
Am Fam Physician. 2010;81(1):42-47
Patient information: See related handout on LASIK, written by the author of this article.
Author disclosure: Nothing to disclose.
Surgical correction of vision is becoming increasingly popular. Laser-assisted in situ keratomileusis (LASIK) is the most popular method of corneal refractive surgery. LASIK is usually limited to adults who have stable refraction. Contraindications include the use of certain medications, conditions that impair healing, abnormal corneal anatomy, and inadequate tearing. Patients who cannot tolerate persistent eye dryness or who engage in activities with a risk of eye trauma should avoid LASIK. Possible complications include diffuse lamellar keratitis, epithelial ingrowth, and flap complications. Almost all patients achieve uncorrected visual acuity of at least 20/40, but higher degrees of pre-operative myopia may require a second operation. Long-term data on safety and stability are just becoming available. LASIK appears to be safe and effective, with only a small tendency for increased myopia in the first few years after surgery.
More than one half of all Americans require corrective lenses for clear vision.1 Since the development of radial keratotomy in the 1970s, corneal refractive surgery has become increasingly popular as a way to avoid the use of eyeglasses and contact lenses. Today, the most popular procedure in the United States for surgical vision correction is laser-assisted in situ keratomileusis (LASIK).2
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Appropriately selected candidates can achieve good vision with LASIK. | C | 14, 18, 21 | Proper patient selection is key to success; newer techniques have better outcomes. |
| Medications that contribute to dry eyes may make a patient unsuitable for LASIK. | C | 13, 15–18 | Dryness can be treated or medication changed. |
| Presbyopic patients may require reading glasses after LASIK. | C | 3 | Newer techniques may be appropriate to overcome this limitation. |
| Long-term effectiveness and safety of LASIK have not been established. | C | 12, 14, 19 | Earlier forms of corneal refractive surgery have been well tolerated and proven safe in the long term. |
Family physicians may be asked about photorefractive surgery by their patients and may be involved in the evaluation and management of ocular problems in LASIK-treated patients. This article describes the indications, benefits, and risks of LASIK surgery and gives an overview of the basic techniques, appropriate expectations for visual improvement, and evidence of the safety and reliability of the procedure. Potential complications, contraindications, and concerns about the procedure are also addressed.
Corneal Anatomy and Physiology
The corneal epithelium is about 400 to 500 microns thick and consists of four to six layers of stratified, nonkeratinizing squamous epithelial cells attached to a basement membrane. Below the basement membrane are the Bowman layer, stroma, Descemet membrane, and endothelium. The upper epithelial surface is covered with a tear film consisting of a glycocalyx produced by conjunctival goblet cells and lacrimal tears. Every seven to 10 days a complete cycle of cell migration occurs from the basal layer to the surface, with final apoptosis and desquamation. Injuries are re-epithelialized by migration and spreading of cells at the periphery of the injury plus migration and differentiation of stem cells from the limbus. Several conditions may interfere with proper corneal healing (Table 1).3
| Underlying cause | Examples |
|---|---|
| Conjunctival disease | Pemphigoid, radiation, Stevens-Johnson syndrome |
| Damaged cellular substrate | Herpes, chemical burns, diabetes mellitus, basement membrane damage or dystrophies |
| Dry eyes | Sicca syndromes, medication effect, insufficient tears |
| Eyelid abnormality | Entropion, ectropion, lagophthalmos, trichiasis |
| Keratopathy | Exposure, neurotrophic |
| Limbal stem cell damage | Burns, ischemia |
| Ophthalmic medication use | Vasoconstrictors, preservatives, anesthetics |
| Surface inflammation | Atopy, other inflammations |
Basics of Vision and Correction
The cornea and tear film perform about two thirds of refraction; the remainder is accomplished by the pupil and the lens. A perfect cornea is spherical, with a radius of about 8 mm. In many eyes, the cornea is not a perfect sphere. Surface cylinder-like distortions may develop in a specific direction, resulting in astigmatism. Additionally, the length of the eye affects where the image is focused. In patients with myopia (i.e., nearsightedness), the image focuses in front of the retina. In those with hyperopia (i.e., farsightedness), the image focus point is behind the retina.
