bartonella henselae, the cause of cat-scratch disease. Although cat-scratch disease was originally thought to be a children's disease, almost one half of cases are now believed to occur in persons older than 20 years.24 The clinical manifestations of infection are an inoculation lesion at the point of injury and inflammation of nearby lymph nodes several weeks later (Figure 3). Complications of infection in immunocompromised persons include bacillary angiomatosis and Parinaud's oculoglandular syndrome.
Leptospirosis
Leptospirosis is one of the most common zoonotic diseases in the world, and Leptospira spp. are carried by a variety of wildlife and domestic animals. In the United States, the disease remains uncommon, but it may be increasing in incidence.25 Dogs appear to be infected more often than cats. Humans can become infected through contact with contaminated urine or other body fluids (except saliva), water, and soil. Human infection is usually asymptomatic or a mild influenza-like illness, but in some cases it can produce high fever, severe headache, hepatitis, conjunctival suffusion (dilation of blood vessels without inflammation), abdominal pain, diarrhea, rash and, in severe cases, renal failure, heart failure, and death.
MRSA
Patients infected with methicillin-resistant Staphylococcus aureus (MRSA) can pass the infection to their dogs, cats, or other pets through normal daily contact, leading to human reinfection despite appropriate therapy. Similarly, health care workers occupationally infected with MRSA may pass it back and forth with a household pet until all carriers have been identified and treated.26 Dogs that visit health care facilities have also been implicated in the cycle of MRSA infection.27
Lyme Disease
Dogs can act as mechanical vectors of Lyme disease (or other tick-borne illnesses) by bringing infected ticks from the outdoors into a house. Persons removing ticks from pets without protection may risk infection with the Lyme spirochete. In households where pets go outside, Lyme disease and other tick-borne diseases should be suspected even when affected persons report no outdoor activity.
Pasteurella
Pasteurella spp. colonizes in the oral cavity of cats and dogs, and human infection can result from close animal contact via biting, scratching, licking, and kissing.28 Cat bites have been reported to cause wound infection more often than dog bites.28 In rare cases, Pasteurella can cause serious systemic diseases such as pneumonia and peritonitis.
Psittacosis
Psittacosis, also known as parrot fever, is caused by Chlamydophila (formerly Chlamydia) psittaci. From 1988 through 2003, there were 935 human cases of psittacosis reported to the Centers for Disease Control and Prevention and most resulted from exposure to infected pet birds, usually cockatiels, parakeets, parrots, and macaws.29 Exposure to feces or nasal secretions of infected birds can result in human infection. Infection commonly presents as a mild influenza-like illness, so the diagnosis may be overlooked. Rarely, it can progress to a significant pneumonia that usually responds to doxycycline (Vibramycin) or macrolides.30
Brucellosis
Brucella canis, a dog pathogen, is considered to be a rare cause of human brucellosis (most human cases are caused by the organism Brucella abortus transmitted through consumption of unpasteurized dairy products or exposure to infected livestock). Brucellosis is characterized by a febrile syndrome that may progress to endocarditis. Recent reports suggest that blood tests for B. abortus may not detect B. canis infection, so the condition may be underdiagnosed.31
Mycobacterium Marinum Infection
“Fish tank granuloma,” caused by M. marinum, is mostly acquired from handling fish aquariums during cleaning or when changing the water. Although the typical infection is a localized granuloma of an upper extremity, M. marinum can cause disseminated disease in immunocompromised persons.32
Other Bacterial Infections
ARTHROPOD INFECTION
Several strains of the scabies mite, Sarcoptes scabiei, have adapted to specific host species. Dogs infected with S. scabiei canis may transmit the mite to humans. When such cross-species transmission occurs, the dog mite usually fails to reproduce and the infection may resolve spontaneously.