Traditionally, vision is corrected using eyeglasses or contact lenses. Convex (“plus”) lenses correct for farsightedness, and concave (“minus”) lenses compensate for near-sightedness. Astigmatism is corrected by inserting a cylindrical shape into the visual axis. The resulting toroidal shape of the lens corrects the astigmatic distortion. In corneal refractive surgery, these corrections are made in the cornea itself, replacing the need for artificial lenses.
History
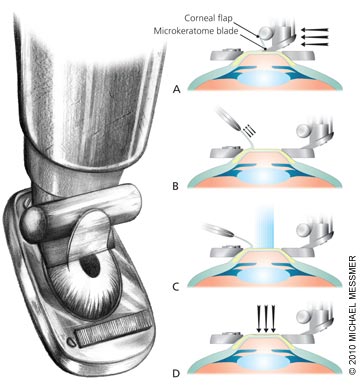
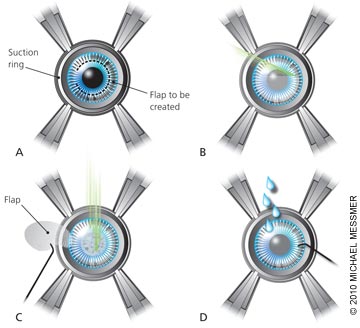
Refractive surgery includes LASIK, radial keratotomy, photorefractive keratectomy, intracorneal rings, and laser subepithelial keratomileusis (LASEK). Keratomileusis, or carving of the cornea, was first developed as a technique in which a disk of corneal tissue was removed, frozen, milled to the required shape, and sutured back into position. The laser was first used in humans in the early 1990s to reshape the cornea in situ under a flap cut by a microkeratome4 (Figure 1). A newer technique uses a femtosecond laser (the “all-laser” LASIK) instead of a microkeratome to create the flap (Figure 2). With refinement, LASIK has become the most popular method of refractive surgery in the United States, with about 1.4 million procedures performed annually.5
Contraindications
Eyesight may change in children and adolescents, and during pregnancy and lactation. LASIK is avoided during these times.
As techniques improve, several previously absolute contraindications to LASIK have been modified to relative contraindications (Table 2).3 Keratoconus, thin cornea, and previous radial keratotomy can cause problems with creating the flap and with healing, but patients with these conditions may be suitable for treatment with newer techniques and other forms of refractive surgery. Insufficient tears can affect corneal healing. Naturally or pathologically dry eyes, or the use of medications that can increase dryness are potential barriers to LASIK. Dryness sensation after LASIK is fairly common in normal eyes; anything that increases dryness may be unacceptable to patients. Extreme dryness, such as that in sicca syndromes, may cause intolerable dryness postoperatively.
| Contraindication | Concern |
|---|---|
| Abnormal wound healing (e.g., keloids) | Controversial; postoperative haze |
| Active corneal ulceration | Corneal breakdown |
| Autoimmune disease or inflammation (e.g., blepharitis) | Poor healing |
| Basement membrane dystrophy (relative) | May be treated first |
| Diabetes mellitus with reduced corneal sensation | Dryness from reduced sensation |
| Dry eyes, particularly sicca syndromes | Prolonged discomfort, visual effects |
| Herpes history | Laser may reactivate virus; LASIK may be considered if no recurrence for more than one year; antivirals should be used prophylactically |
| Keratoconus | May damage already weakened corneal tissue |
| Medication use: isotretinoin (formerly Accutane), amiodarone (Cordarone) | Excessively dry eyes |
| Relative contraindication: any medication that produces dryness (e.g., those with anticholinergic effects, sympathomimetics, clonidine [Catapres]) | |
| Patient younger than 18 years or unstable refraction | Refractive error may progress postoperatively |
| Pregnancy or lactation | Risk of myopic progression, corneal haze, and changes in tear layer; avoidance of fetal exposure to medications |
| Recurrent erosions | Poor healing |
| Thin cornea | Insufficient tissue after ablation, corneal breakdown (newer techniques have been developed that can address thinner corneas) |
| Thyroid orbitopathy | Excessively dry eyes |
Inflammation, collagen vascular diseases, and active ulceration are significant contraindications. Although concerns have been expressed that laser energy may reactivate herpetic infections, few data support this concern. Patients with a history of ocular herpes but no recurrences in the previous year may be acceptable candidates for LASIK and should receive preoperative oral antiviral therapy.
When microkeratomes are used in LASIK, the intraocular pressure is increased to more than 65 mm Hg to stabilize the globe and allow for an even thickness keratectomy. However, glaucoma is not a contraindication because the pressure increase is transient.
Surgery
Candidates for LASIK must be older than 18 years (except for children with specific medical indications) and have stable refraction for about one year. Preoperative evaluation includes slit-lamp examination; retinal evaluation; and refraction, including measurement of astigmatism. About 95 percent of eyes have clinically measurable astigmatism, and in 10 to 20 percent the astigmatism is greater than one diopter (D), causing unacceptable uncorrected visual acuity. Pre-operative consistency of refraction is important for long-term stability of the LASIK correction. Contact lenses must be discontinued before the preoperative assessment (three days for soft lenses, three weeks for hard lenses) to allow the cornea to stabilize.
Wavefront-guided LASIK is a refinement of classic refraction methods. Because the cylindrical aberration of many corneas is not uniform, applying an identical correction over the entire treated area may not give the optimal degree of correction. Wavefront-guided LASIK tailors the laser correction to the specific pattern of corneal refractive aberration in each patient. Studies suggest that wavefront-guided LASIK offers better uncorrected visual acuity than traditional methods.6,7 Most North American refractive surgeons perform wavefront-guided ablative corneal surgery.2
The surgeon must measure corneal thickness to determine if sufficient tissue is present for the procedure, because the quantity of tissue removed increases with the amount of correction needed. The treated area typically measures 6 mm in diameter. In low light, persons with naturally large pupils may exceed this diameter and have visual disturbances (e.g., halos, starbursts) as unfocused light interferes with focused light.
Recovery is quick for almost all patients, with minimal to no postoperative pain. Vision stabilizes over a few months but is almost at goal by two days after surgery. However, patients should be counseled about realistic expectations. LASIK can correct 0.5 to 12 D of myopia, 0.5 to 4 D of hyperopia, and up to 8 D of astigmatism. Although most patients no longer need to use eyeglasses after LASIK, a small percentage have a 0.5 D deviation from plano (i.e., no refractive error) and may drift during recovery to one or two lines' loss on the visual acuity chart. For patients who require more precise vision, this may not eliminate the need for eyeglasses. A second LASIK procedure might correct this error. Patients considering LASIK should inquire whether there is an additional charge for such procedures.
Patients with presbyopia may need to use reading glasses after LASIK, because myopia correction effectively increases the far-sightedness of presbyopia. Some patients may be candidates for monovision, in which the dominant eye is corrected for distant vision and the nondominant eye is corrected for near vision, resulting in anisometropia. Older patients are more tolerant of anisometropia.
Outcomes
Effectiveness of LASIK has improved with experience and newer equipment.8 When a scanning laser with eye tracker or a wavefront-guided laser is used, more than 80 percent of patients achieve vision within 0.5 D of the intended correction, and more than 95 percent achieve vision within 1 D (Table 3).8 Almost all patients achieve at least 20/40 uncorrected vision, and most have 20/20 uncorrected vision after LASIK.