VIRAL INFECTIONS
Lymphocytic Choriomeningitis
Lymphocytic choriomeningitis is a virus that infects hamsters, guinea pigs, mice, and other rodents kept as pets. Human infection from contact with these rodents may be asymptomatic or result in an influenza-like illness with meningitis. There have been reports of fatal infection in organ transplant recipients exposed to pet rodents.35
Rabies
Rabies is a fatal zoonotic disease that is rare in the United States. Because of routine vaccination of dogs and cats, most human cases are currently caused by wildlife rather than pet exposure. Despite the rarity of human infection, almost 40,000 postexposure prophylactic treatments are administered yearly following animal bites, with significant associated medical costs.36
Monkeypox
In 2003, an outbreak of monkeypox in the Midwest was traced to contact with infected prairie dogs sold as pets.37 The prairie dogs had acquired the virus from imported African rodents housed in the same pet stores. The occurrence was a reminder of the potential for the international trade in exotic pets to introduce emerging pathogens.
Animals as Sentinels of Human Infection Risk
Although pets may function as vectors for various infectious agents, there is evidence that an illness diagnosed in a pet can be a “sentinel event,” warning the owners that they too may be at increased risk of infection. For example, because of their greater exposure to outdoor environments and heightened susceptibility to infection relative to humans, dogs have been proposed as sentinels for human Lyme disease risk.38 House cats have become infected with avian influenza virus through contact with infected birds,39 indicating their potential to detect avian influenza risk in the environment.
Diagnosis, Treatment, and Prevention
To diagnose most pet-related infections, the physician must have an index of suspicion for zoonotic disease and routinely ask patients about the presence and health of pets in the household. Adequate care often involves treating both affected humans and pets, and may require coordination of care and communication between physicians and veterinarians.40,41
Routine veterinary care of pets can reduce the chance of zoonotic disease in their owners. Physicians can help educate patients who own pets about preventive steps to further minimize the risk of pet-associated infections. Although few studies have assessed the effectiveness of such measures, specific prevention guidelines involve common-sense measures, such as adequate handwashing, proper disposal of animal waste, and ensuring that infected animals are diagnosed and treated.42,43 To reduce the risk of toxoplasmosis, pregnant women should not change the litter box. Pregnant women should also avoid adopting or handling stray cats and should not feed cats undercooked meat. High-risk persons (i.e., immunocompromised patients, infants and children younger than five years, pregnant women, and older adults) should avoid reptiles, chicks, ducklings, young kittens and puppies, and animals with diarrhea. They should also exercise caution at farms and petting zoos.
Tick control using topical acaricides for dogs in tick-borne disease–endemic areas may reduce risk to dogs and their owners. Pet owners should avoid feeding dogs and cats raw meat to reduce transmission of pathogens. Empiric treatment with antibiotics should be considered in the management of pet bites, especially cat bites; bites to high-risk areas of the body, such as the face or hands; or in immunocompromised patients, although an evidence-based review has found a lack of supporting evidence for routine prophylaxis in dog and cat bites.44 Table 2 lists additional resources on pet-related infectious disease issues.
| Resource | Description |
|---|---|
| American Veterinary Medical Association Web site:http://www.avma.org/communications/brochures/animal_health.asp | Contains fact sheets on a number of topics, including toxoplasmosis and tick control |
| Canary Database Web site:http://canarydatabase.org/ | Includes evidence about animals serving as “sentinels” of infectious diseases and other human health hazards |
| National Association of State Public Health Veterinarians Web site:http://www.cdc.gov/mmwr/PDF/rr/rr5605.pdf National Association of State Public Health Veterinarians. Compendium of measures to prevent disease associated with animals in public settings, 2007. MMWR Recomm Rep 2007;56(RR-5):1–14. | Provides information physicians can use to advise patients on preventive measures in public venues such as petting zoos |
| Healthy Pets Healthy People Web site:http://www.cdc.gov/healthypets/ | Maintained by the Centers for Disease Control and Prevention; provides information about specific pet diseases and prevention of human transmission |
The benefits of pet ownership, including positive effects on mental health, outweigh potential risks of infectious disease.45 The intimate relationship between humans and their pets appears to be bringing human and veterinary medicine into closer alignment.46 Recognizing the need for such collaboration, the American Medical Association adopted a “One Health” resolution in 2007, encouraging closer liaisons between health professionals who work with humans and those who work with animals. This could lead to improved understanding of pet-associated infections and enhance clinical efforts to detect and prevent them in humans and their animal companions.