| Measured visual acuity | Outcome achieved using scanning laser with eye tracker (%) | Outcome achieved with wavefront-guided laser (%) |
|---|---|---|
| 20/20 or better (uncorrected) | 78.6 | 89.2 |
| 20/40 or better (uncorrected) | 96.3 | 98.9 |
| Within 0.5 diopters of intended correction | 82.8 | 80.8 |
| Within 1 diopter of intended correction | 96.0 | 95.1 |
Persons whose jobs require precise vision may still require glasses or a second operation, and should consider the risk of persistent dryness or visual disturbances. Contact or high-impact sports increase the risk that the flap might become dislodged; these activities should be avoided, even though successful repair has been reported in many cases.9–11
Ten-year outcome data have recently become available for LASIK.12 The procedure seems to be safe and effective for patients with high degrees of myopia. There is a tendency for regression to myopia, and a substantial proportion of patients have had a second surgery to improve correction. For patients with high degrees of myopia, this may be preferable to using eyeglasses with thick lenses to correct vision.
LASIK is the most popular form of surgical vision correction, but other procedures may be appropriate for some patients. No flap is formed in photorefractive keratectomy; the epithelium is ablated directly by the laser. This may be more suitable for patients at risk of flap dislodgement. Epi-LASIK opens a thinner flap and may be more suitable for persons with thin corneas. Patients should be counseled about reasonable expectations and should work with the surgeon to find the most suitable approach to vision correction.
Complications
Dry eye symptoms are the most common adverse effects of LASIK (Table 4).4,6,13 About 20 to 40 percent of patients report this symptom six months after surgery.14 Preoperative dryness and female sex may confer higher risks,13 and some surgeons consider preoperative dry eye a relative contraindication. LASIK interrupts sensory fibers of the cornea, reducing the stimulus to tear production.15–17 Tear quantity is reduced and osmolarity is increased postoperatively, with improvement by about three months.18 Dry eyes may be treated with artificial tears, cyclosporine eye drops (Restasis), or punctal plugging, but treatment may not eliminate the symptoms. Tear adequacy can be measured during pre-operative evaluation, and any necessary and medically appropriate changes can be made to medications that can contribute to dry eyes.
| Complication | Frequency (%) |
|---|---|
| Dry eyes | 20 to 40 |
| Diffuse lamellar keratitis | 2 to 4 |
| Epithelial ingrowth | 1 to 3 |
| Flap wrinkles | 0.2 to 4 |
| Free cap | 0.1 to 1 |
| Infection (bacterial, fungal) | 0.1 to 0.1 |
Diffuse lamellar keratitis (i.e., “Sands of Sahara”) occurs in 2 to 4 percent of patients undergoing LASIK.19 Pain can be a symptom. Although this condition is usually noted within the first postoperative week, it has been reported later. The etiology is not clear, but involves epithelial disruption and may be a result of debris or another source of inflammation at the edge of the operative area, particularly if a postoperative epithelial defect is present. Diffuse lamellar keratitis is treated with topical or systemic steroids, depending on the degree. Sight-altering complications are very rare, but can occur.
Epithelial ingrowth occurs when epithelial cells get under the corneal flap. It is evident within weeks of LASIK, and occurs in about 1 to 3 percent of cases.14,20 This complication tends to be self-limited and regresses within weeks without lasting effects. Some cases require lifting the flap and irrigating or using laser energy to eliminate the ectopic cells.
Potential complications of LASIK include irregular flap, free cap (if the entire flap is accidentally removed), over- and under-correction of vision, poor centration of the correction zone, irregular astigmatism, contamination (e.g., blood, fibers, metal from the microkeratome, talc), and infection. Microkeratome-related complications can be avoided with the use of the newer femtosecond laser, which separates the corneal flap using laser energy rather than by cutting.21
When patients who have undergone LASIK present to their family physician with ocular problems, fluorescein staining may be done. Once healed, however, the keratome or laser injury no longer takes up stain. Trauma might result in flap dislodgement, which results in visual impairment. If LASIK was performed within the past month, an ophthalmologist should be consulted.
Cost
Prices vary by market region, technique (wavefront-guided versus standard, femtosecond laser versus microkeratome), and physician. Microkeratome-based procedures may start at approximately $1,600 per eye, and wavefront-guided femtosecond laser operations may cost $2,300 per eye.22 Inexpensive procedures may be restricted to a select few patients.
